Heart failure with reduced ejection fraction (HFrEF) is characterized by a left ventricular ejection fraction (LVEF) in the range ≤40% according to the current classification, whereas heart failure with preserved ejection fraction (HFpEF) is characterized by an LVEF in the range ≥50%. Therapeutically, this differentiation makes a big difference!
Heart failure (HF) is not a single diagnosis, but a clinical syndrome caused by the inability of the heart to meet the physiological demands of the body’s organs. This results in either systems of volume overload, such as dyspnea, ankle swelling, fatigue, and clinical signs of volume overload, or low cardiac output, or both, due to a structural and/or functional abnormality of the heart. Risk factors include a sedentary lifestyle, obesity, high blood pressure, smoking, excessive alcohol consumption, and dyslipidemia, diabetes, or coronary artery disease (CAD). Which are modifiable by lifestyle modification, optimal medical therapy for hypertension, diabetes and dyslipidemia, and preventive vaccinations.
High blood pressure is one of the leading risk factors
In particular, hypertension is among the leading risk factors for the development of HF. Two-thirds of all HF patients suffer from it, and up to 90% in patients with HFpEF. However, uncontrolled hypertension in patients treated with optimal medical HF therapy is rare because of the overlap between HF and antihypertensive medications. Optimal blood pressure targets are as yet unknown for both HFrEF and HFpEF, so individual targets are usually considered, taking into account age and concomitant diseases (diabetes, renal disease, CHD, valvular disease, stroke). Nevertheless, as a general rule, aim for evidence-based medication targets in HFrEF despite mild hypotension; conversely, avoid hypotension in HFpEF with left ventricular hypertrophy and limited preload reserve.
In addition, the diagnosis of heart failure requires the presence of symptoms and/or signs of HF, as well as objective evidence of cardiac dysfunction, such as shortness of breath, fatigue, and ankle swelling. If these are present, the following diagnostic tests are recommended for the evaluation of patients with suspected chronic HF: The electrocardiogram (ECG) may reveal abnormalities such as atrial fibrillation, Q waves, LV hypertrophy (LVH), and a widened QRS complex, which can increase the likelihood of a diagnosis of HF and also guide therapy. If available, measurement of natriuretic peptides (NP) is recommended. A plasma concentration of B-type natriuretic peptide (BNP) <35 pg/ml, N-terminal pro-B-type natriuretic peptide (NT-proBNP) <125 pg/ml, or mid-regional atrial natriuretic peptide (MR-proANP) <40 pmol/L68 make the diagnosis of HF unlikely. Basic investigations such as serum urea and electrolytes, creatinine, complete blood count, and liver and thyroid function tests are recommended to differentiate HF from other diseases, to provide prognostic information, and to guide potential therapy. Echocardiography is recommended as the most important examination to assess cardiac function. In addition to determining LVEF, echocardiography also provides information on other parameters such as chamber size, eccentric or concentric LVH, regional wall motion abnormalities (which may indicate underlying CAD, Takotsubo syndrome, or myocarditis), RV function, pulmonary hypertension, valve function, and markers of diastolic function.
Heart failure may occur regardless of LV ejection fraction
The causes of HF can vary, but ischemic cardiomyopathies are relatively common. Ischemic HF is caused by circulatory disturbances in the heart, for example as a result of CHD. Therefore, the crucial question in initial HF diagnosis is always whether previously unrecognized CHD is present. A noninvasive ischemia test, such as stress MRI, is often used to answer this question. It is a comprehensive method for assessing global and regional function, evaluating whether ischemia or myocardial infarction is already present, and characterizing tissue (myocardial edema, area at risk, ventricular thrombus, cardiomyopathy). Sensitivity to detect infarction is 94-99%; sensitivity to ischemia is 91%; and specificity to ischemia is 83%. If a positive or equivocal stress MRI is present, with evidence of relevant ischemia (≥10%) or ischemic HF patterns, the next step is invasive angiography. Whose result either confirms ischemic HF and necessitates percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass grafting (CABG), or demonstrates bystander CAD. If stress MRI is inconclusive, with limited ischemia (<10%), nachweislich kleinen Infarkten oder sehr jungen Patienten, sollte ein Kalzium-Score (Ca-Score) und eventuell eine computertomografische Koronarangiografie (CTCA) durchgeführt werden. Bei fortgeschrittener HF und einem Ca-Score=0, kann eine ischämische HF ausgeschlossen werden; bei einem Ca-Score>0, CTCA should also be performed to exclude or confirm stenotic CAD and ischemic HF. If positive, invasive angiography is again recommended. Whose result either confirms ischemic HF or demonstrates bystander CHD and necessitates the appropriate therapies.
