Not all patients with venous thromboembolism have an increased risk of recurrence. Those at high risk benefit from continued anticogulation. To calculate the risk of second thrombosis, the risk factors should be recorded and the absolute risk of recurrence calculated. This should be contrasted with the severe anticoagulant bleeding and, if the risk of recurrence predominates, anticoagulation should be continued.
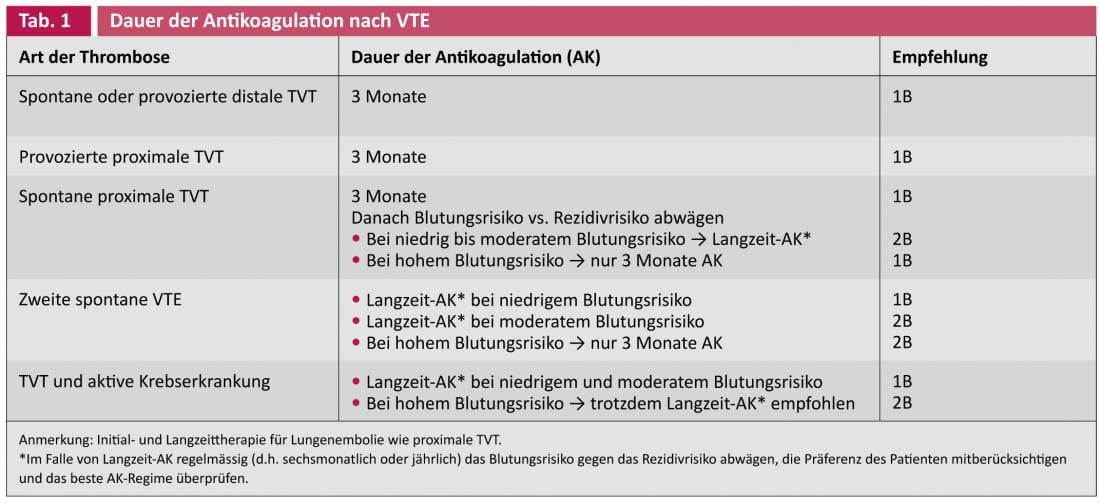
Venous thromboembolism (VTE) includes deep vein thrombosis (DVT) and pulmonary embolism. The absolute risk for the occurrence of first venous thrombosis in the general population is 0.1-0.2% per year and is age-dependent. The risk of recurrence after a previous thrombosis is 5-7% per year, which is 50 to 70 times higher than the risk of a first venous thrombosis [1]. Therefore, it is important to be able to assess the risk of recurrence in an individual patient, as continued anticoagulation (AC) can effectively prevent recurrences. The duration of AK after initial therapy has long been a matter of controversy. Based on numerous studies and meta-analyses, the 9th ACCP Consensus Conference in 2012 arrived at the recommendations shown in Table 1 for the duration of AK [2].
The risk of recurrent thrombosis after cessation of AK depends mainly on two factors:
- Was the acute VTE episode effectively treated, with a minimum duration of AK?
- Are there intrinsic factors that lead to a higher recurrence rate?
Long-term AK – what is it?
Long-term AK is recommended in spontaneous proximal DVT with or without tumor disease and in recurrent thrombosis. Long-term AC is a vague term. How long should be treated at all? Long-term does not mean lifelong. The 9th ACCP Consensus Conference recommends that the duration of AK should be based on individual benefit/risk considerations. No guideline value can be given here that would be equally valid for all patients. The treating physician and the affected patient are thus largely left alone in the decision regarding the duration of AK.
