The essential foundations of palliative care can be well established in all specialties through continuing education, but knowledge of the four dimensions of palliative care detailed in this article is crucial. The salutogenetic concept and resource-oriented care continue to play an important role. In addition to technical expertise, human competence and interprofessionalism are also important components in ensuring that patients receive optimal therapy and care.
The term palliation is derived from the Latin word “pallium” translated coat. What is meant by this is to surround particularly vulnerable patients in difficult phases of life and illness with a shell in order to achieve quality of life and a reduction in suffering. As the WHO definition of palliative care implies, in addition to patients, family members are also target groups for care and support.
Complementing Engel’s bio-psycho-social model, palliative care introduces another dimension, that of meaning or spirituality. More than almost any other specialty, palliative medicine demands a holistic and interprofessional approach in its concept of care.
Patients receiving palliative care are confronted with (life)threatening illnesses, and it is not always only tumor diseases that play a role here. Severe heart and lung disease, as well as metabolic disorders, can be a “burden of illness” analogous to cancer.
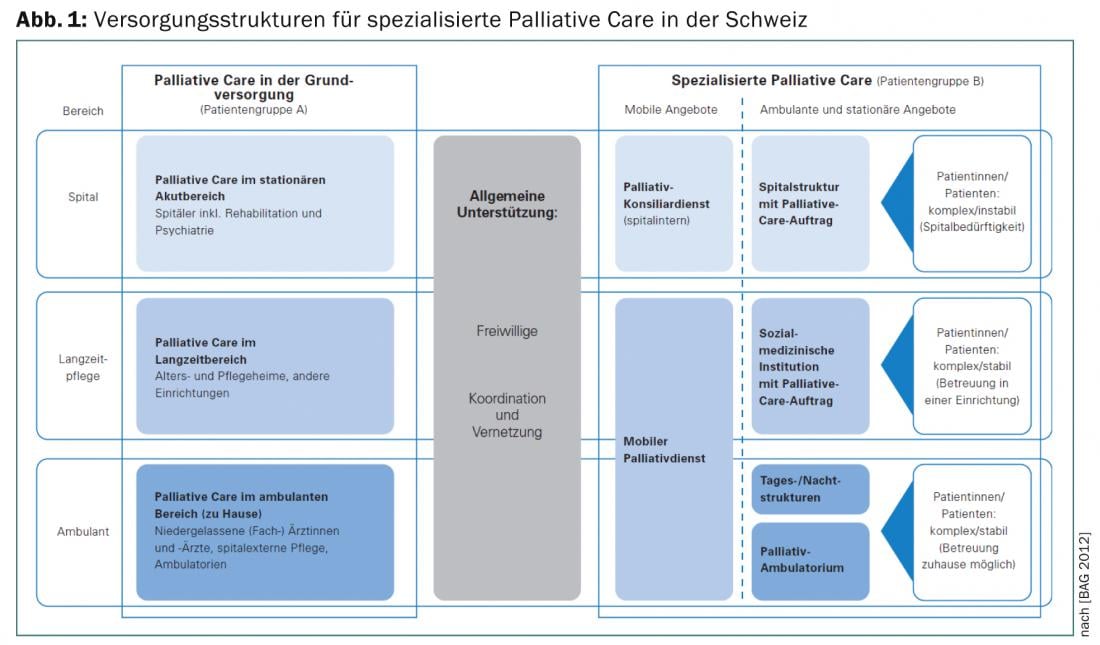
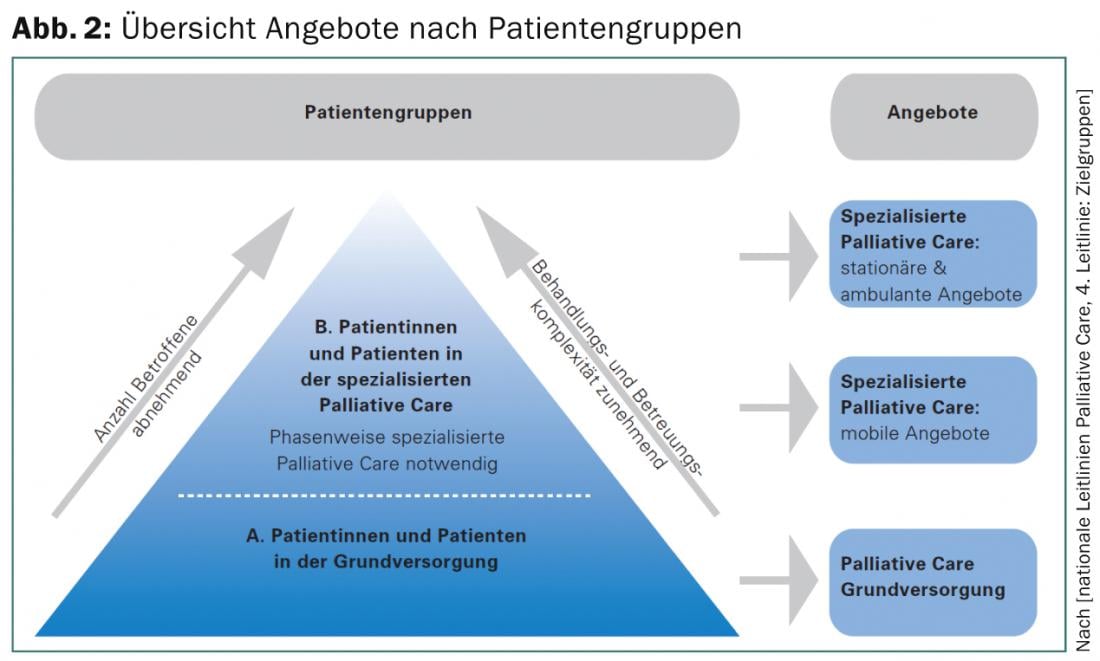
Organizationally and institutionally, a distinction is made between long-term palliative care and specialized palliative care; here, not least, a very decisive differentiation, also with regard to cost bearers, is often difficult and the subject of protracted disputes. An overview of the care structure and offerings in Switzerland are shown in Figures 1 and 2.
If palliative care is provided in the home setting, questions also arise about the network that can provide care. In the specialized institution, the tasks are performed by the interprofessional teams, but this also shows a discrepancy. 80% of the population wants to be cared for and die at home, but for only 20% is this wish feasible.
In the normal inpatient setting, medical and nursing care is made possible, but here there is often a lack of the necessary knowledge about the specifics of palliative care. However, patients do not have to be cared for exclusively in specialized institutions; rather, those responsible can provide good care through further training and the development of standards; in addition, palliative physicians can be consulted on an interdisciplinary basis.
