The more precise the diagnosis, the more successful the therapy. This principle also applies in the field of psychiatry. But the road to a precise diagnosis is still long. Current diagnostic methods are based primarily on the clinical picture. However, the goal of future therapies is to define a tailored treatment by measuring biomarkers, such as physiological, genetic and metabolic factors, which can address the individual characteristics of the patient. This should increase the response to therapy until remission of symptoms in the acute episodes of the disease and by preventing recurrences, as well as lead to improved tolerability. An interplay of pharmacological therapies, psychoeducation, and psychotherapy is imperative for optimal treatment outcomes.
Melancholy as a clinical picture, nowadays known as depression, occurs when the four humors – blood, phlegm, yellow bile, black bile – become imbalanced and the black, burnt bile dominates. At least this is how Hippocrates of Kos (460 BC) understood it. Chr.), the founder of ancient humoral pathology, also known as the four-fluid doctrine. Galenos of Pergamon (130 AD. Chr.) carried this thought further and developed from it the temperament theory, a personality model derived from the Humoralpathologie. This divides the human being according to his basic nature into four temperaments, which he associated with the four bodily fluids (Fig.1). According to his theory, balance of these juices means health, while imbalance causes diseases. In his research, he looked for factors that predisposed people to certain diseases. His interpretation of humoral pathology had an impact as a concept of disease into the 19th century.

With this brief historical outline of the concept of depression, Chairman Prof. François Ferrero, MD, from Geneva, Switzerland, welcomed participants to the breakfast symposium on “What is the purpose of personalized medicine in psychiatry?” at the annual congress of the Swiss Society of Psychiatry and Psychotherapy (SGPP) on September 4 , 2015 in Bern.
Classification systems of mental diseases
Efforts to classify the various mental disorders in a more detailed and biologically differentiated manner are also underway in the field of psychiatry. For years, research has addressed the question of what are the compelling criteria to define depression. The international classifications DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) and ICD-10 (International Classification of Diseases) do not yet allow us to enter an era of personalized medicine. Insufficient knowledge of the etiology of depression and other mental illnesses still sets a limit here. To resolve this, personalized medicine seeks to draw on new insights from molecular biology, genetics, neurocognition, cerebral imaging, and other biomarkers.
Influence of personalized medicine on diagnosis and therapy
Personalized medicine, or precision medicine as it is also known today, aims to increase the accuracy with which patients are diagnosed and subsequently treated. The currently very general diagnosis of depression is to be divided into neurobiologically based subgroups and thus enable a more individual and targeted treatment. This opens new fascinating perspectives and allows to better treat the individual in his uniqueness through biological, psychological and social treatment approaches.
The topic of pharmacologically and psychotherapeutically individualized treatment in depression is one of the research focuses of Prof. M.E. Keck’s group at the Max Planck Institute of Psychiatry in Munich, Germany. Stefan Kloiber, MD, senior physician and research associate at the Institute, presented current research results on the occasion of this symposium.
Depression – a challenge for classification
In Germany, it is estimated that about 4 million people with depression require treatment, of which only about 10% receive adequate therapy. According to the Swiss Health Survey (SGB), 5.2% of the Swiss population suffers from a depressive disorder and only a small proportion of recorded depressed people would be referred to specialized psychiatric treatment [1]. This diagnostic and therapeutic deficit in depression calls for significant improvement in clinical practice. Psychiatric diagnosis, based only on clinical observation and symptoms described by patients, still lacks a link to biological mechanisms of disease.
The challenges of depressive disorders are obvious: depression is posed as an overarching diagnostic construct of various mental and physical symptoms in different combinations. In reality, the disease depression hides different disease mechanisms with equally different symptom constellations. In addition, only a proportion of patients treated respond to currently available therapies. More accurate diagnostics that allow characterization or identification of specific subtypes are therefore highly desirable. What predictors can be identified for a positive response to therapy and which subgroups of patients benefit best from different therapeutic interventions? New treatment approaches and individualized therapies are needed, which can succeed with better transfer between basic research and new clinical therapeutic strategies.
