Modern diabetes devices make everyday life much easier for many sufferers. However, as good as they are at helping to optimize management, they can also cause problems elsewhere: A large number of patients develop irritation and inflammation of the cutis when the devices are worn permanently on the skin.
Devices for diabetics, such as insulin pumps, glucose sensors and integrated automated insulin delivery (AID) systems, have significantly changed and influenced diabetes management. This is particularly true for people with type 1 diabetes and increasingly also for those with type 2 diabetes. The devices are designed to be worn permanently, which requires the constant use of infusion sets, patch pumps or glucose sensors inserted into the skin.
Studies have already shown that skin problems associated with diabetic devices are unfortunately quite common. Skin complications will continue to pose a major challenge in terms of device use in the foreseeable future. Prevention strategies could counteract this, as Anna Korsgaard Berg, Copenhagen University Hospital – Steno Diabetes Center Copenhagen, Herlev, Denmark, explained [1].
As easy and practical as it may seem to wear diabetes devices on the skin, the clinical reality is different for 30-90% of patients: They develop various types of skin irritation due to these devices. The Danish scientist divides skin problems into four main groups:
- Lipodystrophies (lipoatrophy and lipohypertrophy, which have also been observed with the use of insulin pens)
- Contact dermatitis (eczema reactions, which are quite common and probably related to the patch)
- Infections
- Skin lesions (a group of non-specific reactions attributable to the devices).
In addition to these visible skin reactions, itching is the main symptom. It is very commonly reported in users of insulin pumps and glucose sensors and can occur without additional visual symptoms or in association with contact dermatitis, scarring, wounds or lipodystrophy. “Itching can be a very frustrating symptom that interferes with everyday life. In children, it is accompanied by sleep disturbances, difficulty concentrating and attempts to scratch off the device,” explained Korsgaard Berg. Itching can ultimately lead to a vicious circle in which the skin barrier is damaged by scratching, which increases the penetration of allergens and increases susceptibility to contact dermatitis.
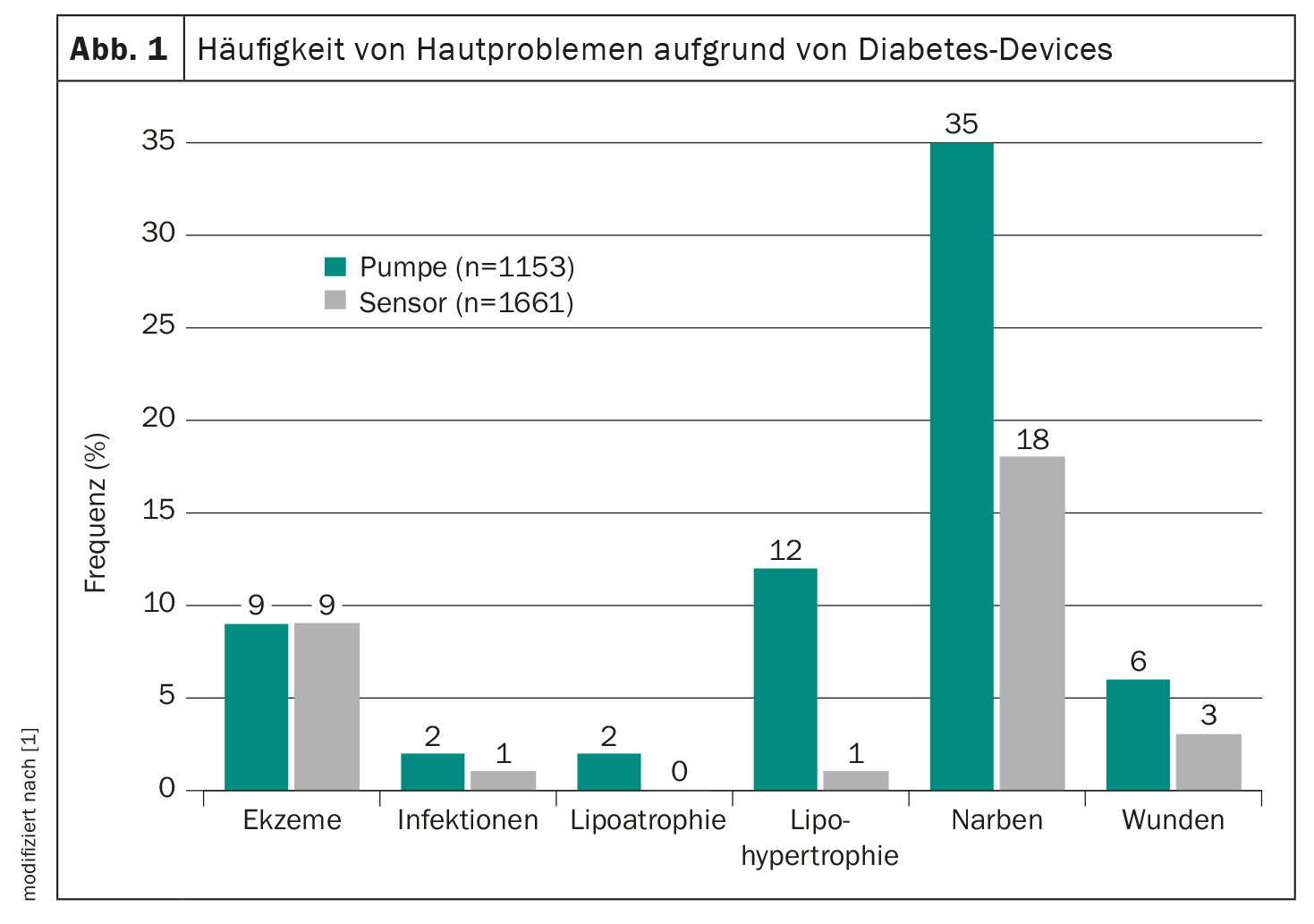
The speaker was involved in a multicenter study in which the skin of all patients who came to the outpatient clinic was examined for 4 weeks in 22 centers around the world. For children and adolescents, 9% of patients were found to have current eczema; scars were more often caused by pumps than by sensors (Fig. 1) .
Lipodystrophies
Lipodystrophies are known complications of insulin treatment that impair insulin absorption and occur in the subcutaneous layer of the skin, whereas most other skin problems begin at least in the epidermal or dermis layer of the skin [2]. They can be divided into lipohypertrophy and lipoatrophy.
Lipoatrophy is a very rare complication. The ethology of lipoatrophy is not well understood, but it is a type of non-specific autoimmune response to insulin. The treatment usually consists of changing the type of insulin.
