Especially in scarring and androgenetic alopecia, the results of pharmacological therapies are often unsatisfactory, which can be very distressing for affected individuals. Hair transplantation is one way to treat this and other forms of hair loss in a sustainable manner, although the chances of success vary from individual to individual.
The following review article describes the possibilities and limitations in various forms of hair loss from the perspective of a transplanting surgeon who regularly performs hair transplants in her own practice. A portion of patients report directly for consultation and a portion of patients are referred by dermatologists.
Indications at a glance
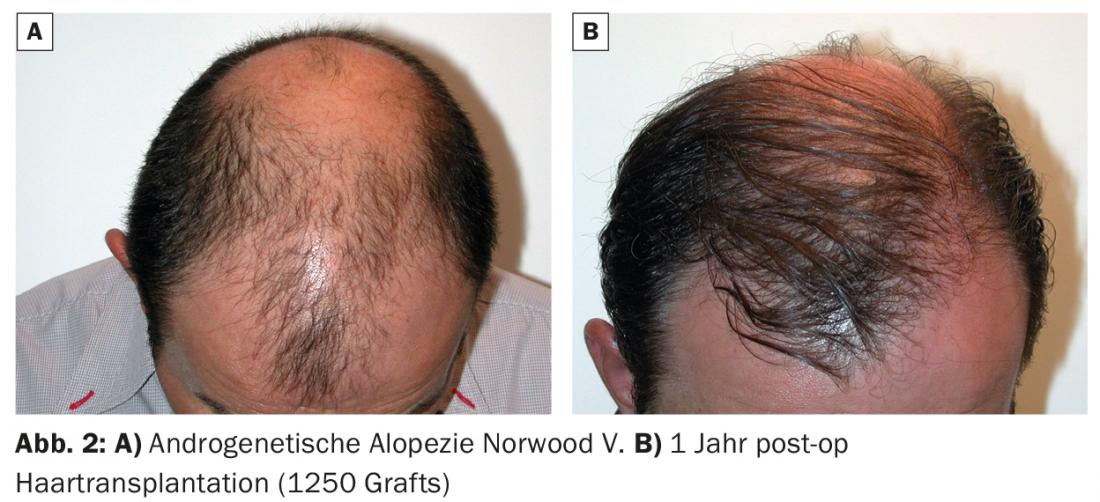
Androgenic alopecia is the most common and classic reason for hair transplantation – both in men and women. The hair loss pattern in men is classified according to Norwood I-VII [1] and describes the typical hair loss pattern in men in the secretory corner, forehead and vertex areas.
In women, hair loss usually appears diffusely in the upper part of the head, described by the classification according to Ludwig [2]. If hair loss in women is very extensive, hair transplantation is not recommended. If it is a limited, broad-based thinning in the front part of the crown that tapers towards the back (fir tree pattern, Olsen classification), it can be thickened by means of a hair transplant and improves the patient’s quality of life enormously. If a woman constitutionally has a very high forehead, the hairline can be advanced through hair transplantation. Transgender patients (male to female) with receding hairline have a desire for a female hairline, which can be feminized in a very elegant and natural way with hair transplantation.