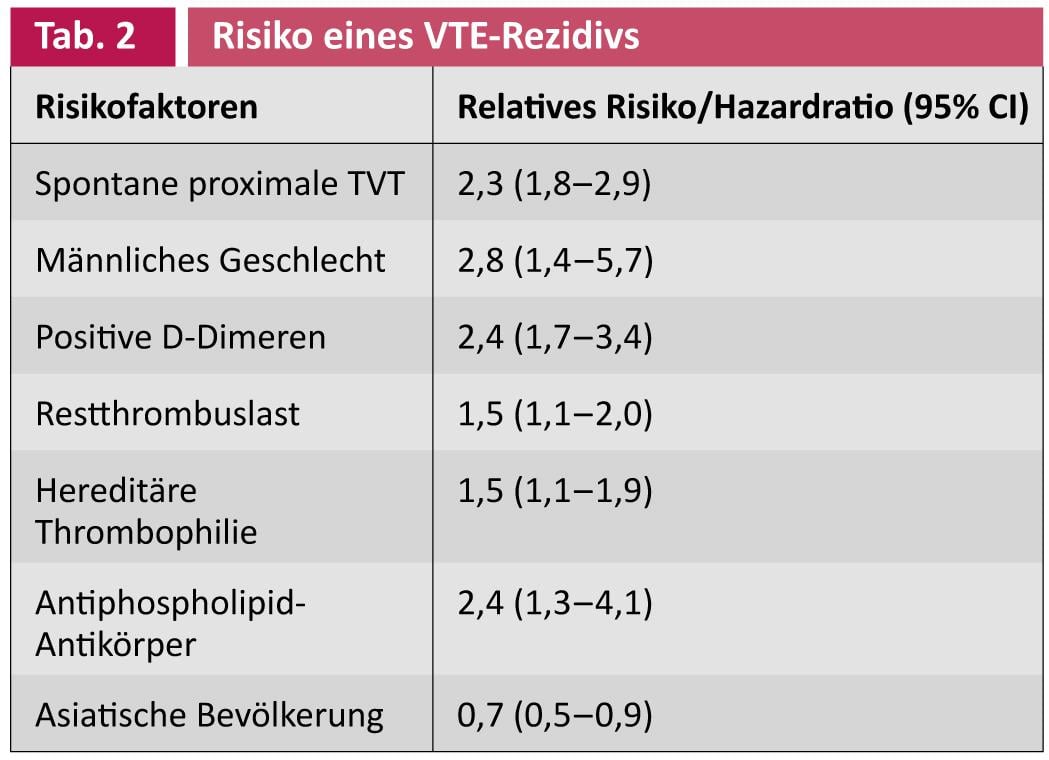
The incidence of severe anticoagulant hemorrhage is in the range of 1-4%/year with intracerebral hemorrhage of 0.4-1.5% depending on the literature and risk population. The following risk factors were associated with increased bleeding: Age >65, previous bleeding, tumor disease with or without metastasis, renal insufficiency, hepatic insufficiency, thrombocytopenia, st. n. stroke, diabetes mellitus, anemia, under comedication with antiplatelet agents, difficult control of AK, alcohol abuse, frequent falls, recent surgery, comorbidity, and decreased functional capacity [3]. Table 2 presents relevant risk factors for recurrent thrombosis and is discussed in more detail below.
Spontaneous proximal DVT
It has been known for many years that patients with spontaneous proximal DVT and/or pulmonary embolism after cessation of oral AK have a much higher risk of recurrent thrombosis than patients with provoked initial thrombosis. In a cohort study, Prandoni et al. in 1626 patients with spontaneous or provoked proximal DVT or pulmonary embolism after discontinuation of AK after a median follow-up of 50 months showed that recurrent thrombosis had occurred in 22.3% of patients after this period. Patients with initial spontaneous thrombosis had the highest risk of thrombosis recurrence compared with provoked thrombosis, with a hazard ratio of 2.3 (95% CI, 1.8-2.9) [4].
Male gender
Several studies have shown that the risk of VTE recurrence is higher in men than in women. In a prospective study of 474 patients with a first proximal spontaneous or provoked DVT with a follow-up of 3477 person-years (mean, 7.3 years), the risk of recurrence was 4.1% person-years in men and 1.6% person-years in women. Men with spontaneous proximal initial thrombosis had a 2.8-fold (95% CI, 1.4-5.7) increased risk of recurrence compared with women [5].
