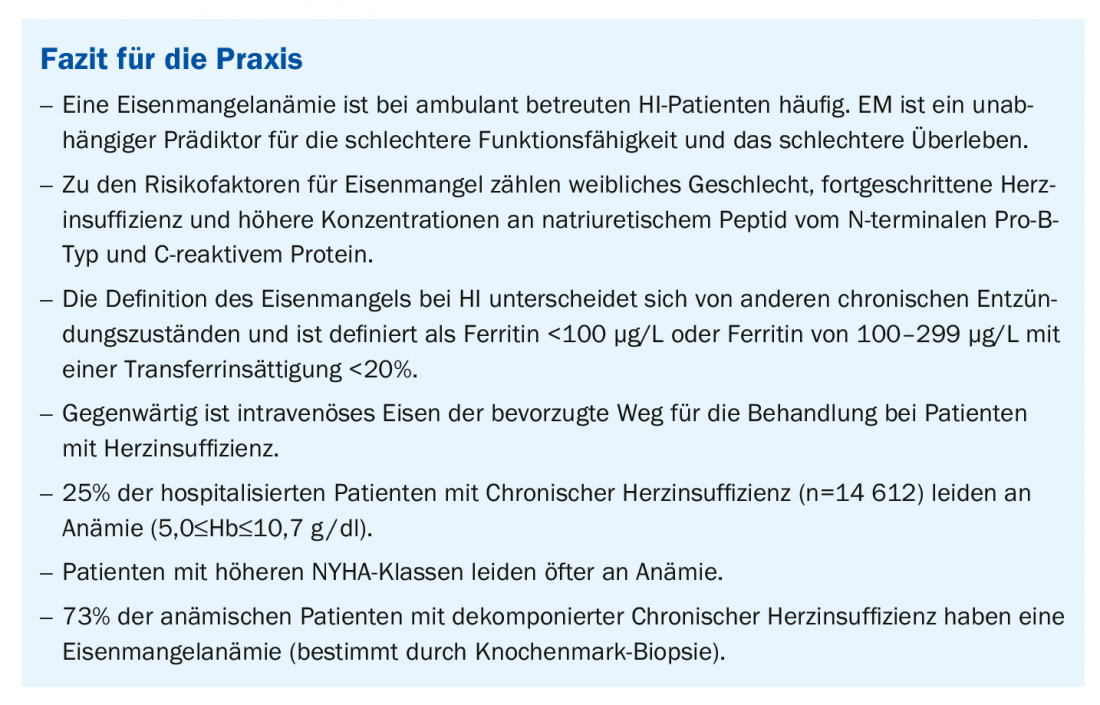
Iron deficiency is a common comorbidity in patients with heart failure and has been associated with increased mortality and hospitalizations. The benefits and safety of iron supplementation were examined in a meta-analysis.
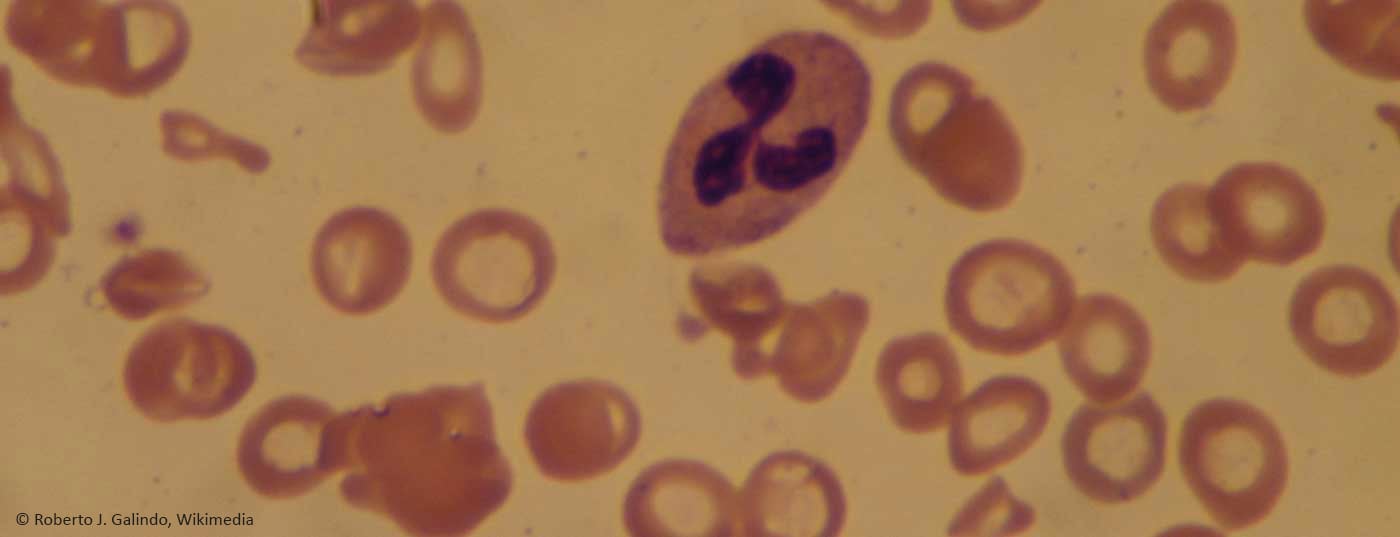
(Red) The prevalence of EM is often underestimated. Despite apparently adequate iron stores assessed by serum levels of iron and ferritin, up to three quarters of patients with anemia, normal renal function, and advanced HI have EM based on bone marrow aspiration results. Iron is necessary for optimal hematopoiesis, but also plays a central role in oxygen transport (hemoglobin), storage (myoglobin), cardiac and skeletal muscle metabolism, synthesis and degradation of proteins, lipids, ribonucleic acids, and mitochondrial function. Cardiac iron uptake and intracellular iron handling are essential for cardiac function. The iron in circulation is transported by transferrin, which keeps the iron in a non-reactive state.
