Up to 5% of children and adolescents in German-speaking countries live with diseases of the respiratory tract – especially the lungs – and have drug therapy in case of exacerbations, but also in the symptom-free interval. Despite all the advantages of inhalative application, this is not possible in some cases, especially in younger children, so that systemic application is certainly justified.
Up to 5% of children and adolescents in German-speaking countries live with diseases of the respiratory tract – especially the lungs – and have drug therapy in case of exacerbations, but also in the symptom-free interval.
Medications may be administered systemically or locally in the form of inhaled agents, although the advantages of inhaled administration usually outweigh the disadvantages. With inhaled therapy, the active substance is deposited locally directly at the site of action and is absorbed systemically only to a very small extent, with correspondingly low systemic or local side effects. In contrast, systemically administered active ingredients act equally throughout the body, with the consequence that significantly larger doses of active ingredient must be introduced systemically in order to achieve a sufficient effect at the target site – in this case, the lungs. This ultimately leads to significantly higher side effect rates. Despite all the advantages of inhalative application, this is not possible in some cases, especially in younger children, so that systemic application is certainly justified.
The success of inhalation therapy, i.e. whether the affected child’s health really improves and the conditions for age- and development-appropriate participation and quality of life can be achieved, depends on various factors:
- Were the correct diagnostics performed and is the diagnosis correct?
- Was the correct agent prescribed at the correct dose?
- Has the correct inhalation device been selected?
- Does the patient master the correct inhalation technique?
- Does the patient take the medication according to the prescription (regularly, if applicable)?
Each of these factors must be met for therapy to be successful – if just one of these factors is neglected, improvement in health is at risk. The two aspects of proper diagnostics and the need for the right agent will not be discussed further here.
In quite a few cases, it can be observed that despite an apparently correct diagnosis and the selection of the right active substance, there is no improvement in the patient’s state of health. Experience from practice shows that in the overwhelming majority of cases this is because the patient is
- should inhale with an inhalation device that is not suitable for him,
- the inhalation device is operated incorrectly and the inhalation maneuver is faulty or
- the patient inhales only irregularly or not at all.
In the following, these three aspects are considered in a more differentiated way.
Importance of choosing a suitable inhalation device