D-dimers
Several studies have shown that patients who develop positive D-dimers one month after discontinuation of oral AK have an increased risk of recurrence. The PROLONG randomized controlled intervention trial demonstrated that patients with spontaneous proximal DVT and a positive D-dimer test one month after stopping AK benefit from restarting AK [6]. In PROLONG, 608 patients had AK discontinued after at least three months and D-dimers measured after one month. D-dimers were elevated in 36.8% of cases. AK was not restarted in patients with negative D-dimers. The patients with elevated D-dimers were randomized into two groups: One group received AK for an additional 18 months; the other group with positive D-dimers did not receive AK again. After an average of 1.4 years of follow-up, 6.2% of patients who had negative D-dimers at baseline had recurrence. Patients with elevated D-dimers without continuation of AK had recurrence of thrombosis in 15.0% of cases. Patients with positive D-dimer test and resumption of AK had recurrence of thrombosis in 2.9% of cases. The hazard ratio for patients with positive D-dimer test without AK was 4.3-fold (95% CI, 1.2-14.6) significantly higher than that for patients with positive D-dimer test with AK. Patients with elevated D-dimers without AK showed a 2.3-fold (95% CI, 1.2-4.5) increased risk of thrombosis compared with those with negative D-dimer test without AK [6].
A meta-analysis of four studies of D-dimer measurement after discontinuation of AK involving 1539 patients with spontaneous VTE confirmed the results of the PROLONG trial: 16.6% of patients with elevated D-dimers after discontinuation of oral AK had recurrent thrombosis at follow-up, whereas only 7.3% of patients with normal D-dimers had recurrent thrombosis. Detection of elevated D-dimers was associated with a 2.4-fold increased risk of recurrence (95% CI, 1.7-3.4) for VTE [7].
Residual thrombus load
After DVT, it takes some time for the vein to recanalize. Siragusa et al. were able to demonstrate in the randomized controlled intervention study DACUS with 258 patients with spontaneous or provoked proximal DVT that after three months of AK a residual thrombus of >40% of the vein diameter was present in 69.8% of the patients [8]. AK was not continued in patients without residual thrombus.
Patients with increased residual thrombus burden were randomized into two groups: One group received AK for an additional nine months, and the other group had AK discontinued. After two years of follow-up, patients who had no residual thrombus at baseline had recurrence in only 1.3% of cases. In contrast, patients with increased residual thrombus burden without continuation of AK had recurrence of thrombosis in 27.2% of cases. Patients with residual thrombi and continuation of AK for another nine months had recurrence of thrombosis in 19% of cases after two years. The hazard ratio for patients with increased thrombus burden without AK was 24.9-fold (95% CI, 3.4-183.6) significantly higher than for patients without thrombus burden. It should be noted here that the confidence interval is very wide, indicating some fuzziness/inaccuracy of the data [8]. A meta-analysis of 14 studies with residual thrombus measurement demonstrated only a small increase in the risk of recurrence (HR: 1.5, 95% CI, 1.1-2.0) [9].
Hereditary thrombophilia
For the common mild forms of thrombophilia, a meta-analysis showed that the relative risk of recurrence was low for the heterozygous factor V Leiden mutation at 1.5 (95% CI, 1.1-1.9) and for the heterozygous prothrombin mutation at 1.4 (95% CI, 1.0-1.8). Because of the only modestly increased risk of recurrence, prolonged AK per se is not warranted [10]. In the 2009 Cochrane analysis, there were no randomized controlled trials evaluating the utility of thrombophilia screening to assess recurrence risk [11]. A 2012 update still found no controlled studies, so no clear recommendation is currently possible in this regard [12].
Antiphospholipid antibody
Patients with antiphospholipid syndrome have a significantly increased risk of recurrent thrombosis. Pengo et al. were able to show in a retrospective study of 160 patients with antiphospholipid syndrome that the hazard ratio for thrombosis recurrence was significantly increased by 2.4-fold (95% CI, 1.3-4.1) in patients in whom AK had been terminated compared with those who had been on long-term anticoagulation [13].
Malignancy
Patients with an active malignancy have an approximately fourfold increased risk of VTE and a sixfold increased risk if they are on chemotherapy [14]. At the same time, there is also an approximately threefold increased risk of increased bleeding. The risk of recurrence of VTE can exceed 27% per year despite therapy with vitamin K antagonists, so long-term AK is recommended if tumor disease is active [15, 16].
