Laser plays an important role in pigmented and vascular lesions. Breast cancer patients with chronic radiation dermatitis and telangiectasia in particular also benefit.
Various laser systems are suitable for the treatment of hyperpigmentation caused by skin aging or exposure to light, with the choice depending on skin type, pigment depth and accompanying lesions (e.g. vascular lesions, actinic keratoses). For deep-lying dermal pigment, a laser with a longer wavelength is selected. Short-pulsed, Q-switched (QS) lasers are most commonly used, e.g., QS Nd:YAG (532 or 1064 nm), Ruby laser (694 nm), or Alexandrite laser (755 nm). Other systems that can be used include flash lamps (Intense Pulsed Light, IPL), picosecond lasers (532, 755, 1064 nm) or fractional ablative lasers, reported Kristine Heidemeyer, MD, Bern.
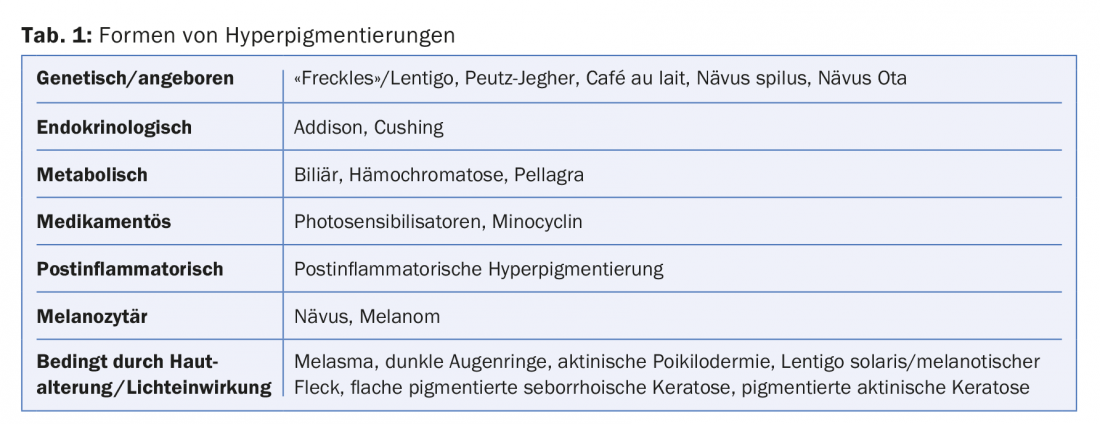
Different forms of hyperpigmentation are shown in Table 1.
Treatment of lentigines and flat seborrheic keratoses
For the treatment of lentigines or flat seborrheic keratoses, the QS Nd:YAG with frequency doubling (532 nm) is suitable. Treatment can also be performed with the flash lamp or, if available, with the picosecond laser (532 or 755 nm). One to three sessions are required with each of these three treatment systems. With the two laser systems, almost complete fading can be achieved. After treatment with the picosecond laser, the treated area is only whitish in color and slightly swollen for a few hours, while healing takes three to four days after flash lamp therapy and up to seven days after laser treatment with QS Nd:YAG, the speaker said. Patients should be instructed not to remove crusts to prevent possible scarring. The most common complications of treatment are post-lesion hyperpigmentation. In this regard, dark skin type and diffuse dyschromia are at increased risk. Consistent sun protection for four weeks is important.
Before lentigines are treated with laser, a thorough examination with a dermoscope should always be performed to avoid missing the diagnosis of lentigo maligna. Recently, patients with biopsy-confirmed lentigo maligna (melanoma in situ on sun-damaged skin) or with invasive lentigo maligna melanoma were retrospectively studied to determine how frequently the lesion had been erroneously treated cosmetically by dermatologists before correct diagnosis [1]. In 7.4% of the 503 patients studied, dermatologists had previously performed aesthetic treatments, most commonly cryotherapy and laser treatments [1].
Pigmented actinic keratoses, dark circles under the eyes, melasma
The two-dimensional treatment of pigmented actinic keratoses by means of PDT (photodynamic therapy) often also has a favorable effect on the pigment, the lecturer reported. The good cosmetic result, the response rate of 70-90% and the influence of the field carcinization by the areal treatment speak for the PDT of pigmented actinic keratoses. Disadvantages of PDT are the pain and the effort. Alternatively, treatment with an ablative laser or – although less successful – with a QS pigment laser can be considered.