Individual predisposition determines therapeutic success
In drug treatment, pharmacokinetics is a key factor for success. Ingested drugs are absorbed by the intestine, metabolized in the liver and reach the target organs via the bloodstream. Since antidepressants exert their effect in the brain, they must cross the blood-brain barrier after metabolization in the liver. Special transporter proteins (e.g. the P-glycoprotein) are located there, which actively transport various substances, including several psychotropic drugs, from the central nervous system back into the blood. According to the latest findings, genetically determined increased activity of the P-glycoprotein could result in insufficient drug concentration in the brain due to increased reverse transport, which may lead to a poorer response to the administered drug. Depending on the knowledge of the activity of this gene, for example, high-dose therapy could be considered. Determination of the genetic variants of the P-glycoprotein (ABCB1 gene) and other biological information could bring personalized pharmacological therapeutic strategies to success.
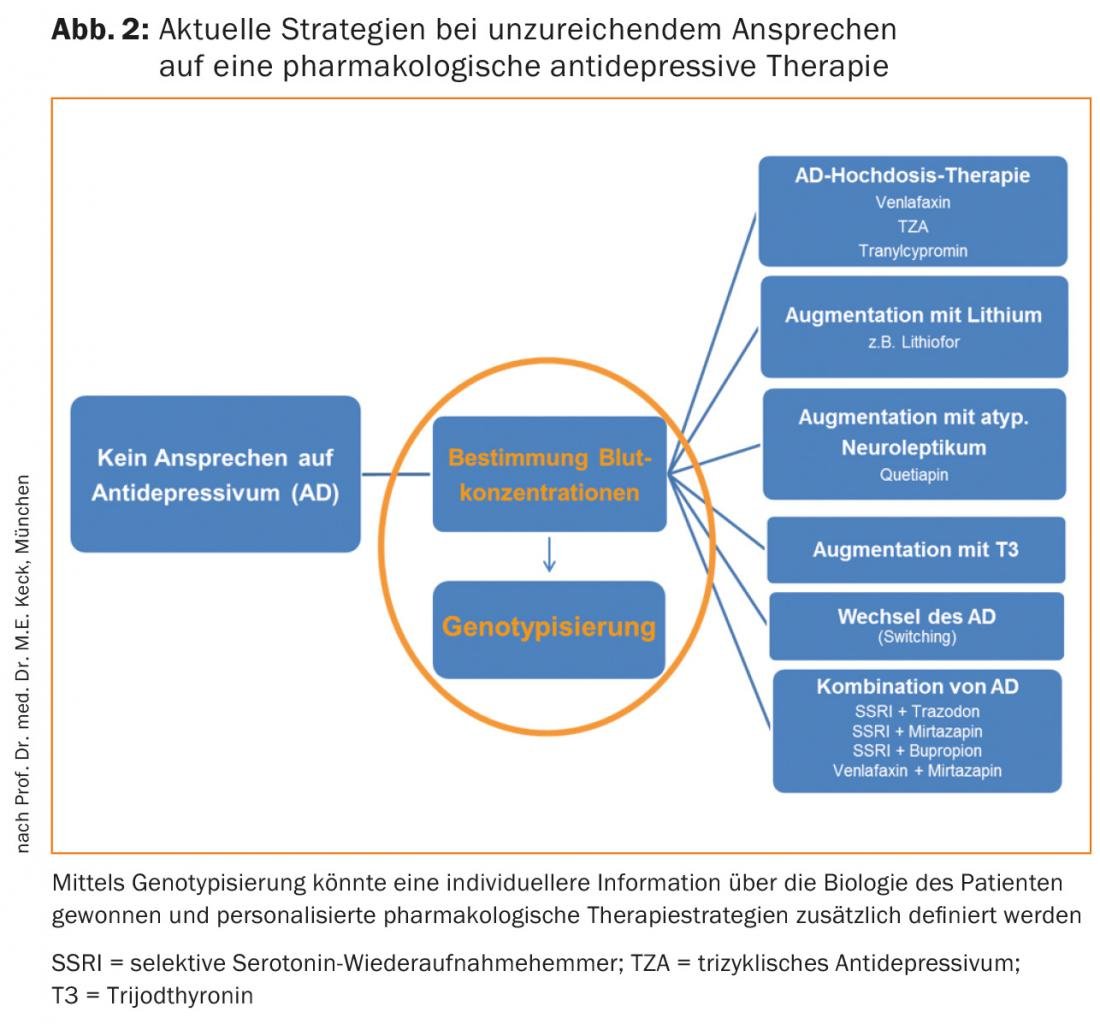
Currently, according to current treatment guidelines, various strategies, such as determination of drug concentration in the blood and various escalations of pharmacological therapy, are used when a patient shows an inadequate response to antidepressant therapy alone. Additional genotyping of variants of the ABCB1 gene could allow for more individualized therapy selection and dosage adjustment through the resulting indication of P-glycoprotein activity (Fig. 2).