Children differ significantly from adults in terms of the anatomy of their respiratory organs, respiratory physiology, and motor skills. Even within the same age group, the level of development, motor skills, coordinative abilities, and respiratory physiology can vary greatly from child to child. As a result, children may not be able to use some inhalers (devices) properly for motor, physiological and, in some cases, cognitive reasons. For example, children usually do not manage to apply a sufficiently high inspiratory suction to operate powder inhalers (DPI) in such a way that deagglomeration of the drug agglomerates occurs reliably. Similarly, with metered dose inhalers (MDIs), children usually do not manage the coordination between exhalation, inhalation, triggering of the spray burst, and slow inhalation flow correctly. The selection of the right inhalation device contributes decisively to the success of inhalation therapy. The advantages and disadvantages of common inhalation systems presented in Table 1 provide initial guidance on their suitability in children.
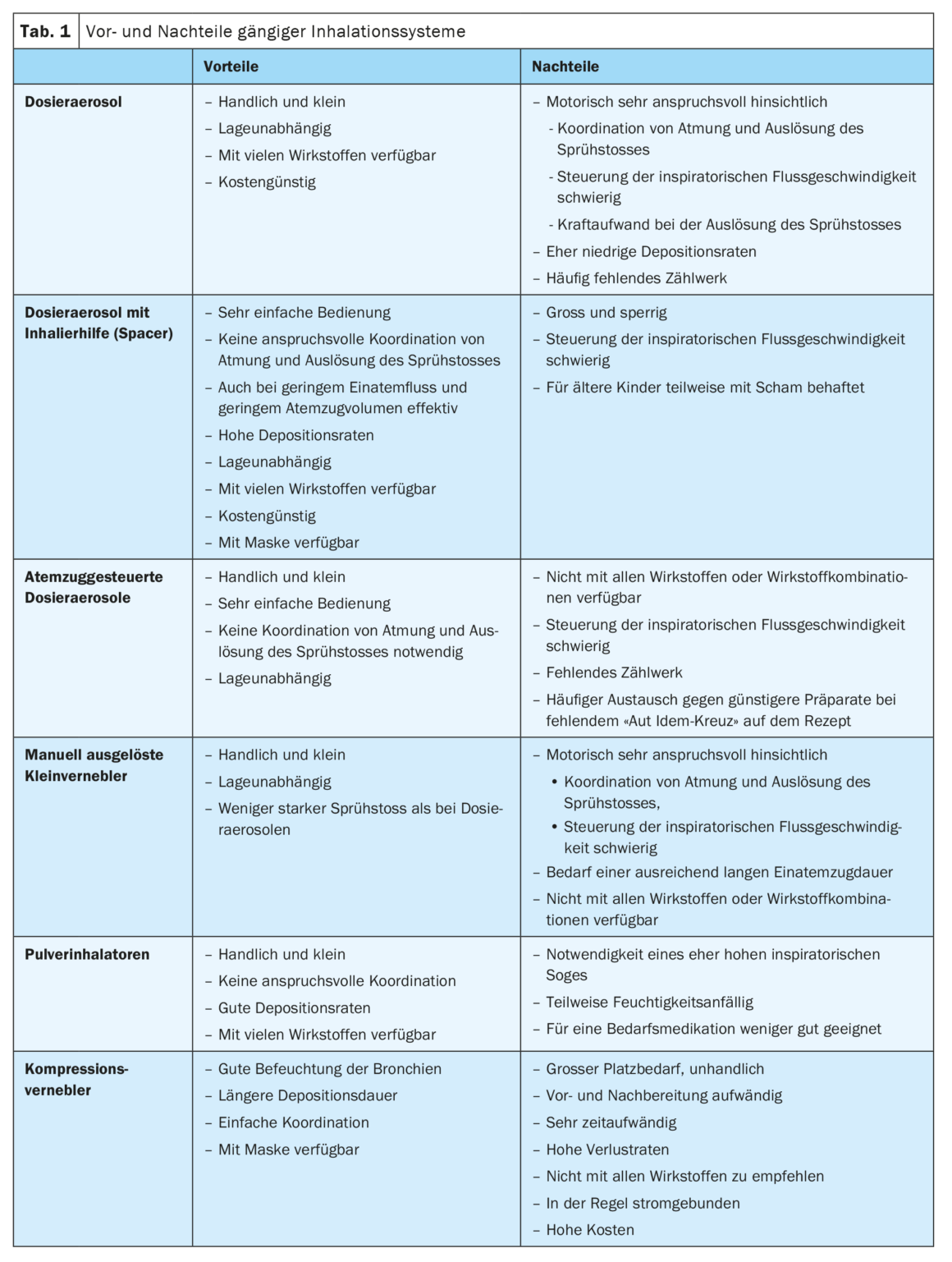
Features, advantages and disadvantages of spray inhalers
In general, it can be said that metered dose inhalers and manually triggered small nebulizers are unsuitable for children up to about 12 years of age, as the coordination of inhalation and exhalation, air holding, triggering of the spray burst and control of a slow inspiratory flow rate is too demanding and often not mastered even by adults. In addition, children usually do not have the necessary finger strength to trigger the spray by pressing down on the active ingredient container. Thus, there is a risk of delivering too small a quantity of active ingredient or none at all, or of triggering the spray burst at a time that is poorly coordinated with inhalation.
Metered dose inhalers with spacers place the least demands on the user’s coordination and breathing technique. They can be used with quiet slow breathing even with a low breath volume without restrictions. Even in very young children, inhalation is possible if necessary with the aid of a tight-fitting mask. Thus, metered dose inhalers with inhalation aids are excellently suited for almost all age groups and generally ensure good and reliable deposition of the active ingredient with the fewest possible side effects. An inhaler should have a sufficient but also not too large volume of about 150-230 ml, an inhalation valve that prevents exhaled air from breathing back into the chamber, and a universal flexible attachment that is compatible with various metered dose inhalers.
In the case of breath-triggered spray inhalation systems or breath-triggered metered-dose inhalers, the active ingredient is delivered automatically without manual triggering by inhalation flow alone. The mechanisms used ensure that the aerosol is automatically delivered through the mouthpiece at the correct time shortly after inhalation begins. For this purpose, an inspiratory flow rate of approx. 20 l/min is already sufficient, so that the triggering of the spray burst is ensured even during an exacerbation with low respiratory flow rates. The devices are handy and small, insensitive and particularly well suited for demand therapy. Children from about 6 and most from 9 years of age are able to use appropriate preparations well. Due to the small format and the rather low demand on coordination and breathing technique, they are a good alternative for children. Since most exchanges of prescribed inhalants under rebate contracts involve the exchange of breath-triggered metered-dose inhalers to metered-dose inhalers (without an inhaler), it is recommended that the exchange be prohibited when a breath-triggered device is prescribed.
