In family practice, patients with ear, nose, and throat disorders are common outside of the cold season. Above all, a runny nose and sore throat are part of everyday practice. Dr. Mesut Pasha, Head Physician, ENT Clinic, Baselland Cantonal Hospital, Bruderholz site manager, gives tips on treatment by a general practitioner and when an ENT specialist should be consulted.
Acute rhinitis, also known as “common cold”, is a viral infection which is treated symptomatically by decongestant measures. If required due to allergies, an H1 antihistamine or even corticosteroids may also be administered topinasally. It is not uncommon for acute rhinitis to be accompanied by sinusitis, as the swelling of the mucous membranes can lead to obstruction in the approaches to the sinus cavity. The accumulation of secretions leads to bacterial overinfection, which requires appropriate other therapy.
Idiopathic or vasomotor rhinitis must also be differentiated. Non-allergic and non-infectious rhinitis is recurrent clear rhinorrhea that occurs primarily with a change in environment (warm/cold) and food intake. One evidence-based treatment option for this form of rhinitis is the administration of nasal sprays containing capsaicin and eucalyptus. Capsaicin is an active ingredient derived from chili peppers that causes downregulation of transient receptor potential vanilloid (TRPV) receptor expression in sensory nerve fibers (C-nerve fibers). Capsaicin is administered in short treatment doses, usually up to 5× a day. However, when using it, it should be remembered that the active ingredient is sharp and can cause extensive irritation in the nose, such as burning, sneezing and coughing. Therefore, the first application should be done with local anesthesia or low dose if necessary. [1]
What do the EPOS recommendations say?
In acute uncomplicated rhinosinusitis, systemic antibiotics have been administered, decongestant measures have been performed, and mucolytics and analgesics have been used. With the European position paper (EPOS) from last year, a more guideline-based treatment now exists. Therapy is therefore symptomatic for the first five days, if necessary with corticosteriods topinasal. Only after a symptom score of seven, with an analog scale up to ten, is treatment with amoxicillin given. If there is no improvement within 48 hours, an ENT specialist should be consulted. The administration of macrolides, tetracyclines and cotrimoxazole is not recommended due to the pathogen spectrum and side effects.
In the presence of frontal sinus involvement or frustrated prior therapy as well as underlying immunosuppressive disease, acute uncomplicated rhinosinusitis can quickly become acute complicated rhinosinusitis. Primary therapy then consists of administration of topinasal steroids, aminopenicilin with beta-lactamase inhibitor (if no antibiogram is available), oral cephalosporin or clindamycin with fluoroquinolone if necessary. If additional orbital complications occur, surgical intervention is usually required.
According to EPOS 2020, chronic rhinosinusitis is defined as chronic rhinosinusitis with or without nasal polyps. To be distinguished from this are inflammations due to another underlying disease, such as ciliary dyskinesia, cystic fibrosis, type I allergies or Asperin-sensitive respiratory diseases. In ciliary dyskinesia and cystic fibrosis, only symptomatic therapy is given. In type I allergy, specific immunotherapy and/or allergen restriction should be performed, whereas adaptive deactivation or specific oral tolerance induction should be performed in asperin-sensitive respiratory disease.
Chronic rhinosinusitis is not a risk factor for the development of sinunasal carcinoma or nasopharyngeal carcinoma. The persistent inflammation leads to inflammation of the paranasal sinuses. As a result of inflammation, the so-called remodeling of the mucosa occurs. A biofilm forms, which is a possible cause of recurrences and therapy resistance. A permanent cure is usually only possible by surgery. Nevertheless, topical corticosteriods should be used, even before surgery, as they reduce potential complications. In childhood, topical corticosteriods are not recommended according to EPOS 2020. However, rhinopathia gravidarum is treatable without hesitation with modern topinasal steroids. Standard surgical treatment procedures include endoscopic/microscopic-assisted paranasal sinus surgery, with the goal of restoring ventilation to the paranasal sinuses. It is important to operate in a way that is gentle on the mucosa, since an excessive reduction in the volume of the nasal concha can lead to paradoxical nasal breathing obstruction (“empty nose syndrome”). Postoperative follow-up with inhalations and nasal rinses is also essential. Nasal rinses with topical corticosteriods have proved particularly effective, as the active ingredient has a longer contact time compared with spray aerosols and is therefore more effective. In addition, hypertonic saline solutions are recommended.