Lipohypertrophy is a common reaction to insulin and is only triggered by the insulin pump and not by the glucose sensor. “It can be seen as a consequence of the anabolic effect of insulin and leads to hyposensitized areas, which means that many tend to put the devices on that side because it doesn’t hurt as much. This greatly affects insulin absorption and therefore it is important to avoid these areas for the insulin pump.” Some studies show that the glucose sensor works very well in these areas, so patients should be advised to use the glucose sensor there instead of the pump.
Ultrasound has been shown to be helpful in the assessment of lipohypertrophy and is more sensitive than palpation alone.
Contact dermatitis
One of the most common reactions to diabetes devices is contact dermatitis, an inflammatory skin reaction caused by either irritating or allergenic substances and is therefore referred to as irritant or allergic contact dermatitis. The reaction is painful and itchy, and the skin is typically very red.
The first prospective study of skin problems found that between 14% and 35% of insulin pump and glucose sensor users develop contact dermatitis, but the true prevalence of irritant/allergic contact dermatitis is difficult to determine as it requires a patch test and therefore a referral to a dermatologist.
Infections
Skin infections are no longer as common as they were 20 years ago, which is mainly due to improved hygiene measures and advances in the design of infusion sets. They are caused by colonization with microorganisms, mainly staphylococci and streptococci. It may also be a secondary infection associated with contact dermatitis or itching, which make the skin susceptible to these infections. They occur most frequently in connection with the insulin pump and less frequently with the glucose sensor.
Skin injuries
Skin lesions are a non-specific group of reactions that are mostly related to the bonding or removal process. These include wounds, hyperpigmentation and scars, but also the small “dots” that are frequently observed. Most of these reactions are thought to be related to the medial adhesive or the device itself, which is why these reactions, including contact dermatitis, are referred to as MARSI (Medical Adhesive-Related Skin Injury).
The scars may be more of a chronic disorder of the skin that develops over time: they may also be a later clinical manifestation of chronic itching, infection or contact dermatitis.
Causes of skin problems
Medical adhesives are used in all plasters. There are four groups of adhesives: Latex-based, arylate, silicone and hydrocolloid. Most adhesives are based on acrylate. “Especially with children and adolescents, it is important that the plaster adheres well enough so that we don’t have to stick another plaster over the device. So it’s a balancing act between ensuring the device adheres properly and avoiding skin irritation,” explained Korsgaard Berg.
The design of the appliances is seen in many reviews as the main cause of skin problems. In allergic contact dermatitis, the causes of reactions are allergens, but in this case not only allergens from the medical adhesive that touches the skin are responsible, but also allergens from the adhesive in the housing part of the device. The adhesive must be strong enough to ensure sufficient adhesion so that no additional patches are needed to keep the device on for the entire wearing time, and often more reactions are observed when the device is changed for longer wearing times. Cross-sectional studies have identified various factors associated with skin problems, including a tendency to atopy, prolonged wearing time of the device and a low number of skin patches [2].