In the case of dark circles under the eyes, it is very important to clarify the cause, because often it is not pigment deposits. Loss of volume may result in shadowing, or thinning of the skin may result in increased shining through of the vessels. However, if pigmentary deposits are indeed present (e.g., dark skin type, postinflammatory hyperpigmentation after eczema, drug-induced, hemosiderin), a Q-switched pigment laser (e.g., QS Nd:YAG, QS Ruby) or the picosecond laser can be used for treatment [2].
In melasma, which forms in cases of genetic disposition and under the influence of hormones and UV light, both epidermal and dermal pigment is present. Short-wave visible light also has an effect on lesions, the speaker said. The fact that there is also a vascular component (more and larger vessels in the melasma) is important for laser therapy, he said. However, laser is not the first-choice treatment for melasma. She treats melasma topically with Pigmanorm® for three to four months in Bern. Irritation must be avoided, otherwise post-lesion hyperpigmentation may occur. To prevent this, the treatment must be reduced immediately. If topical therapy is unsuccessful, the speaker applies exfoliation followed by topical therapy. If this is not successful either, she uses pulsed dye laser (PDL) for light skin types. She cited the publication of a prospective randomized split-face study from France that compared treatment with bleaching cream (hydroquinone 4%, tretinoin 0.05%, fluocinolone acetonide 0.01%) combined with PDL on one half of the face with cream treatment alone on the other half of the face for four months from the end of winter [3]. A follow-up inspection took place after the first summer. The aim of the three dye laser treatments, each three weeks apart, was also to influence the vascular component of melasma. Combined therapy did not achieve a higher response, but a lower recurrence rate, the speaker said. Maintenance therapy following induction therapy is very important and consists of cosmetic bleaching creams and consistent protection from UV and visible light (mineral filters even for dark skin types).
Laser treatment of vascular lesions
In 1983, Rox Anderson reported in a groundbreaking publication in Science on the “selective photothermolysis” he developed, which allows light rays to be used therapeutically without simultaneously burning the skin [4]. Visible light can penetrate water – and that’s what skin is mainly made of – very well without being absorbed, said Hans-Joachim Laubach, MD, president of the European Society for Lasers and Energy Based Devices (ESLD), Geneva. However, as soon as a laser beam with a wavelength of the visible light spectrum hits a structure with color instead of water, the absorption behavior changes. Hemoglobin strongly absorbs visible light from 560 to 600 nm. With a dye laser from this wavelength range, at low penetration depths (approx. 0.5 to 1 mm) fine, superficial vessels are treated. Only hemoglobin is selectively heated by photon absorption. Approximately 107°C is reached in the process. The resulting gas causes the small vessel to explode without significantly heating the surrounding skin (heating to about 42°C in the dermis). Vascular lesions can also be treated, but less selectively, with flash lamps (full visible light spectrum from about 530 nm). A Danish study has shown that both an IPL device and a long-pulsed dye laser are well suited for the treatment of telangiectasia in chronic radiation dermatitis after breast carcinoma radiotherapy [5].
Source: Aesthetic Dermatology & Laser Medicine, October 26, 2017, Zurich
Literature:
- Hibler BP, et al: Lentigo maligna melanoma with a history of cosmetic treatment: prevalence, surgical outcomes and considerations. Lasers Surg Med 2017; 49: 819-826.
- Vrcek I, et al: Infraorbital dark circles : A review of the pathogenesis, evaluation and treatment. J Cutan Aesthet Surg 2016; 9: 65-72.
- Passeron T, et al: Melasma treatment with pulsed-dye laser and triple combination cream: A prospective, randomized, single-blind, split-face study. Arch Dermatol 2011; 147: 1106-1108.
- Anderson RR, et al: Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science 1983; 220: 524-527.
- Nymann P, et al: Intense pulsed light vs. long-pulsed dye laser treatment of teleangiectasia after radiotherapy for breast cancer: a randomized split-lesion trial of two different treatments. Br J Dermatol 2009; 160: 1237-1241.
DERMATOLOGIE PRAXIS 2017; 27(6): 44-46