Epistaxis: Mostly harmless, rarely severe
Usually, the source of bleeding is found in the area of the anterior nasal septum, the locus Kiesselbachi. The most common cause is the manipulation of vessels, for example, due to trauma. However, it also happens that the bleeding is blood pressure related or worsened by anticoagulation. These include antiplatelet agents, coumarin derivatives, direct oral anticoagulants (DOAs), and heparins. In the case of marcoumar, standard coagulation diagnostics are sufficient. Diagnosis is more difficult with DOAKs because no specific antidotes are available to date. Due to the relatively short half-life, in this case the spontaneous course is awaited with simultaneous application of local measures. Therapy depends on the localization and primarily includes compression of the nostrils and coagulation. If the bleeding still cannot be stopped, anterior or posterior nasal tamponade is an option. In addition, tranexamic acid can be used as a nasal spray or as an impregnated nasal tamponade. In addition, if severe nosebleeds occur in children, juvenile angiofibroma should be ruled out. The differential diagnosis also includes Rendu-Osler-Weber’s disease, for which angiogenesis inhibitor injections have been shown to be effective.
Tonsillitis usually viral
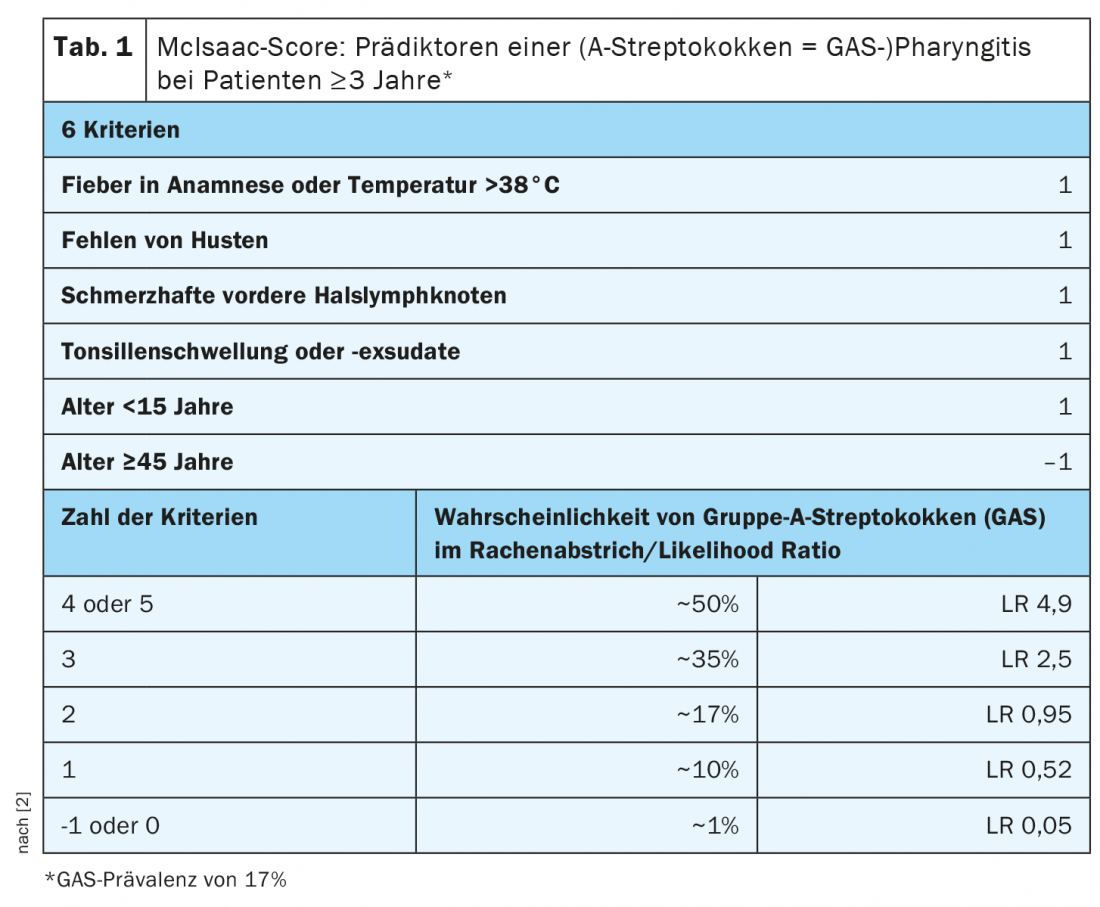
Tonsillitis is an infectious disease. The acute form is in the vast majority of cases caused by viruses, rarely by bacteria. Treatment is symptomatic with astringents, analgesics, and corticosteriod if necessary. In bacterial tonsillitis, the McIsaac score is useful in predicting the likelihood of a positive culture for group A beta-hemolytic streptococci in patients (Table 1) [2]. The indication for therapy is based on the risk of tonsillogenic sequelae, such as acute post-streptococcal glomerulonephritis or rheumatic fever. The administration of penicillin V for 7-10 days is recommended. In case of penicillin intolerance, cephalosporins or clindamycin may be administered alternatively for five days. Macrolides, tetracyclines, and cotrimoxazole are not indicated because of a different pathogen spectrum and side effects. As a result of an immune reaction of the delayed type, against the exotoxin of beta-hemolytic streptococci, scarlet fever exanthema may also occur. Scarlet fever is characterized by a vigorous immune response characterized by flushing of the cheeks, perioral pallor, an edberry or raspberry tongue, and a fine-spotted exanthema most pronounced in the groin. Corticosteroids are recommended as therapy, specifically 10 mg of dexamethasone daily, as it positively benefits the symptom of sore throat.
Disease with similar symptoms