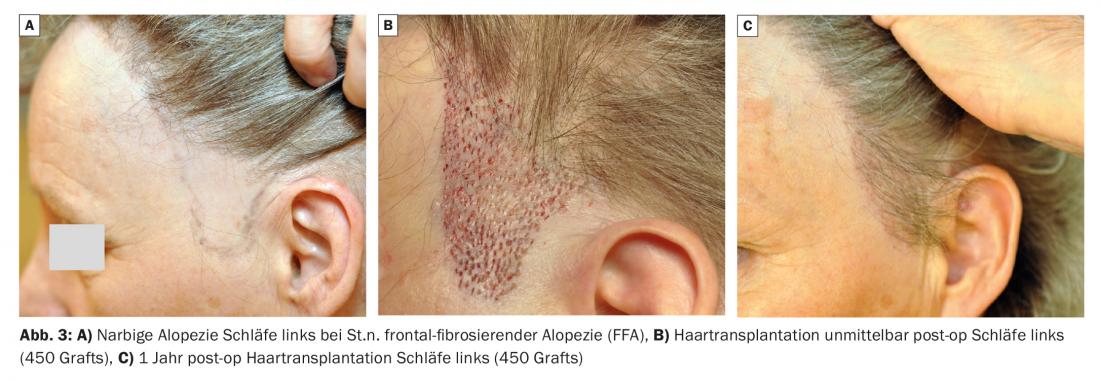
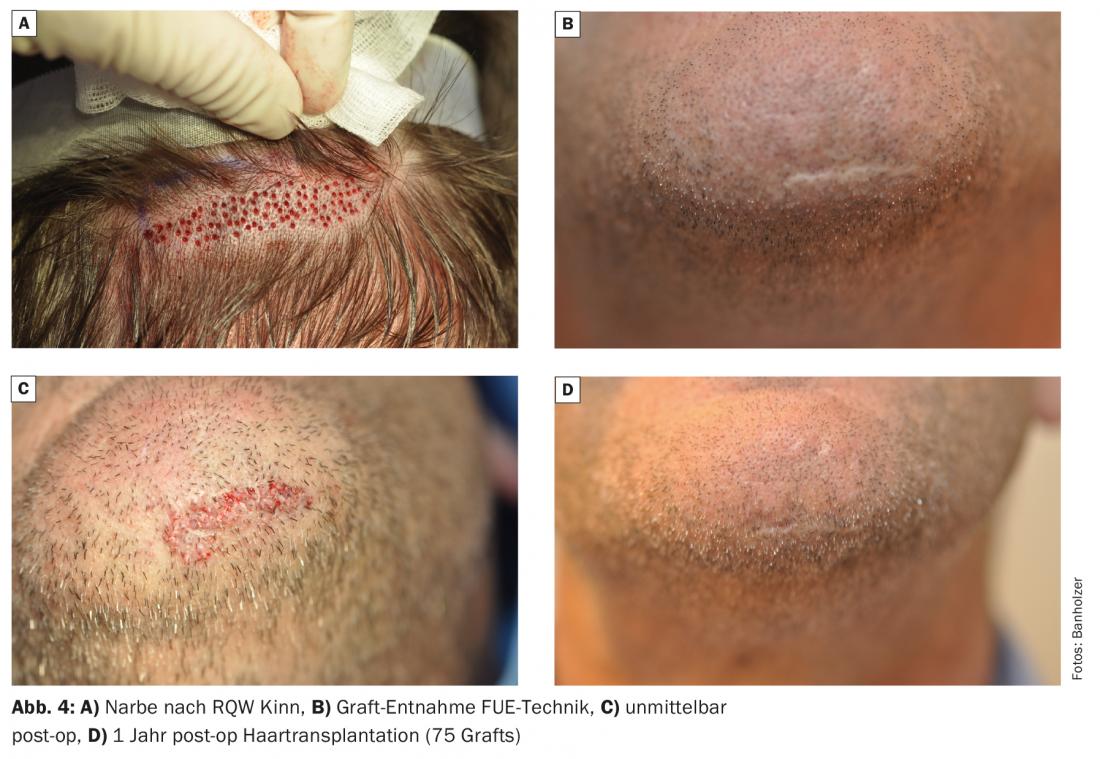
Capillitial scars of various etiologies are often a major problem for patients. Often these scars remind you of a traumatic time. For example, an accident with a burn, or a tumor diagnosis with consequences of invasive tumor surgery or radiation or after treatment of unsightly permanent makeup in the eyebrow area, etc.. Hair transplantation is also a low-risk, low-pain, but very successful therapeutic solution for these patients.

What are the options?
Any hairy area of the body is basically suitable for hair follicle harvesting and these can be transplanted basically anywhere. Those who are not affected by hair loss themselves find it difficult to understand how great the suffering is in these patients. Surgical intervention through hair transplantation can often improve the quality of life in a simple way. Cultural differences on the subject of hair loss are also interesting. In countries with a Muslim background, men often have transplants in the beard area, and in Asian countries there is a desire for chest hair.