Due to the diversity of topics and problems, interprofessionality is of great importance. Physicians, nurses, physical therapists and psychooncologists, occupational and respiratory therapists, nutritionists, social workers and pastoral counselors are all part of a comprehensive care setting. In an institution, these professional groups are readily available, but availability becomes more difficult in the outpatient setting.
The four dimensions of palliative care
To visualize the complexity of palliative care requirements, we would like to use the classification according to the dimensions mentioned above.
Biological dimension: In medicine, this dimension is naturally the starting point for medical interventions and requires the usual skills in evaluating the current and previous medical history. Unlike in acute medicine or with a clearly curative approach, however, the detailed medical facts are not the focus of the anamnesis, but rather the symptoms that bother the patient because of his or her illness. While pain or nausea are usually reported spontaneously by patients, other distressing symptoms are often only experienced when specifically asked. Shortness of breath, loss of appetite, dizziness, weight loss, diarrhea, constipation, impaired concentration, sweating, pruritus, fatigue, and inappetence, in addition to pain, can massively impair quality of life and are more often resistant to pharmacological measures. It is essential to plan ahead during the course of the disease with regard to possible complications, for example ileus in the presence of peritoneal carcinomatosis or the occurrence of delirium in the end-of-life phase.
Psychological dimension: Here, sadness, anxiety and depression play an important role and are often difficult to separate from the physical symptoms. Whether nausea has its origin in the complicated interplay of gastroenterologic, endocrinologic, or mechanical pathologies or is an expression of anxiety cannot be easily distinguished but plays a crucial role in treatment. Coping strategies, defense or repression, and sexuality also belong in this dimension.
Social dimension: The social dimension is of paramount importance in these situations, as the disease and the threat it poses affect both social relationships with partners, children and friends, call autonomy into question, but also have a lasting impact on one’s job, hobbies, housing situation and, not to forget, finances. The design of the last phase of life and the place of dying are significantly determined by the social environmental factors.