Gene variants and epigenetics as differentiators in diagnosis.
Stefan Kloiber, MD, then showed how chronic stress can trigger mental illnesses and how an individual genetic predisposition is significantly involved in the development and progression of disease. In the absence of normalization in the Dex-CRH test, it was shown that patients who still had elevated stress hormones at discharge had a 43% recurrence rate within six months, compared with an 8% recurrence rate in patients with normalized stress hormone levels [2]. Studies showed that the stress hormone system hypothalamic-pituitary-adrenocortical axis (HPA system) is differentially vulnerable throughout life. One reason for the difference in resilience could be attributed to epigenetic factors. In animal experiments, low maternal affection was shown to result in increased methylation and thereby repression of the glucocorticoid receptor (GR) gene, leading to resistance to negative feedback, or overactivity of the stress hormone axis [3,4]. Conversely, positive experiences could lead to an improvement in the stress hormone system.
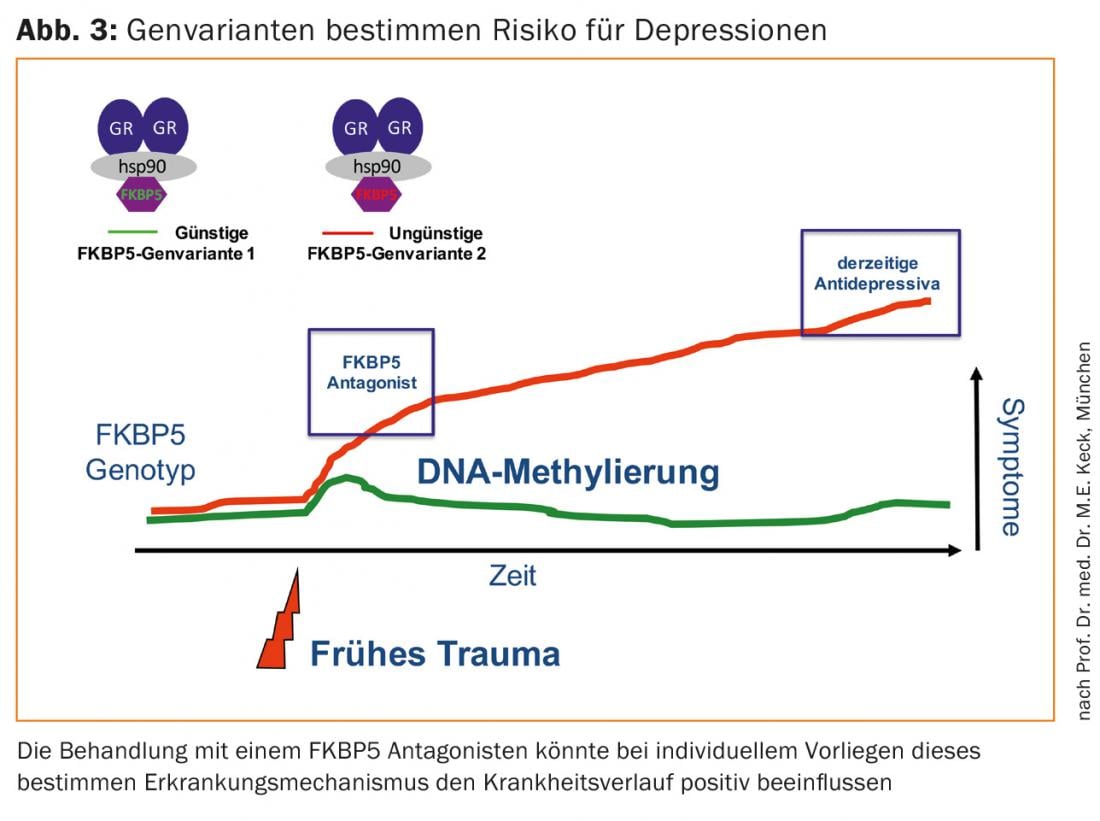
An important factor for stress regulation is the protein FKBP5. It binds to glucocorticoid receptors, thereby affecting their activity and thus the entire stress hormone system. Scientists at the Max Planck Institute have found that in the presence of certain gene variants, the FKBP5 gene can be epigenetically altered after childhood trauma. This subsequently leads to a dysregulation of the stress hormone axis, which increases the risk for depression or anxiety disorder in adulthood [5–7]. Therefore, researchers are trying to develop pharmacological strategies to affect FKBP5, potentially allowing people with childhood trauma who have an unfavorable FKBP5 gene variant to be treated individually and early in the future (Fig. 3).
