Chronic kidney disease is a progressive disease closely associated with hypertension. In a large number of patients requiring renal replacement therapy, consistent blood pressure reduction could have prevented end-stage renal disease. This is because blood pressure medications not only protect against cardiovascular events, but also exhibit a kidney-protective effect.
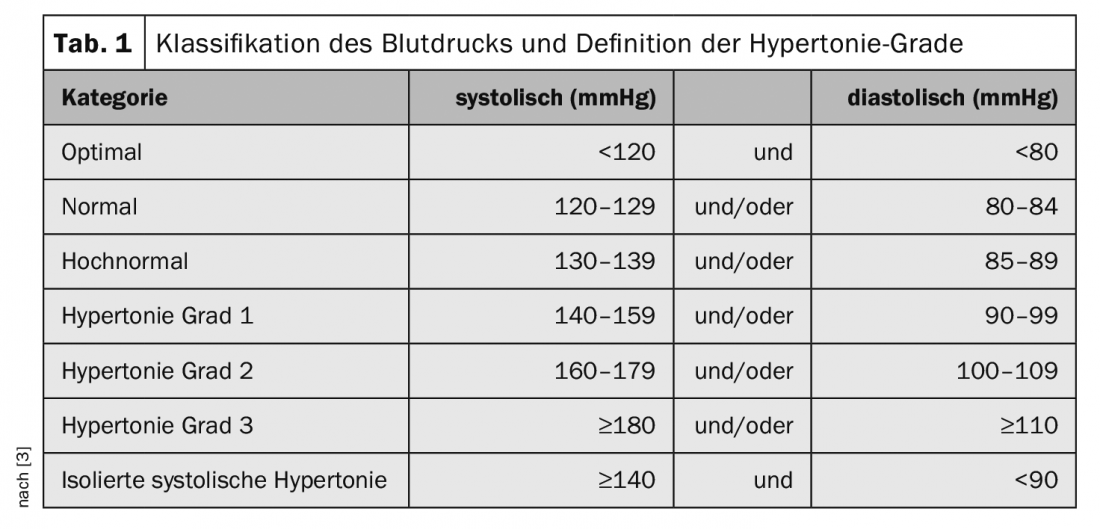
Hypertension is not uncommon – it is estimated that one in three people over the age of 50 and one in two people over the age of 60 suffer from high blood pressure. This is by no means an ailment, but a serious illness that can have serious consequences. As a rule, values of 140/90 mmHg should be aimed for (tab. 1). The kidney is involved in the regulation of blood pressure through hormone and urine production, among other things. If it suffers damage, this has corresponding effects. For example, renal insufficiency leads to fluid and pressure overload in the bloodstream. But vice versa, there is also an influence. People with hypertension have an increased risk of developing chronic kidney disease (CKD). First and foremost, high blood pressure is associated with damage to the blood vessels and thus with cardiovascular disease. The negative effects on the kidney, on the other hand, are less common. In the broadest sense, however, CKD can also be counted among vascular diseases. The filter units of the kidney are made up of thousands of tiny vessels. These are damaged and can no longer perform their function if the pressure is too high. Effective hypertension therapy is indicated to avoid renal failure and the subsequent need for renal replacement therapy.