Spiritual dimension: It becomes completely difficult with the fourth dimension of spirituality. Physicians in particular are not accustomed to addressing this issue in their medical histories and evaluations. In the existential threat and in the face of one’s own finiteness, this dimension, which is unfamiliar to us, should also be included from the medical side in order to ensure holistic care that corresponds to the wishes of the patient and his relatives. Religious imprinting, helpful rituals, cultural background, the question of the meaning of life and what the end can look like are as central as the recording of physical complaints.
Assessment
In addition to the art of history taking, the sparing use of assessment tools can prevent symptoms or distress from being forgotten in these complex situations. However, it is important to ensure that patients in advanced stages of the disease are not unnecessarily burdened with superfluous questionnaires. We use the adapted “Edmonton Symptom Assessment Scale”, a questionnaire that uses ten items to ask about the main symptoms of the Bio-Psychic Dimensions and also rates their expression on a scale of 0 -10. The instrument is suitable both for assessing the situation at the beginning of treatment and for evaluating therapeutic interventions after they have taken place, in order to document the success or failure of measures.
Although instruments such as the HADS for anxiety and depression are also suitable for the psychological dimension, the medical or nursing interview is more often more effective here, as the stresses from the social sphere can be recorded at the same time. Difficulties may be encountered in distinguishing situationally appropriate sadness or dejection from clinically relevant depression or adjustment disorder, which might be amenable to medication intervention. It must be borne in mind here that the duration of treatment must be sufficiently long for the measure to be successful and that in certain situations the use of depressant benzodiazepines may be more appropriate.
When dealing with social difficulties, both medical and nursing skills are at times overwhelmed. In a clinic, the involvement of social workers can provide valuable services, for example when it comes to clarifying pension issues, facilitating additional benefits and advising on follow-up care if the way back home is questionable. Estate planning can also be addressed. On an outpatient basis, specialized counseling centers, such as the Cancer League, provide valuable services and help with the procurement of aids.
The spiritual dimension can be delegated in part to pastoral counselors and psychooncologists, but when it comes to questions about resuscitation, living wills and measures to be taken in the event of deterioration, it is once again the doctors who are called upon. Regarding assessment, Einstein’s quote is a good guide: “Not everything that can be counted counts. Not everything that counts can be counted.”
Pathogenesis versus salutogenesis
Although the salutogenetic approach is no longer a foreign concept in medicine due to the work of Aron Antonovsky, it must be reflected again and again, especially in palliative care, what the goal of treatment should be. Not curing the underlying disease, but dealing with it, especially by strengthening resources, are central elements of the care philosophy and must be repeatedly addressed by us as those treating the patient. Actually, curative and palliative care should not be an either-or, but a both-and, depending on the current disease situation. However, if the focus shifts, i.e. the focus is no longer on the illness but on being ill, this should be actively communicated.
It is worthwhile to find out whether the patient has a good “sense of coherence” or whether, due to biographical risk factors, the focus tends always to be on “the glass half empty”. The careful adaptation of the hopes of the patients entrusted to us to the real existing possibilities are also an important task, since research results show that the so-called “Calman gap”, i.e. the discrepancy between what is desired and what is possible, can negatively shape the quality of life of palliative patients. The art is not to deprive patients of hope, but also to project their wishes and hopes on a realistic background.
The Sense Model – A Guide
As with many complex care situations, the structure, goal, and course of care can get out of hand. It is therefore helpful to adopt a structured approach analogous to that used, for example, for the treatment of heart failure or diabetes mellitus. We decided to use the SENSE model because of the good experience we had.
Here, the term’s acronyms for S = symptom control, E = decision making, N = network, S = support, and E = end-of-life represent the tasks involved in caring for palliative patients and their families. Depending on the specific situation, a certain area is given more or less importance. The model as a guideline for reviewing necessary measures has now proved very useful in the care provided in our clinic and is found to be equally helpful by all professional groups.
Pharmacology
The specifics of pharmacological interventions in the field of palliative care can only be touched upon in passing here. However, general principles can be established for the drug treatment of the various symptoms. Palliative care requires relatively few preparations, as synergies can often be achieved. Thus, morphine is not only very good analgesic, but also very potent in the control of dyspnea. Sleep disturbances, pruritus, and depression respond well to mirtazapine. Metoclopramide is well suited for opioid-induced nausea; in the absence of a response, the add-on administration of haloperidol, corticosteroids, or the sertrone applies to the treatment of nausea in addition to – if possible – causal cause control. Haldoperidol and quetiapine have an antidelirant effect, while midazolam, which is also used in palliative sedation, has a sedative and antiepileptic effect. It is important in this context to be aware of the possible organ dysfunctions that may affect pharmacokinetics. Most of the drugs used in palliative care are at least partially used off-label, i.e. the substance is not approved by Swissmedic either with regard to the population, dose, form of administration (e.g. s.c.) or the indication in this form. Nonetheless, they are used in the spirit of best practice. Prescribing backup medications for any potential symptom onset is essential. Very helpful are the best practice Bigorio recommendations on a variety of symptoms in palliative care.