Hair transplantation into bald spots is basically suitable regardless of the etiology into all body regions (capillitium, eyebrows, beard as well as pubes or thoracic hair). Hair transplantation into scars is now a medically viable alternative to major procedures such as expander surgery, flap surgery, or skin grafts. Hair transplantation is much less invasive for the patient compared to the above mentioned procedures (no anesthesia, no hospital stay and in most cases only a two-day inability to work). It also greatly minimizes healing costs.
What are the limitations?
In terms of health insurance, unfortunately, the cost of the procedure is not covered in most cases. In terms of medical feasibility, there are the following limitations:
In hair transplantation, not as many hair follicles can be transplanted. The number of hair transplants (“grafts”; also called “follicular units”) is limited on the one hand by the number of hair follicles available (in the case of congenital hair loss, this is limited to the back of the head and the temporal region) and on the other hand by the duration of the procedure and the size of the area to be transplanted as a result of the maximum daily dose of local anesthesia.
Congenital hair loss should not be transplanted until it has been successfully stabilized by long-term pharmacological therapy with finasteride or topical application of minoxidil.
In scarring alopecia due to inflammatory etiology such as frontal fibrosing alopecia, lichen planopilaris or “fibrosing alopecia in a pattern distribution” (FAPD), the inflammatory process must be cauterized for successful intervention. This is difficult to assess both clinically and histologically. Even then, hair transplantation is not always successful and reliable studies are lacking.
In childhood, hair transplantation is not recommended: Firstly, due to lack of compliance in the first ten days after a surgical procedure (careful handling of grafts). Second, the long duration of surgery in a child requires anesthesia (instead of local anesthesia), which is an unnecessary risk medically. It is recommended to wait with the surgical intervention until after puberty.
If a thinned out, i.e. not yet completely bald area of hair is thickened by means of hair transplantation, this often leads to a very pronounced “shock-loss” of the remaining hair, especially in women. This is a temporary complication of hair transplantation, which leads to an even greater thinning of the preoperative hair density during the first six months postoperatively. A prerequisite for passive balding is that the patient is psychologically stable.
In very young patients with congenital hair loss, future progression of androgenetic alopecia must be carefully evaluated and planned for to avoid “overharvesting,” which means not transplanting hair follicles affected by hair loss. This is often difficult to anticipate in very young patients. Firstly, these grafts would fall out again in the longer term, secondly, scars caused by the removal will be visible and thirdly, this can lead to an unnatural hair loss pattern from which the patients then suffer enormously and, due to the lack of donor hair, there is no longer any possibility of correcting this.
Transplantation of body and beard hair into the capillitium is unsatisfactory from an aesthetic point of view and it is not recommended.
Conclusion
Pharmacological therapy of hair loss is often unsatisfactory, especially in scarring alopecia as well as in androgenetic alopecia. As we are all well aware, these patients have a great deal of suffering and surgical intervention such as hair transplantation is the only alternative. It is a minimally invasive procedure; the technique of hair transplantation has developed greatly and today it is impossible to imagine medicine and plastic aesthetic surgery without it. In most cases, it helps the patient to achieve a good, 100% natural and lasting result – provided that the indication is professional, conservative and restrained.
Most hair transplants are cosmetic-aesthetic in nature and not medically necessary. However, these patients are also very grateful that hair transplantation exists and greatly appreciate the improved quality of life it provides.
Take-Home Messages
- 80% of men and 50% of women are affected by constitutional hair loss. The suffering pressure for patients with alopecia of any type/form (congenital hair loss, scarring alopecia) is enormous.
- To help these patients with irreversible damage from hair loss, the only final option is surgical intervention such as hair transplantation. If the indication is correct (congenital hair loss stable), this is the only sustainable, therapeutic solution.
- Hair transplantation is a low-risk and low-pain procedure and is performed on an outpatient basis under local anesthesia and twilight sleep in the practice.
Literature:
- Norwood OT: Male pattern baldness: classification and incidence. South Med J 1975; 68: 1359-1365.
- Olsen EA: Female pattern hair loss. J Am Acad Dermatol 2001; 45(Suppl): S70-80.
DERMATOLOGIE PRAXIS 2019; 29(1): 8-10