Hypertension can make dialysis necessary
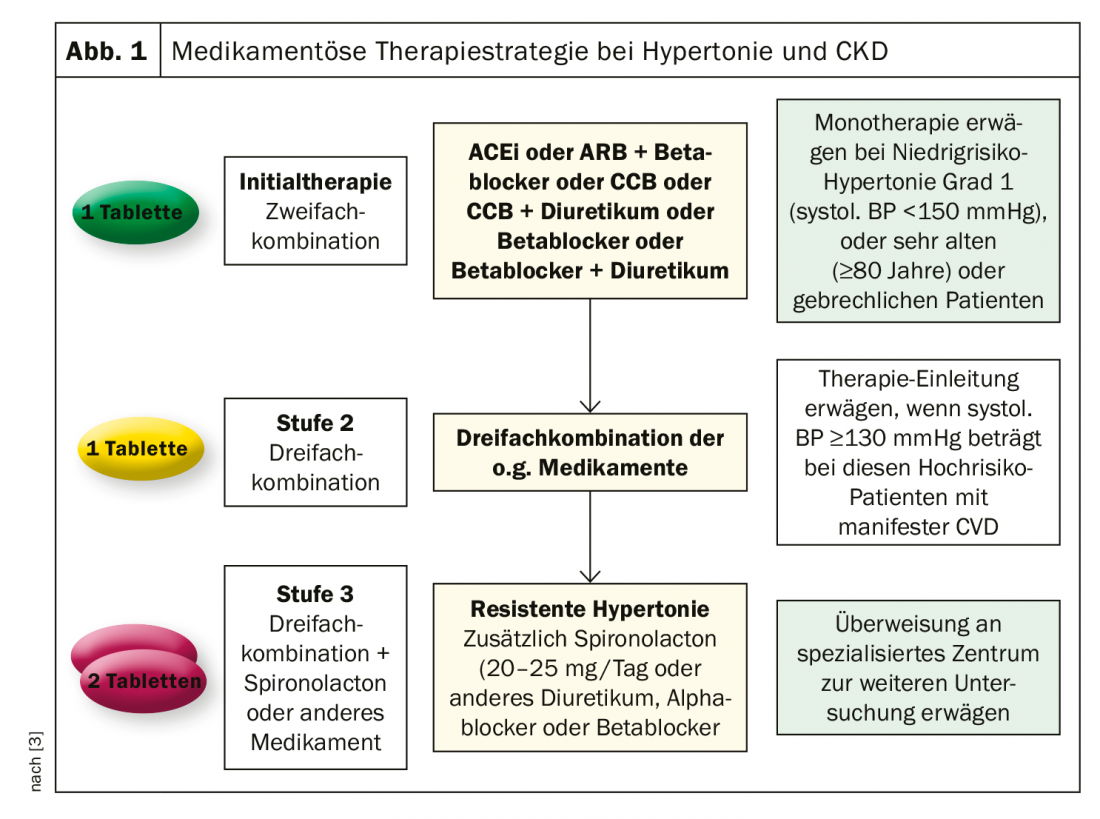
Hypertension is the second most common reason patients need dialysis. The number of dialysis patients who are dependent on blood washing due to hypertension-related damage to the kidneys is approximately 10-19% in Europe [1]. In Switzerland, approximately 4500 patients are currently dependent on renal replacement therapy [2]. Accordingly, effective blood pressure lowering would have saved approximately 850 patients from this step. However, countermeasures should be taken early in the event of hypertension. This is not easy in that many Swiss do not even know their blood pressure values. The new blood pressure guideline of the European Societies of Hypertension and Cardiology (ESH/ESC) advises antihypertensive medication from values of 140/90 mmHg [3]. Prior to this, lifestyle modification measures should be implemented to achieve the target value of 130/80 mmHg. These include, for example, limiting salt intake, limiting alcohol consumption, increasing vegetable intake, regulating body weight, and regular aerobic exercise. However, these values only apply to people with healthy kidneys. Patients with CKD should receive pharmacological intervention earlier (Fig. 1) . Results of a combined study showed that patients with intensive blood pressure lowering tend to have a lower incidence of needing dialysis [4]. Intensive blood pressure control is also associated with lower mortality.
Literature:
- https://era-edta-reg.org/files/annualreports/pdf/AnnRep2017.pdf (last call: 12.11.2019)
- www.swissnephrology.ch/media/srrqap/MedizinAktuell_2017_aktuelle_Erkenntnisse.pdf (last call: 12.11.2019)
- https://leitlinien.dgk.org/files/2019_Pocket_Leitlinie_Hypertonie_Version2018.pdf (last call: 12.11.2019)
- Ku E, Gassman J, Appel LJ, et al: BP Control and Long-Term Risk of ESRD and Mortality. J Am Soc Nephrol 2017; 28: 671-677.
CARDIOVASC 2019; 18(6): 22