Prognostic utility of classical HFrEF drugs.
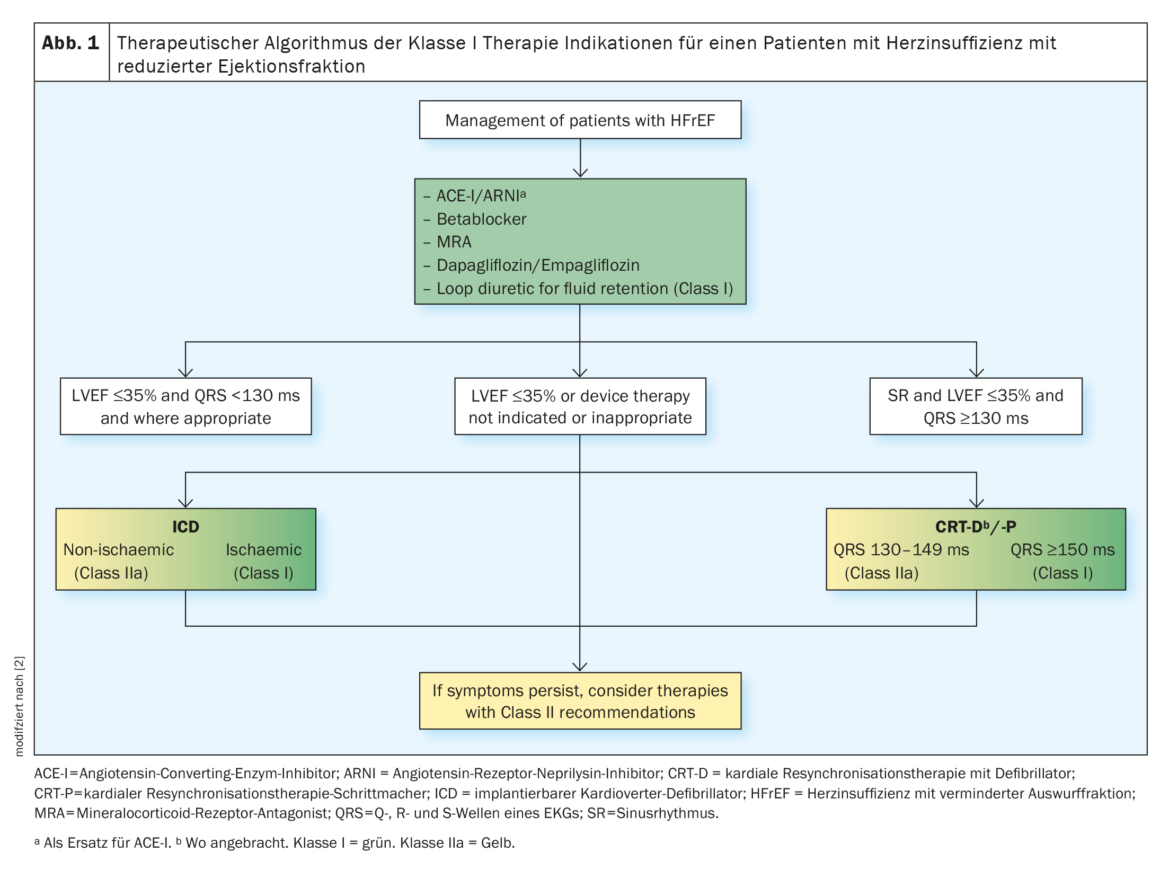
Currently, based on left ventricular ejection fraction, two main patient groups are distinguished: patients with impaired pumping function (≤40%) of the heart in whom systolic heart failure (HFrEF) is present and patients with heart failure with preserved pumping power (≥50%) of the heart (HFpEF). The differentiation makes a big difference therapeutically, because for patients with HFrEF, an arsenal of evidence-based therapeutic options to reduce morbidity and mortality has now been developed by clinical research. In particular, the so-called “Fantastic Four” (ARNI/ACE-I/ARB, BB, MRA, SGLT2-I) reduce morbidity and mortality within four weeks of starting treatment.