The differential diagnosis includes infectious mononucleosis, also known as Pfeiffer’s glandular fever, which is caused by the Epstein-Barr virus. Here, in addition to generalized lymphadenitis, there is also hepatomegaly. The therapy is purely symptomatic. It should be borne in mind that the administration of amoxicillin or ampicillin can lead to drug exanthema. Complications are rare, but Epstein-Barr viruses are associated with numerous malignancies and chronic fatigue. Tonsillectomy for symptom control or abbreviation of disease progression is not necessary unless airway obstruction is present.
Rather rarely, angina plaut Vincenti occurs, which is caused by a mixed infection with Treponema vincenti and Fusobacterium nucleatum. Clinically, the infection manifests as a usually unilateral tonsillitis with fibrin-covered ulceration of the palatine tonsil. The impressive local finding is often accompanied by relatively minor clinical symptoms.
Indication for tonsillectomy vs. tonsillotomy
Particularly in childhood, tonsillar hyperplasia is frequently seen, increasing in volume after antigen confrontation. There is usually no disease value unless there is respiratory or feeding impairment. A tonsillotomy should then be performed to reduce the volume. Unlike tonsillectomy, part of the tissue is preserved, so the tonsils can continue to fulfill their function in the body’s immune system. Tonsillotomy also has a lower postoperative morbidity and bleeding complication rate. And a history of acute tonsillitis is not a contraindication either.
If, on the other hand, repeated inflammations of the palatine tonsils occur, a viral or bacterial inflammation is present. In this case, a sore throat differentiation should be made into acute tonsillitis, acute pharyngitis, or acute tonsillopharyngitis. According to the current S2k guideline, throat swabs or routine blood tests have no consequence, and antistreptolysin titer (ASL titer) determination is also of no value. The basis for the decision to indicate tonsillectomy is the number of episodes in the last 12 months: < 3 physician-diagnosed episodes, tonsillectomy is not an option; 3-5 physician-diagnosed episodes, tonsillectomy is a possible option; and ≥6 physician-diagnosed episodes, tonsillectomy is a therapeutic option. However, the effect on annual episodes of sore throat is moderate at best, but the effect on quality of life tends to be positive.
Literature:
- Mesut Pasha: The management of common ENT disorders in family practice. Continuing Medical Education Forum, Sept. 08, 2021.
- www.doctors.today/a/atemwegsinfektionen-antibiotikatherapie-bei-kindern-und-jugendlichen-2155218
- Goadsby, et al: A Controlled Trial of Erenumab for Episodic Migraine. N Engl J Med 2017, doi: 10.1056/NEJMoa1705848.
HAUSARZT PRAXIS 2021; 16(10): 32-33