Ethnicity
An epidemiologic study in California of more than 23 000 patients with spontaneous or provoked DVT examined the incidence of recurrent thrombosis in different populations. Asians had a 0.7-fold lower risk of recurrence than the white population (95% CI, 0.5-0.9) [17].
Conclusion
Not all patients with VTE are at increased risk of recurrence. Each individual risk factor listed above is important in assessing the risk of recurrence, but is not specific enough per se as a sole parameter (except active malignancy) to make a general recommendation. A combination of these risk factors may be important [18]. As an example, consider a patient who was anticoagulated for three months after spontaneous proximal DVT. Now the question is how long the AK should continue. The 9th ACCP Guidelines do not help much in this regard. Decision making for duration of therapy lies in the absolute risk of recurrence. Assuming that the absolute risk of recurrence is conservatively estimated to be 2-4% per year and the patient is a male, the absolute risk increases 2.8-fold due to the relative risk increase, i.e., to approximately 6-11% per year. If one has other risk factors (Tab. 2), these can be combined. The increase in the risk of recurrence to approximately 6-11% per year may already be sufficient to warrant continuation of AK and must be weighed against the individual risk of severe bleeding.
Should the patient wish to discontinue AK for VTE after three to 12 months, urgent consideration should be given to 100 mg of aspirin daily for three years, as ASA was shown to reduce the risk of VTE recurrence by 32% and vascular events (arterial and venous) by 34% in the combined ASPIRE and WARFASA trial, with no increase in major bleeding [19].
Literature:
- White RH: The epidemiology of venous thromboembolism. Circulation 2003; 107: 14-18.
- Guyatt GH, et al: Executive summary: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141: 7S-47S.
- Kearon C, et al: Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis,9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141: e419S-494S.
- Prandoni P, et al: The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica 2007; 92: 199-205.
- Christiansen SC, et al: Sex difference in risk of recurrent venous thrombosis and the risk profile for a second event. J Thromb Haemost 2010; 8: 2159-2168.
- 6 Palareti G, et al: D-dimer testing to determine the duration of anticoagulation therapy. N Engl J Med 2006; 355: 1780-1789.
- Siragusa S, et al: Residual vein thrombosis to establish duration of anticoagulation after a first episode of deep vein thrombosis: the Duration of Anticoagulation based on Compression UltraSonography (DACUS) study. Blood 2008; 112: 511-515.
- Carrier M, et al: Residual vein obstruction to predict the risk of recurrent venous thromboembolism in patients with deep vein thrombosis: a systematic review and meta-analysis. J Thromb Haemost 2011; 9: 1119-11125.
- Marchiori A, et al: The risk of recurrent venous thromboembolism among heterozygous carriers of factor V Leiden or prothrombin G20210A mutation. A systematic review of prospective studies. Haematologica 2007; 92: 1107-1114.
- Cohn D, et al: Thrombophilia testing for prevention of recurrent venous thromboembolism. Cochrane Database Syst Rev 2009: CD007069.
- Cohn DM, et al: Thrombophilia testing for prevention of recurrent venous thromboembolism. Cochrane Database Syst Rev 2012; 12:CD007069.
- Pengo V, et al: Clinical course of high-risk patients diagnosed with antiphospholipid syndrome. J Thromb Haemost 2010; 8: 237-242.
- Heit JA, et al: Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 2000; 27 (160): 809-815.
- Lindhoff-Last E: Risk assessment of recurrence of venous thromboembolism. Hemostaseology 2011; 31: 7-12.
- Akl EA, et al: Anticoagulation for the long term treatment of venous thromboembolism in patients with cancer. Cochrane Database Syst Rev 2008: CD006650.
- White RH, et al: Incidence of idiopathic deep venous thrombosis and secondary thromboembolism among ethnic groups in California. Ann Intern Med 1998; 128: 737-740.
- Eichinger S, et al: Risk assessment of recurrence in patients with unprovoked deep vein thrombosis or pulmonary embolism: the Vienna prediction model. Circulation 2010; 121: 1630-1636.
- Brighton TA, et al; ASPIRE Investigators: Low-dose aspirin for preventing recurrent venous thromboembolism. NEJM 2012; 367: 1979-1987.
CARDIOVASC 2013; 12(1): 4-7