Communication
As always in medicine, successful communication is also an indispensable prerequisite for a sustainable doctor-patient relationship in the case of palliative patients. Time, calmness and clear statements as well as the renunciation of empty phrases and generalities are the basis for conversations with patients and relatives. Possible fears and anxieties must be anticipated. A frequent topic of conflict is the issue of nutrition in the palliative situation. The idea of starving to death is threatening for patients and family members alike. Here, a proactive response helps to ensure that in the case of generalized systemic phases of disease, artificial nutrition no longer positively influences the course of the disease. Nonetheless, tube feeding or intravenous caloric intake can be provided after detailed explanation if the patient continues to wish to do so for a defined period. In most cases, however, it can be conveyed that in the absence of a sense of hunger, a high-calorie diet often does more harm than good. Controversy also often ignites over the issue of fluid administration. The pros and cons must be presented to patients and family members.
In the case of difficult communication, it is also important to remember that existing family conflicts or unresolved issues, as well as emotional stress, can sometimes trigger unjust or aggressive behavior on the part of the patient and family members. Clarifying conversations that address the underlying problems without reproachful attitudes and without claiming to be able to resolve long-standing family conflicts are usually helpful here. Holding so-called round-table discussions helps to ensure that everyone involved has the same level of knowledge and understanding.
Summary
Accompanying and caring for seriously ill patients is one of the important tasks of practicing physicians from a wide range of specialties. In this sense, it is to be welcomed that there are increasingly low-threshold offers for further education. The physician care structure needs many general practitioners, internists, oncologists, and surgeons who know the basics of palliative care. For specialized institutions, comprehensively trained physicians are needed who have acquired a certificate of competence in palliative care, as planned for the future, in addition to their specialized training. Geriatricians in long-term care facilities should likewise be further trained for the often even more ethically challenging care of cognitively impaired patients. Last but not least, we also need a number of highly specialized palliative care physicians to advance the academic anchoring of the field and the progress of research activities.
Christel Nigg, MD
Nic Zerkiebel, MD
Literature:
- Neuenschwander H, et al: Palliative Medicine, Krebsliga Schweiz, 2nd revised edition, 2006.
- Beubler E: Kompendium der medikamentösen Schmerztherapie, 4th revised edition, Springer WienNew York, 2008.
- Gallacchi G, et al: Schmerzkompendium, 2nd edition, Thieme-Verlag, 2005.
- Recommendations Breakthrough Pain, ed: Swiss Society for Palliative Medicine, Care and Support, palliative ch palliative.ch 2006.
- Eychmüller St: Sense makes sense, Therapeutische Umschau 2012; 69(2): 87-90.
- Büche D.: Assessment and assessment instrument in palliative care, Therapeutische Umschau 2012; 69(2): 81-86.
- National Strategy for Palliative Care 2010-2012, Federal Office of Public Health (FOPH) 2009. www.admin.ch/palliativecare.
- Indication criteria for specialized palliative care www.bundespublikationen.admin.ch
- Antonovsky A: Salutogenesis. On demystifying health. German edition by Alexa Franke. dgvt-Verlag, Tübingen 1997.
- Hydration at the end of life, Bigorio recommendations: Ed: Swiss Society for Palliative Medicine, Care and Support, palliative ch, 2011.
- Kunz R: Palliative care a comprehensive approach to care, not a new specialty, Swiss Medical Journal, 2006 (87): 1106.
- Swiss Academy of Medical Sciences SAMS: Palliative Care. Medical ethical guidelines and recommendations, 2006.
- Bruera E, et al: The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J of Palliative Care 1991 (7): 6-9.
- Saunders C: Cicley Saunders Dying and living: spirituality in palliative care. Translated from Engl. by Martina Holder-Franz.
InFo Oncology & Hematology 2014; 2(3): 5-8.