According to the European Society of Cardiology guidelines, common standard therapy for heart failure with reduced ejection fraction (HFrEF) initially includes the use of an angiotensin-converting enzyme (ACE) or angiotensin II receptor type 1 (AT1) inhibitor and a beta blocker (BB). If blood pressure is adequate and eGFR is ≥30 ml/min/m², the switch to sacubtril/valsartan may be made. ACE inhibitors or AT1 blockers must be discontinued prior to administration. To avoid angioedema, at least 36 hours should elapse between last ACE inhibitor administration and initiation of ARNI. In case of intolerance to ACE-I or ARNI, ARBS/Sartans may be used. Both RAAS-I, ARNI, and SGLT2-I can transiently decrease eGFR. A creatinine increase <50% and an eGFR decrease <10% from baseline is acceptable and renal function recovers. In particular, SGLT2-I have shown a survival benefit independent of diabetes status/HbA1c.
Patients with ischemic HF have a higher average risk of sudden cardiac death (SCD) than patients with nonischemic HF. In the presence of SCD risk factors such as NYHA** classification II-III and LVEF ≤35% despite ≥3 months of established optimal medical therapy and survival >1 year, there is an ICD# class I indication for patients with ischemic HF and a class IIa indication for all patients with nonischemic HF. Patients with NYHA classification IV who are refractory to pharmacologic therapy (survival <1 year) receive a Class III indication. Cardiac resynchronization therapy (CRT) is recommended for patients with symptomatic HF, an LVEF ≤35% despite optimal medical therapy, and left bundle branch block (LBBB) in sinus rhythm and a QRS duration ≥150 ms (Fig. 1) [2].
** NYHA = New York Heart Association
# ICD = Implantable Cardioverter Defibrillator
Preventive examinations and treatment of underlying diseases
In patients with HFpEF, prognosis-improving therapies are lacking despite many studies. To date, no treatment has been shown to reduce mortality and morbidity. In this case, the only remaining option is still the empirical attempt to alleviate the patients’ symptoms with (loop) diuretics and to achieve a switch to a healthy lifestyle. The lack of a common therapy makes screening and treatment of underlying diseases such as hypertension, diabetes, amyloidosis, CHD, and valvular disease all the more important in patients with HFpEF, explains PD Dr. Philip Haaf, cadre physician at University Hospital Basel [1]. The vast majority of HFpEF patients suffer from hypertension, and many also have underlying CHD. Things to look for include atrial fibrillation, diabetes, COPD, kidney disease, previous oncologic therapies, iron status, valvular heart disease, hypertrophic cardiomyopathy, and cardiac amyloidosis, Haaf added.
Too little iron is bad – but so is too much!
Cardiomyopathy due to iron overload occurs primarily in patients with primary or inherited hemochromatosis, secondary to multiple blood transfusions. Cardiac MRI can provide relief by quantifying iron levels in the heart and liver for diagnosis and monitoring of iron chelator therapy and phlebotomy. Even more significant than iron overload, however, is iron deficiency in heart failure. For patients with HF, iron deficiency is present with a ferritin <100 ng/ml or ferritin <300 ng/ml with a transferrin saturation (TSAT) <20%. Iron deficiency may present independently of anemia and affects 55% of patients with chronic HF and up to 80% of patients with acute HF. The exact cause of iron deficiency in HF remains unknown.
It is recommended that all patients with HF and Class I indications be regularly screened for anemia and iron deficiency by complete blood count, serum ferritin concentration, and TSAT. Intravenous iron supplementation with ferric carboxymaltose should be considered in symptomatic HF patients recently hospitalized for HF with LVEF ≤50% and iron deficiency, defined as serum ferritin <100 ng/ml or serum ferritin 100-299 ng/ml with TSAT <20%, to reduce the risk of HF hospitalization. Treatment of anemia in HF with erythropoietin-stimulating agents is not recommended in the absence of other indications for therapy.