Special features, advantages and disadvantages of powder inhalation devices
Powder inhalers are generally unsuitable for children up to 8 years of age and also still for many older ones, as they require a rather high inspiratory suction for the deagglomeration of the active substance agglomerates in the device. Younger children usually cannot apply this, so that the non-deagglomerated large active ingredient particles then already impacted in the throat and at the latest in the large bronchi and hardly reach the smaller bronchi. This drastically reduces deposition at the site of action and can lead to side effects such as thrush in the throat. When prescribing a powder inhaler, it must therefore be regularly checked whether the inspiratory suction is sufficiently high. The test whistles provided by the pharmaceutical companies are not suitable for a meaningful objective examination of the flow. Using the “In-Check Dial” test device, a simple, fast and relatively reliable statement can be made about the applied inspiratory flow and the suitability of various powder inhalation devices.
Although the compression nebulizers, which are in fact very frequently prescribed, have the great advantage of humidifying the lungs with the effects of liquefying and loosening secretions, they are less suitable for the daily administration of active substances because of the time required, the complicated preparation and cleaning, and the low deposition rates. It usually takes 10-15 minutes to inhale a full dose of active ingredient. During this inhalation period, it must be ensured that the child inhales slowly (and at best with a short pause for breath), if possible continuously with a straight head, carefully through the mouth with complete lip closure (or tightly fitting mask). This is hardly possible in children, which is why this form of inhalation of active substances – especially steroids – is rather unsuitable and significantly more ineffective than, for example, inhalation with metered-dose inhalers and inhalation aids. Nevertheless, the compression nebulizer has its place because of the good humidification of the lungs. Inhalation with NaCl is helpful in many respiratory diseases. For example, it may be recommended to administer the active substance with a metered-dose inhaler and an inhalation aid and subsequently to moisten the bronchi via NaCl inhalation with the compression nebulizer in order to loosen the secretion.
For inhalations with a mouthpiece, it must be ensured that the mouthpiece is completely enclosed tightly with the lips without a gap and that
inhalation takes place exclusively through the mouth and not additionally through the nose. If this cannot be ensured, metered dose inhalers with an inhalation aid as well as compression nebulizers with a mouth-nose mask can be used. Care should be taken to choose the right size and the mask should preferably be made of a soft material that adapts well to the contours of the face without exerting much pressure. The mask must fit on the face completely without gaps or open areas. Even a small gap between the face and the mask significantly reduces deposition rates. Since even with a correctly used mask, higher loss rates of the active ingredient occur than with mouthpiece inhalation, children should be switched from mask to mouthpiece as early as possible.
be The use of a nose clip can be helpful, as long as it is tolerated by the child.
Other pitfalls in prescribing and instructing inhalation devices
Special consideration should always be given when different inhalers for different active ingredients are prescribed at the same time. This is the case, for example, in some indications that require continuous therapy (for example, with a steroid) with simultaneous demand therapy (for example, with a beta-2 mimetic). In these cases, a powder inhaler is often used for continuous therapy (good deposition rates, easy coordination, etc. in children from about 8 years of age) and a spray inhaler is used for on-demand medication (e.g., with a handy and easy-to-use breath-controlled metered-dose inhaler). However, since powder inhalers tend to require higher inspiratory flow rates, whereas spray inhalers require the slowest possible inspiratory flow, there is a risk that after rapid inhalation with the powder several times a day, the spray will be inhaled with too rapid an inspiratory flow if necessary, and the then high impaction of the aerosol in the throat will lead to a massive reduction in the deposition rates in the bronchi and a correspondingly poor effect.
Especially in very young children, inhalation is individually challenging. Since it is not uncommon for patients to be afraid of inhalation or at least very skeptical, instructors as well as parents and caregivers must act with particular sensitivity and creativity. In particular, if the child cries or screams during inhalation, the active ingredient will not reach the site of action sufficiently, as the intrathoracic pressure is high and breathing is compressed and shallow. It is the task of the instructors and caregivers to playfully reassure the child and give him great security, so that inhalation occurs via calm and relaxed breaths without crying or screaming.