Staging concepts help in classification and treatment of bipolar disorder
Patient stratification and diagnostic factors are key components in making treatment decisions for patients with bipolar disorder, as Prof. Jean-Michel Aubry, MD, of the University of Geneva, emphasized in his presentation.
Bipolar disorders are characterized by great heterogeneity with many different subtypes. The prevalence is 2-3% when all subtypes of the bipolar spectrum are included. Thus, this ranges from normal mood swings to type I bipolar disorder, which is also characterized by considerable variance in terms of number of relapses and quality of remission after each episode (Fig. 4).
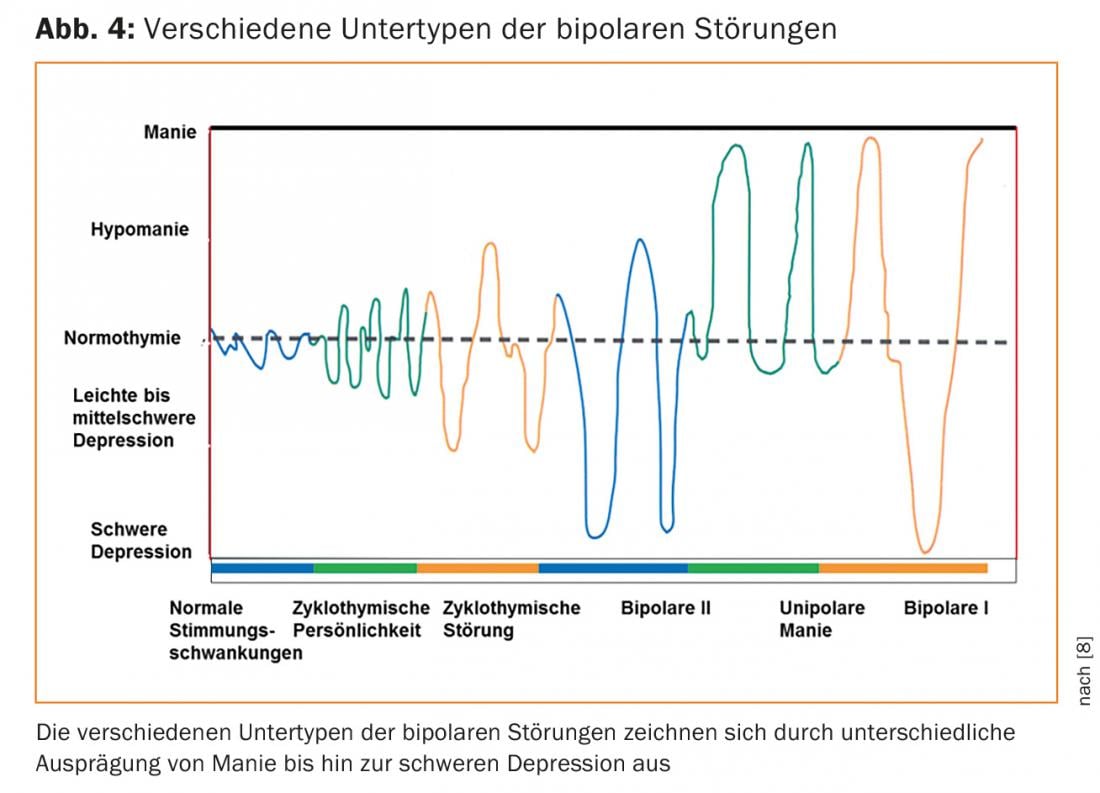
In order to classify the different stages of bipolar disorder, the concept of staging was developed about ten years ago, and since then various models have been developed, which are currently attracting great interest [9]. A common goal of these models is to better select pharmacological and psychotherapeutic treatment in clinical practice in the future. For example, one study showed that already today, patients in stage I are more often prescribed monotherapies, while patients in stage II are given a combination of two molecules and patients in stages III and IV are more often given polypharmacy with at least three psychotropics [10]. Further, these staging models should help select psychotherapeutic and pharmacologic interventions specific to each stage.
