Thanks to state-of-the-art diagnostic and therapeutic options, almost all children and adolescents who develop cancer can be cured today. However, the consequences of such hemato-oncological treatment should not be ignored. Cardiovascular complications are at the top of the list.
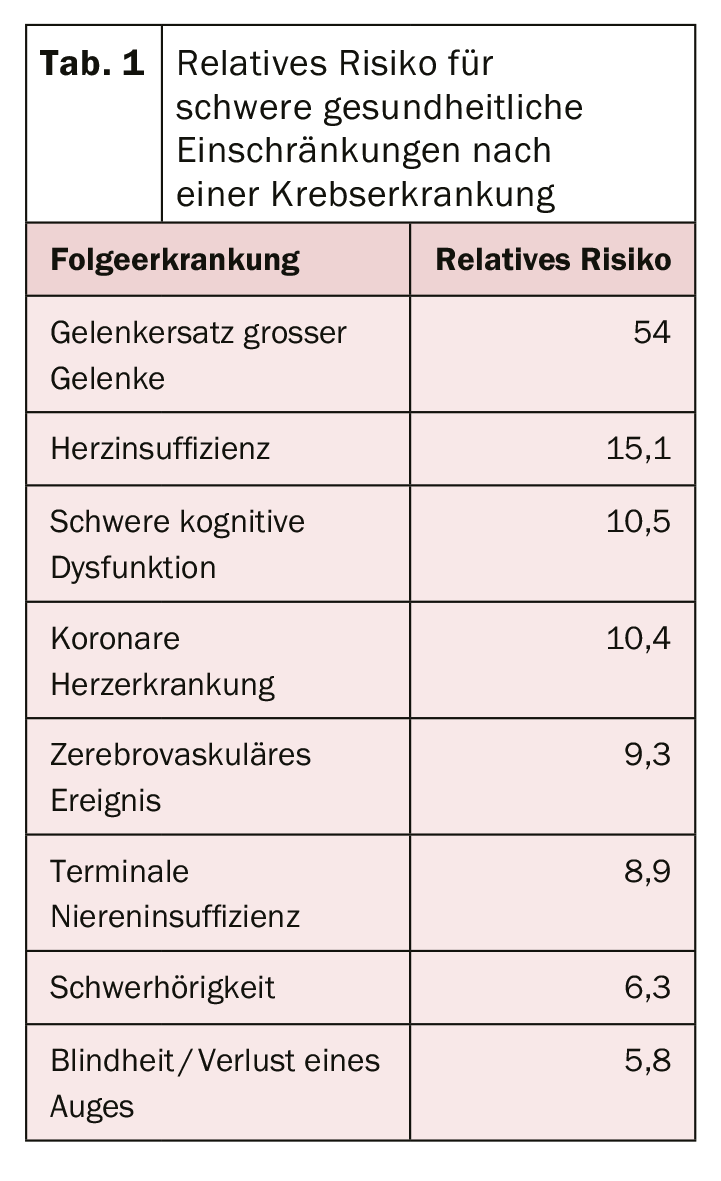
The survival rate of children and adolescents who develop cancer has been increased to over 80% in recent years. Nevertheless, their life expectancy is reduced because late effects resulting from cancer therapy cannot be ruled out. Up to 70% of all patients suffer from such health impairments 30 years after the end of treatment. These can affect different organs and potentially be life-threatening again, such as another cancer or severe heart failure. Common fatal outcomes after childhood cancer are secondary malignant neoplasms and cardiac problems.
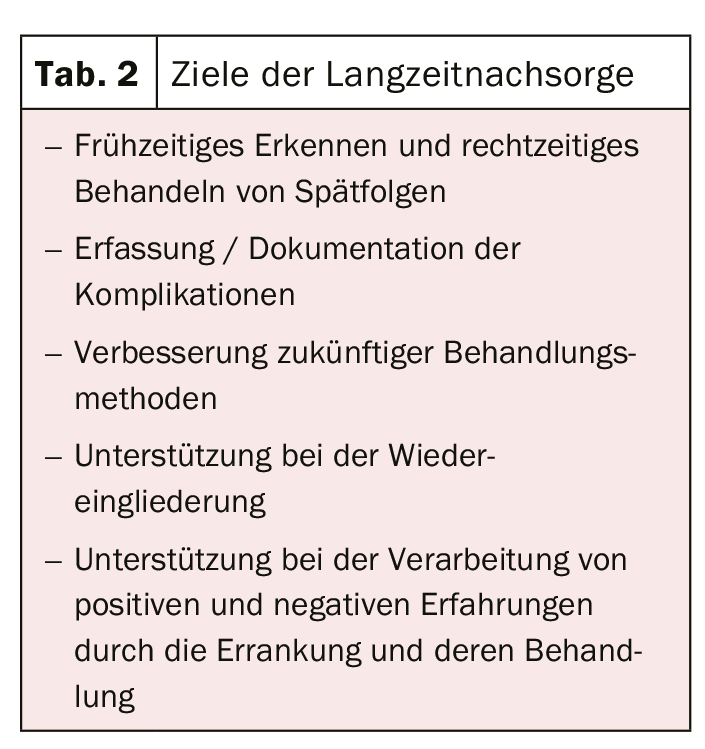
The risk of complications is influenced by individual factors such as previous diseases, age, gender and genetic predisposition. But of course the type of oncological therapy also plays a major role. Experts advocate an individualized follow-up plan, as many diseases can be treated well in the early stages. However, since the affected individuals then no longer fall under the purview of pediatric oncologists, an interdisciplinary approach is required.
The most common complications at a glance
The most common late effects can be found in the endocrine area. Endocrinopathies occur because radiotherapy can lead to dysfunction of endocrine organs. Thyroid disorders, hypothalamic-pituitary system disorders, or gonadal dysfunctions occur in more than one in two. The latter can be found mainly after chemotherapies. Radiation therapies are usually more likely to result in thyroid dysfunction or neoplasia.
The most serious and potentially life-threatening consequences include cardiac disease. Cardiomyopathies, valvular changes, arrhythmias or coronary heart disease can be treated well initially, but often the right time is missed and the disease progresses. The likelihood of cardiac complications increases, especially with anthracycline-containing chemotherapy and thoracic radiotherapy. A combination of both treatments, as used primarily in Hodgkin’s disease, further increases the risk. Overall, the relative risk of heart failure is increased by a factor of 15 for patients with childhood cancer. In addition, sufferers are also seven to eight times more likely to experience early cardiac-related mortality. According to the current guideline of the International Guideline Harmonization Group, a regular echocardiographic checkup should be performed because the risk of cardiomyopathies is significantly increased.
Further reading:
- www.awmf.org/uploads/tx_szleitlinien/025-003l_S1_Nachsorge_von_krebskranken_Kindern_Jugendlichen_06-2013-abgelaufen.pdf (last accessed on 2019-09-14)
- Kaatsch P, Spix C: German Childhood Cancer Registry – Annual Report 2017 (1980 – 2016).
- www.ighg.org/guidelines/topics/ (last accessed on 2019-09-15)
- Armenian SH et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. The Lancet Oncology 2015; 3:e123-e136
- www.kinderkrebsinfo.de/patienten/nachsorge/spaetfolgen___langzeitnachsorge/einfuehrung/index_ger.html (last accessed on 2019-09-14)
CARDIOVASC 2019; 18(5): 20