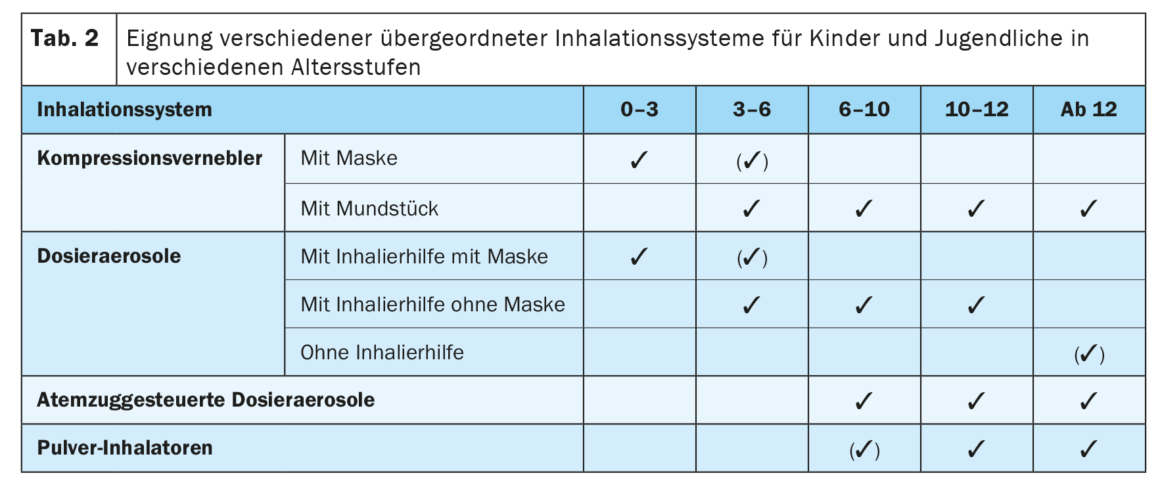
Last but not least, very individual aspects concerning the child’s motivation must be taken into account when selecting the right inhalation device. Children often do not make rational-objective decisions about performing health-related actions or behaviors, but rather subjective and perceived irrational decisions. Therefore, in some cases, for example, the child may be uncomfortable or embarrassed by the color or shape of the inhaler, fear teasing, and therefore not inhale publicly when needed. An unpleasant taste may cause refusal to inhale. And if the inhalation maneuver is too complex, too complicated or takes too long, this can also lead to refusal or at least to poor execution with a correspondingly poor effect. In such cases, if possible, the child’s behavior should be respected and an alternative inhalation system for the necessary medication should always be constructively sought. Table 2 provides a rough guide as to which inhalation devices are good or not suitable for children at which age.
Importance of detailed instruction or teaching of inhalation technique appropriate to target group
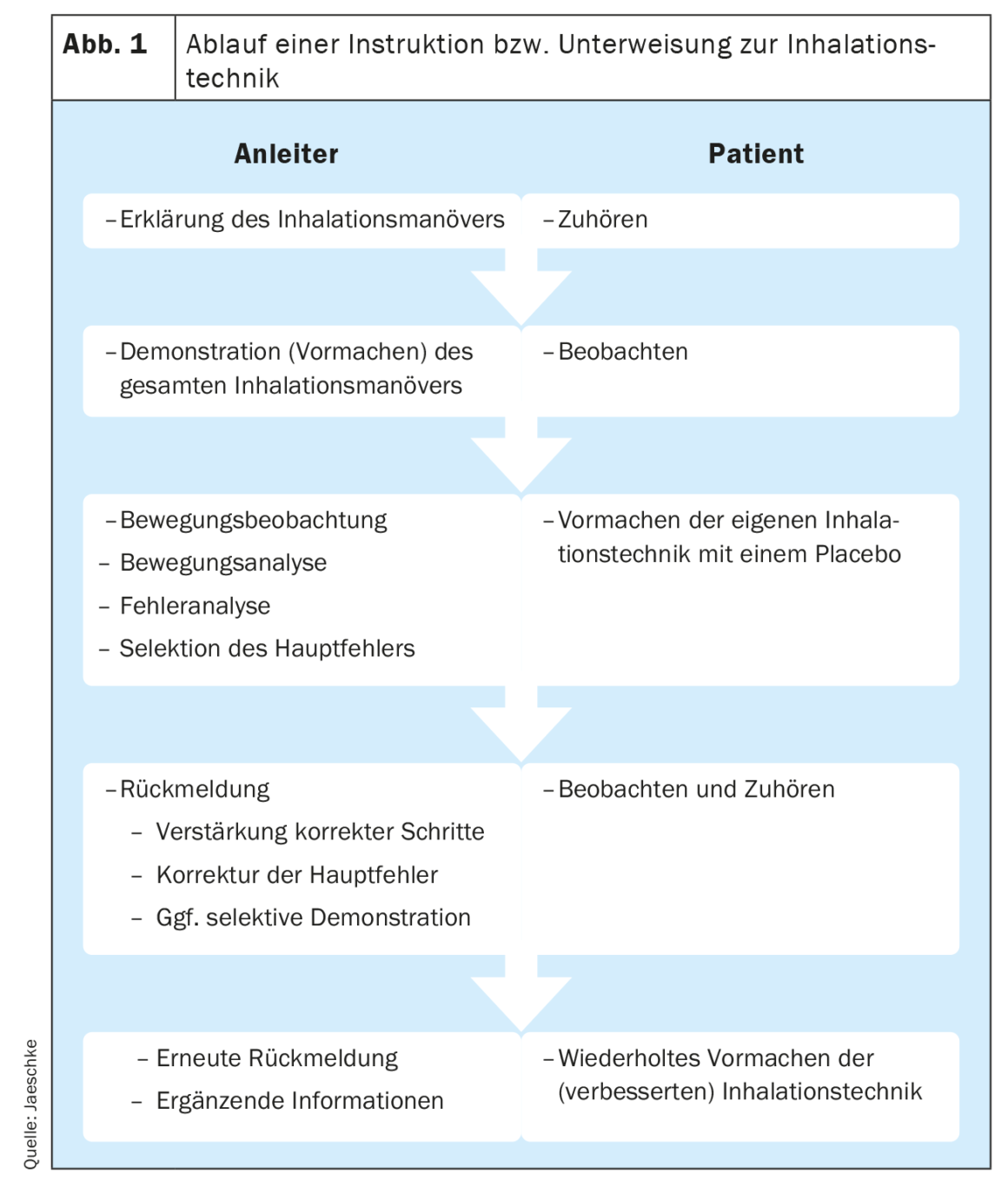
A prerequisite for the best possible effect of the administered medication is a correct and error-free inhalation technique. Inhalation itself, or the inhalation maneuver, is a complex motor process that places high demands on the coordination of breathing, posture and operation of the inhalation device. Therefore, after selecting the appropriate inhaler, learning the correct inhalation technique is of great importance. This should always be done face-to-face with children by an experienced professional.
This instruction, or inhalation instruction, includes.
- the age-appropriate explanation of the inhaler,
- the explanation of the sequence of the individual steps of the inhalation maneuver,
- detailed demonstration of the inhalation maneuver by the instructor, and