Pathophysiology and epidemiology
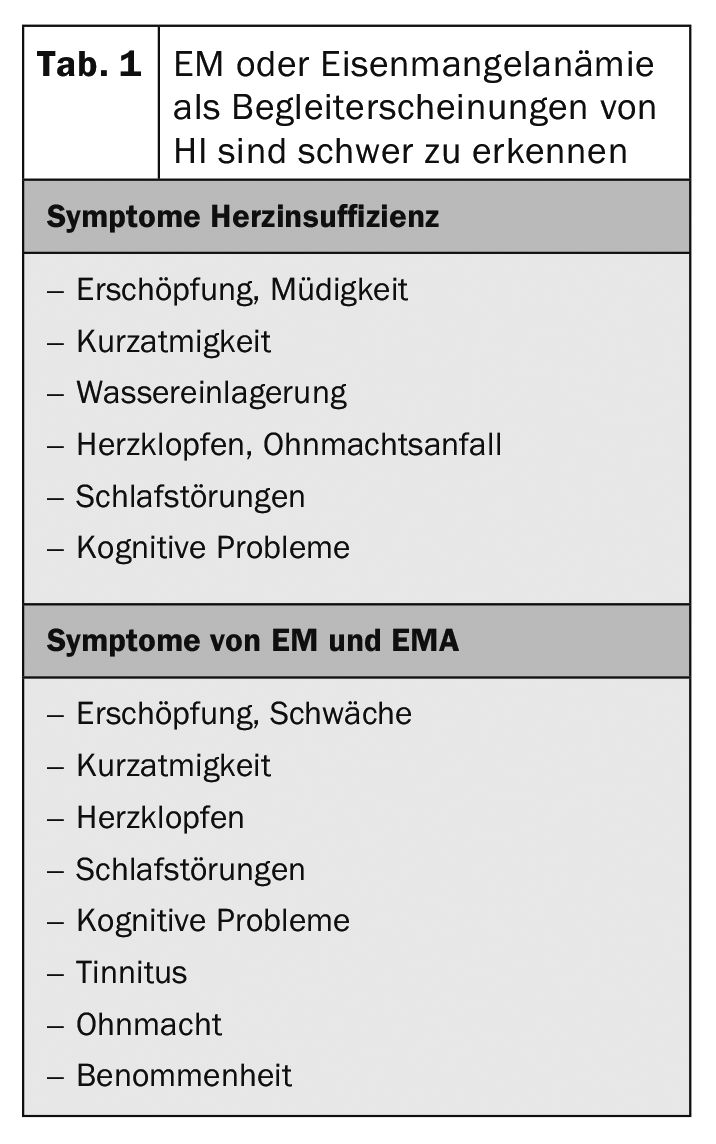
The pathophysiology of EM with HI is likely multifactorial. When patients with HI are diagnosed with EM, it is important not to overlook other causes such as gastrointestinal ulcers or malignancies. There may be simple factors, such as blood loss due to antiplatelet or anticoagulation therapy, that lead to iron loss. Malabsorption may also play a role. In addition, interstitial intestinal edema may result in decreased oral iron absorption. Overloading the liver can also have an impact. The chronic inflammatory state associated with HI results in elevated levels of pro-inflammatory cytokines such as interleukin-6 (IL-6). Inflammation induces the synthesis of hepcidin, reducing the release of stored iron. While most chronic inflammatory diseases are associated with higher hepcidin levels, studies in HI patients have shown that advanced HI is associated with lower hepcidin levels and does not appear to correlate with IL-6 in this patient group. This may be due in part to increased erythropoietin levels associated with advanced HI, as well as hepicidin suppression (Table 1).
Intravenous supplementation
Oral iron is poorly absorbed, especially in patients with chronic diseases such as HI. Adverse gastrointestinal effects limit tolerability. Several months of oral iron therapy would be required to replicate EM in HI, typically requiring ≥1000 mg. In contrast, only a few i.v. injections are required to achieve a significant increase in markers of iron stores. I.v. iron replacement bypasses the gastrointestinal tract and improves the absorption of iron. Several small studies have suggested a potential benefit of i.v. iron in HI patients.
Source: Iron Academy 2019
HAUSARZT PRAXIS 2019; 14(5): 36
CARDIOVASC 2019; 18(5): 26