Burnout and depression are two conditions that physicians are having to deal with more and more frequently. Not only with the patients, but above all with themselves. Public opinion and the ever-increasing quality criteria demand the professionally unassailable physician with the highest possible emotional competence. But the dream job can also turn out to be a nightmare – further exacerbated by the Corona pandemic.
It has been known for some time that physicians in particular are often overworked. The working conditions do not exactly contribute to a relaxed work-life balance. Medicine is therefore a profession that can make people ill. Currently even more than before, as a survey has shown. The reason is not solely that colleagues become infected with SARS-CoV-2. No, the work situation of many physicians has been exacerbated by the pandemic. One in two physicians say that their feelings of being overworked and in a bad mood have increased as a result of the crisis.
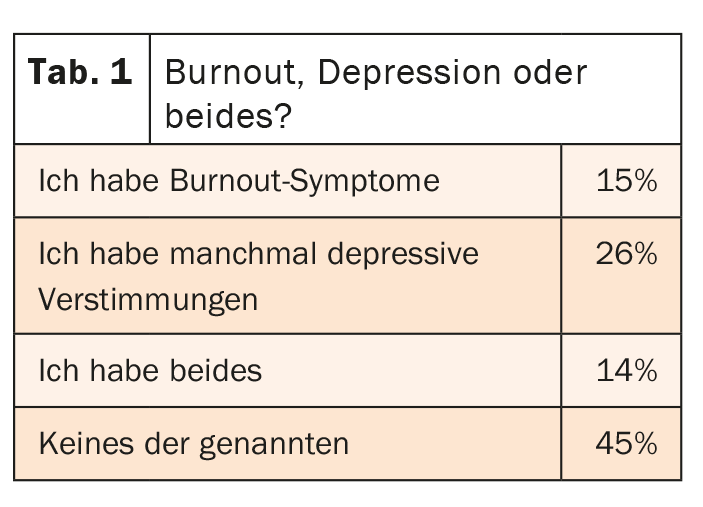
Burnout and/or depression are common among physicians anyway. Two years ago, 45% of respondents reported suffering from such symptoms. But this share rose by another 10 percentage points between June and August 2020 – with no improvement in sight. 26% of physicians state that they sometimes suffer from depressive moods, 15% have rather burnout symptoms and 14% have both (tab. 1). The boundaries between the clinical pictures are fluid. In total, this is 55% of respondents who do their job every day despite these pressures. The comments reflect how this overload manifests itself: highly functional at work, overstimulated at home, and emotionally inaccessible. In addition, many physicians suffer from sleep disorders, which further fuels exhaustion and nervous stress.
Root Cause Analysis
Above all, the work situation seems to be causal for the psychological stress of those affected. Especially in the hospital, work seems to get on the nerves: 67% said that the job contributes strongly or very strongly to depressive symptoms. Among colleagues in private practice, only 39% see it the same way. Above all, social isolation, fueled not only by the pandemic but also by an excessive workload, contributes to the poor mood. In addition, there is an excessive bureaucracy and an incapacitating administration. However, physicians also perceive the hopeless handover of their practice, the double burden of children and career, the “constant bombardment by politics and health insurers” and digitization as psychologically stressful. The limits of their workload are reached above all by the unloved duties of managing and documenting their work (44%) and overtime (42%). Physicians in private practice are also more stressed by legislative mandates – 46% compared to hospital employees at only 7%. Hospital physicians, on the other hand, feel more burdened because they spend too much time at work – 49% vs. 34% for physicians in private practice. The difference is even greater in the lack of recognition and respect from administration and employers, as well as from colleagues or employees: 55% in hospitals, 11% in private practices. Another classic that causes great pressure for physicians in hospital operations: when management pressures and profit maximization takes precedence over patient well-being (47% vs. 19%).
Stress trigger corona
The survey clearly shows that the psychological stress of physicians has continued to increase compared to previous years. Since the online questionnaire was completed shortly after the peak phase of the 1st Corona wave, participants were already able to take stock: One in two physicians stated that the pandemic had increased their feelings of burnout. 40% of colleagues could not see any worsening due to the crisis.
What could bring relief?
For each colleague, the problems are a bit different, so there can be no universal solution. When it comes to money, family physicians (56% vs. 28% of specialists) and general practitioners (52% vs. 19% for clinicians) are more likely to speak up. More than half of respondents would take pressure off better pay. Slimmed-down rules, for example, are also seen by family physicians in particular as a burnout antidote (60%). Stress with administration and within the team, on the other hand, is more of an issue for hospital physicians. They want more respect (52% versus 8% for established physicians) from their employers and colleagues. It would also help 41% if they didn’t have to constantly look at the money when treating their patients.
Doctor – the most difficult patient of all
Those who have already experienced burnout try to stabilize their psyche in different ways. Every fourth physician has reduced his working hours, 22% have organized work differently. Family physicians, in particular, often hire additional staff. However, doctors seem to have a hard time asking for help themselves. 66% of those affected have not yet sought help. Only 5% are currently looking and 6% are thinking about getting help from an expert. This is due, among other things, to the fact that 38% of respondents do not consider their symptoms serious enough – but also to the fact that one in three physicians is simply too busy to take care of themselves and their psyche. A vicious circle that must be broken!
Source: Medscape Report: Burnout and Depression in the Corona Crisis – What’s Stressing Physicians Mentally and How They Could Be Helped. 10.11.2020. Available at: https://deutsch.medscape.com/diashow/49000709
InFo NEUROLOGY & PSYCHIATRY 2020; 18(6): 44-45 (published 11/30/20, ahead of print).
CARDIOVASC 2020; 19(4): 39-40
InFo PNEUMOLOGY & ALLERGOLOGY 2021: 3(1): 17
DERMATOLOGY PRACTICE 2021; 31(2): 22