- the observed implementation by the patient with correction by the instructor.
After the brief explanation, the demonstration should be precise, at a slow pace, highlighting each step and exaggerating particular aspects of the inhalation maneuver. If the patient subsequently attempts to perform the inhalation maneuver himself using a placebo device, the instructor has the task of attentive observation with movement and error analysis. After analyzing the individual steps of inhalation and identifying correct and incorrect ones, the child should first be authentically praised for what he or she has already done correctly. Subsequently, the main error is addressed first and only then, if necessary, other errors are addressed, corrected, and selectively demonstrated again by the instructor. Then, the child should practice repeatedly and be observed by the instructor until he or she perfectly masters the inhalation technique to ensure success of the inhaled therapy. Figure 1 shows the sequence of instruction or inhalation instruction.
Eliciting motivation to carry out the therapy on a regular basis
Once the right active ingredient has been prescribed in the appropriate device for the child and the inhalation technique has been instructed and practiced until the child masters it flawlessly, a sufficiently high level of motivation and structuring is also required so that the child really does perform the therapy regularly in everyday life.
For this purpose, it is important to show the child what possibilities and perspectives open up to him or her through good and regular inhalation therapy. It must develop intrinsic motivation, i.e., motivation emanating from the child, to perform the inhalations regularly and reliably. Techniques of motivational interviewing can be helpful here. The aim is for inhalation to have a fixed routine place in the child’s or family’s daily routine and for it to be part of the morning routine or evening procedure as a matter of course in the sense of a ritual.