There are also other non-specific factors such as occlusion, moisture, tension and pressure when the appliance is attached. Over time, this also causes a small, non-specific group of reactions. It has been speculated whether a more vulnerable skin barrier in people with type 1 diabetes could explain the high rate of skin problems, but no evidence for this was found in a case-control study in which various skin barriers were examined.
Cross-sectional studies have shown various association factors with skin problems, including an atopic disposition, i.e. atopic dermatitis, asthma or allergic dermatitis, which lead to an increased risk of developing skin problems. The duration of device use also plays an important role here. “It takes some time for skin problems to become noticeable. It has been found that reactions start around 4 to 8 months after the insertion of a new device. Some patients reported that they had no reactions for more than 8 months and then eventually started to react to these devices,” the expert explained.
Prevention of skin problems
The 6 techniques for the prevention of skin problems were described in the consensus statements on medical adhesives [3]. This applies not only to devices for diabetics, but to all applications of medical adhesives:
- Choice of adhesive
- Repeated gluing
- Long-term use of adhesive tapes/tapes
- Skin care
- Laying technique
- Removal technique.
The first 3 points can hardly be influenced, but the last 3 points were used by Anna Korsgaard Berg and her colleagues in a study [4] as part of a skin care program to prevent skin problems. In the cluster-controlled skin care study, an intervention group (n=112), which considered skin care, application and removal, was compared with a control group (n=58) with usual care. Children and adolescents who had started treatment for diabetes were included in the study and followed up for 12 months.
Three recommendations were made:
- Avoid alcohol or disinfection when putting on a new diabetes device at home (also recommended in hospitals). The use of disinfectants dries out the skin.
- Use of liquid lotion at the “break points” for the diabetes device to strengthen the skin so that it can tolerate wearing these devices.
- Gentle removal.
The results showed that eczema and itching were not eliminated in the skin care program group, but wound development was reduced by two thirds compared to the control group (Fig. 2) .
Therapy options
The treatment of skin problems includes not only the acute treatment of the exact reaction, but also the secondary prevention of new reactions.
Most skin problems heal over time due to the natural healing process and do not require acute treatment other than avoiding the affected area (changing the side of the device and not using a new device on the affected skin). Secondary prevention, on the other hand, is a step-by-step model in which the first step is skin care and the use of different spots. The next step is a thin liquid barrier that is glued to the skin before a new diabetes device is attached to protect the skin. When applying a patch, it is important to find one that is skin-friendly and not acrylic-based. The final step is to use a preventative steroid injection or lotion on the skin before inserting a diabetes device. “However, watch out for skin atrophy caused by steroids. It has been proven that the daily use of a steroid lotion over a period of only 4 weeks leads to skin atrophy, which means that the skin barrier is impaired and you are therefore in a vicious circle. It is therefore recommended to reduce the use of steroids and find other solutions.”
The increasing popularity of diabetic devices has led to a corresponding increase in the incidence of skin problems associated with their use. The long-term dermatological and allergic consequences of the devices are still largely unknown, so further investigation and ongoing research is needed to better understand the long-term consequences and potential benefits of using more skin-friendly adhesives, concludes Anna Korsgaard Berg.
Congress: ATTD 2024
Sources:
- Korsgaard Berg A: Lecture “Skin Problems caused by Diabetes Devices”, Session “Skin problems in diabetes”. The 17th International Conference on Advanced Technologies & Treatment for Diabetes, Florence, March 6-9, 2024.
- Korsgaard Berg A, Zachariae C, Nørgaard K, Svensson J: Skin Problems due to Treatment with Diabetes Technology: A Narrative Review. Medical Research Archives 2023; doi: 10.18103/mra.v11i11.4747.
- McNichol L, Lund C, Rosen T, Gray M: Medical Adhesives and Patient Safety: State of the Science. Journal of Wound, Ostomy and Continence Nursing 2013; 40(4): 365-380; doi: 10.1097/WON.0b013e3182995516.
- Korsgaard Berg A, Grauslund AC, Sørensen F, et al: A Skin Care Program to Prevent Skin Problems due to Diabetes Devices in Children and Adolescents: A Cluster-Controlled Intervention Study. Diabetes Care 2023; 46(10): 1770-1777; doi: 10.2337/dc23-0462.
InFo DIABETOLOGY & ENDOCRINOLOGY 2024; 1(2): 30-32 (published on 2.5.24, ahead of print)