Diagnosis with the aid of biomarkers
To further characterize the disease of bipolar disorder, research is now being conducted on various biomarkers. Several biomarkers have been studied in the past, such as epigenetic markers, immune-inflammatory markers, cognitive endophenotypes, sleep and circadian markers, and brain tomography, but so far no markers are sensitive and reliable enough to draw more accurate conclusions about the disease. The specificity and sensitivity of potential biomarkers still need to be greatly refined so that they can be used to specify the different developmental stages of bipolar disorder.
Duration of disease and start of therapy influences treatment success
The duration of the disease and the previous history seem to be of central importance for successful treatment. A study by Kessing et al. was able to show that starting lithium therapy as early as possible in the course of the disease increases the likelihood of response to lithium [11]. Likewise, the number of episodes seems to be crucial for the treatment success: the response to therapy is better if there were less than five episodes before the first treatment, whereas if there were more than ten episodes, the effectiveness of the treatment was lower [12].
As far as psychoeducation is concerned, the picture is similar; again, treatment efficacy is highly dependent on disease progression; one study suggests that fewer than seven previous episodes form the boundary between response and nonresponse to psychoeducation [13]. Thus, these studies also support the idea of early intervention after diagnosis.
Outlook
In addition to all the new findings in genetics, epigenetics, psychoeducation, psychotherapy and drug treatment, at the end of the symposium all speakers emphasized the importance of cooperation between doctor and patient – the active participation of the patient and the associated adherence to therapy have a high therapeutic value.
Take home messages
- The goal of personalized medicine/precision medicine is to increase the accuracy of diagnosis and subsequent therapy.
- Personalized medicine draws on new insights from molecular biology, genetics, neurocognition, cerebral imaging, and other biomarkers.
- Gene variants of FKBP5 may differentially influence risk for depression or anxiety disorder in adulthood following trauma in childhood.
- Staging is used to classify the different stages of bipolar disorder in order to tailor pharmacological and psychotherapeutic interventions.
- Disease duration and history are central to successful treatment of bipolar disorder.
- The active participation of the patient and the associated adherence to therapy have a high therapeutic value.
Source: Annual Congress of the Swiss Society for Psychiatry and Psychotherapy (SGPP), September 2-4, 2015, Bern.
Literature:
- Baer N, et al: Swiss Health Observatory, 2013.
- Zobel AW, et al: J Psychiat Res 2001; 35(2): 83-94.
- Feder A, et al: Nat Rev Neurosci. 2009; 10(6): 446-457.
- Meaney MJ, Szyf M: Trends Neurosci 2005; 28(9): 456-463.
- Binder EB, et al: Nat Genet 2004; 36(12): 1319-1325.
- Binder EB, et al: JAMA 2008; 299(11): 1291-1305.
- Klengel T, et al: Nat Neurosci 2013; 16(1): 33-41.
- Goodwin F, Jamison KR: Manic-Depressive Illness: Oxford University Press, 1990, 2007.
- Kapczinski F, et al: Acta Psychiatr Scand 2014; 130(5): 354-363.
- Goi PD, et al: Rev Bras Psiquiatr 2015; 37(2): 121-125.
- Kessing LV, et al: Br J Psychiatry 2014; 205(3): 214-220.
- Berk M, et al: Bipolar Disord 2011; 13(1): 87-98.
- Colom F, et al: Acta Neuropsychiatr 2010; 22(2): 50-53.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(1): 48-52.
HAUSARZT PRAXIS 2016; 11(2): 38-42