Valve problems occur frequently
Aortic stenosis causes extra workload on the left ventricle, which can lead to cardiac hypertrophy and heart failure. Severe aortic stenosis is present when the valve opening area is ≤1 cm² or when the mean pressure is ≥40 mmHg. This leads to an increase in LV afterload and LV hypertrophy and remodeling, which in turn worsens HF. When using vasodilators, care must be taken to avoid hypotension. Surgical replacement is recommended for all patients <75 Jahren empfohlen, die zusätzlich ein geringes chirurgisches Risiko aufweisen. Die Transkatheter-Aortenklappen-Implantation (TAVI) wird bei Patienten>75 years of age who are at increased surgical risk. However, due to the gentle procedure, TAVI is also being used more and more in younger patients.
Aortic regurgitation can also develop into heart failure over time. Aortic regurgitation is considered severe when there is a large volume of regurgitation and reflux into the aorta. This leads to progressive LV dilatation and subsequent dysfunction, which in turn worsens HF. Beta-blockers should be used with caution because they may prolong diastole and worsen aortic regurgitation. The surgical approach is considered the standard of care for aortic regurgitation, but TAVI is also increasingly used particularly in high/prohibitive surgical risk.
Severe mitral regurgitation (MR) can also cause heart failure. Surgical intervention, preferably repair, is recommended in patients with severe primary MR and HF symptoms. If surgery is contraindicated or considered high risk, percutaneous repair may be considered. In patients with severe secondary MR and HFrEF requiring revascularization, mitral valve surgery and coronary artery bypass grafting (CABG) should be considered. Isolated mitral valve surgery may be considered in symptomatic patients with severe secondary MR despite optimal therapy and low surgical risk
Tricuspid regurgitation (TR) may be caused by or a consequence of RV dysfunction and HF. Treatment of HF with TR includes drug therapy (diuretics, neurohormonal antagonists). In selected cases, transcatheter therapy and surgery may be considered. Tricuspid valve surgery is recommended in patients with severe TR requiring left-sided cardiac surgery. It should also be considered in patients with moderate TR and tricuspid valve dilatation requiring left-sided cardiac surgery and in symptomatic patients with isolated severe TR. Transcatheter techniques have recently emerged as potential treatment options for TR. Preliminary results show improvement in severity and symptoms of TR with low complication rates.
Cardiac amyloidosis still an underdiagnosed cause
Typically, one in six patients with unexplained left ventricular hypertrophy and/or HFpEF suffers from cardiac amyloidosis (CA). The two most common forms are light chain immunoglobulin (AL) and transthyretin (ATTR) amyloidosis. An age >65 years and HF together with LV wall thickness >12 mm on echocardiography are the main criteria for suspicion of CA. Cardiac imaging and endomyocardial biopsy (EMB) or extracardiac biopsy are required for the diagnosis of AL-CA in patients with abnormal hematologic tests. Technetium-labeled 99mTc-PYP## or DPD$ or HMDP& scintigraphy with planar and SPECT*** imaging has a specificity and positive predictive value for ATTR-CA of up to 100%. In contrast, CMR£ has a sensitivity and specificity of 85% and 92%, respectively. However, EMB remains the gold standard for the diagnosis of ATTR-CA with sensitivity and specificity approaching 100%.
## mTc-PYP=Technetium-labeled 99mTc pyrophosphate
$ DPD=3,3-diphosphono-1,2-propanedicarboxylic acid
& HMDP=hydroxymethylene diphosphonate
*** SPECT = single photon emission computed tomography
£ CMR = cardiac magnetic resonance
Literature:
- PD Dr. med. Philip Haaf: Herzinsuffizienz mit reduzierter und erhaltener EF. Forum Medizin Fortbildung (FomF), Update Refresher 2023, Kardiologie I, 24.01.2023.
- McDonagh TA, et al.: 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal, Volume 42, Issue 36, 21 September 2021, Pages 3599–3726, https://doi.org/10.1093/eurheartj/ehab368.
Further reading:
- Zeppenfeld K, et al.: 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. European Heart Journal, Volume 43, Issue 40, 21 October 2022, Pages 3997–4126, https://doi.org/10.1093/eurheartj/ehac262.
HAUSARZT PRAXIS 2023; 18(2): 20–21
CARDIOVASC 2023; 22(1): 26–28