The parents or caregivers of those affected play an important role in ensuring that they take the medication regularly, and they must therefore also be instructed accordingly in any case. A written, understandable, possibly illustrated therapy plan is essential here.
If the possibilities of instruction and inhalation teaching are not sufficient for this purpose, the child or family should be referred to qualified asthma training (e.g. facilities that train according to the guidelines of the Arbeitsgemeinschaft Asthmaschulung im Kindes- und Jugendalter e.V.).
Conclusion
The success of inhalation therapy in children depends to a large extent on the selection of the right inhalation device, on good and comprehensive age-appropriate instructions, and on the child’s intrinsic motivation to perform the therapy regularly. Careful selection of the inhalation device is a basic prerequisite for all further steps. Prescribers must be sensitive, targeted, and consistent in actively perceiving the individual circumstances and conditions of each patient and taking these into account when selecting suitable devices and weighing up the advantages and disadvantages. Instruction and guidance with joint practice are essential and should be mandatory for each new prescription as well as at regular follow-up appointments. Ultimately, a drug applied by inhalation is effective only to the extent that it is deposited at the site of action.
Professionals should undergo extensive training in this regard in pharma-independent continuing education courses for practitioners. The asthma academies of the Arbeitsgemeinschaft Asthmaschulung im Kindes- und Jugendalter e.V.(www.asthmaschulung.de), among others, offer such training.
Take-Home Messages
- A drug applied by inhalation is effective only to the extent that it is actually deposited in the lungs at the target site.
- The success of inhalation therapy in children depends to a large extent on the selection of the right inhalation device.
- Each child has different motor, cognitive and motivational prerequisites and abilities, so the choice of inhaler must always be made individually.
- Professional, comprehensive, personalized age-appropriate guidance face-to-face is essential.
- A written therapy plan should always be given to the children and adolescents and their caregivers.
- The child’s motivation to take it regularly must not be neglected.
- Comprehensive hands-on training of instructors, prescribers and
other medical and pharmaceutical professionals should
be mandatory.
Literature:
- Lin HL, Wan GH, Chen YH, et al: Influence of nebulizer type with different pediatric aerosol masks on drug deposition in a model of a spontaneously breathing small child. Respir Care 2012; 57(11): 1894-1900.
- Iramain R, Castro-Rodriguez JA, Jara A, et al: Salbutamol and ipratropium by inhaler is superior to nebulizer in children with severe acute asthma exacerbation: randomized clinical trial. Pediatr Pulmonol 2019; 54(4): 372-377.
- Braido F, Chrystyn H, Baiardini I, et al: “Trying, But Failing” – The Role of Inhaler Technique and Mode of Delivery in Respiratory Medication Adherence. J Allergy Clin Immunol Pract 2016; 4(5): 823-832.
- Schultz A, Le Souëf TJ, Venter A, et al: Aerosol inhalation from spacers and valved holding chambers requires few tidal breaths for children. Pediatrics 2010; 126(6): e1493-e1498; doi: 10.1542/peds.2010–1377.
- Sanchis J, Gich I, Pedersen S.: Aerosol Drug Management Improvement Team (ADMIT). Systematic Review of Errors in Inhaler Use: Has Patient Technique Improved Over Time? Chest 2016; 150 (2): 394-406.
- Plaza V, Giner J, Rodrigo GJ, et al: Errors in the Use of Inhalers by Health Care Professionals: A Systematic Review. J Allergy Clin Immunol Pract 2018; 6(3): 987-995.
- Castro-Rodriguez JA, Rodrigo G: Agonists through metered-dose inhaler with valved holding chamber versus nebulizer for acute exacerbation of wheezing or asthma in children under 5 years of age: a systematic review with meta-analysis. J Pediatr 2004; 145: 172-177.
- Sakrani NF, Hussein SE, Borg M, Konstantinopoulou S: Assessing and addressing barriers toward MDI use in acute asthma exacerbations at a tertiary pediatric ED in the United Arab Emirates. Int J Pediatr Adolesc Med 2022; 9(1): 41-45.
- Wildhaber J, Kamin W. (eds.): Inhalation therapy in childhood and adolescence. 2nd ed. UNI-MED Verlag aG. Bremen 2010.
InFo PNEUMOLOGY & ALLERGOLOGY 2023; 5(1): 8-13.











