Iron deficiency is not only common in malignancies, but also a risk factor for impaired efficacy of antitumor treatment. Accordingly, transferrin saturation should be kept in view and iron supplementation should be started in time.
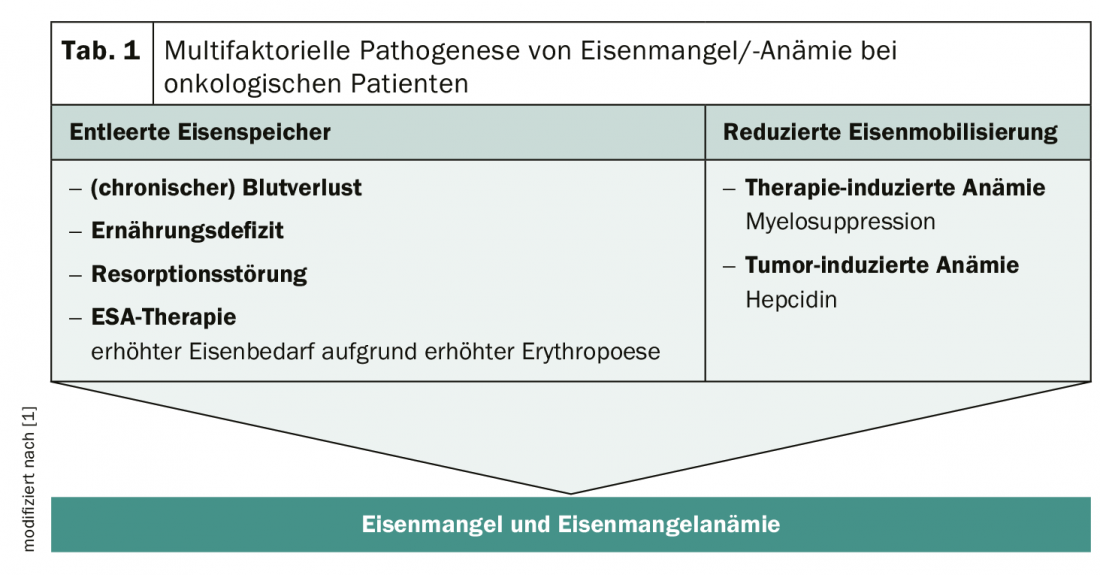
The body’s iron stores are literally depleted by tumor diseases and their treatment with intensive chemotherapy. As a consequence of chronic inflammation, proinfllammatory cytokines such as IL-6 are increasingly released. As a result, the liver produces more hepcidin, which slows down iron absorption in the intestine and at the same time reduces iron mobilization. This results in an inflammation-related iron deficiency, which, depending on its severity, can lead to anemia. In addition, oncological patients suffer from depleted iron stores (Tab. 1). In general, the higher the grade of the tumor, the greater the risk of anemia for the patient. But anemic patients are three times more likely to experience dose reductions and treatment interruptions, limiting the effectiveness of anti-tumor therapy. This also increases the risk of recurrence and decreases the overall survival rate. In addition, symptoms such as fatigue, impairment of the immune system and cognitive dysfunction place an additional burden on those affected. The higher the iron deficiency, the lower the quality of life of individuals on therapy.
Act early
Studies show that increasing hemoglobin levels are associated with increasing quality of life. In general, an Hb value between 11 and 13 g/dL is considered optimal to achieve a sufficiently good level of quality of life. Accordingly, iron deficiency should be detected and treated in time, before the Hb value drops too much. An important marker of iron saturation is transferrin saturation (TSAT). In oncology patients, the reference values according to ESMO guidelines for functional iron deficiency are TSAT <20% and serum ferritin values >100 μg /ml. From an Hb <12 g/dl (women) or 13 g/dl (men), a TSAT <20% and serum ferretin values <100 μg/ml one speaks of an iron deficiency anemia with an absolute iron deficiency. The current S3 guidelines on supportive therapy also advocate close monitoring of iron status. According to their recommendation, a determination of transferrin saturation (TSAT) should still take place before the start of chemotherapy.
Effectively compensate for undersupply
There are several options available to compensate for the deficiency quickly and effectively. In acute care, a blood transfusion may be necessary. However, this should be used only in exceptional cases that increases mortality and the risk of infection and thromboembolic complications. The administration of erythropoiesis-stimulating agents (ESA) is another option to which a majority of patients respond well. However, the risk of thrombosis increases. Iron substitution is also effective and can be given orally or i.v. and also in combination with ESA. However, oral administration requires certain clinical prerequisites, as the absorption capacity in the intestine may be significantly reduced by the inflammation.
Source: 34th German Cancer Congress (DKK)
Literature:
- Aapro M, et al: Prevalence and management of cancer-related anemia, iron deficiency and the specific role of i.v. iron. Ann Oncol 2012; 23: 1954-1962.
InFo ONCOLOGY & HEMATOLOGY 2020; 32 (published 4/24/20, ahead of print).