When asthma patients suffer from exacerbations, in at least two-thirds of cases they are triggered by either an allergy or an infection. In addition, however, there is also a not small number of cases that occur suddenly and for reasons that are incomprehensible to the physician.
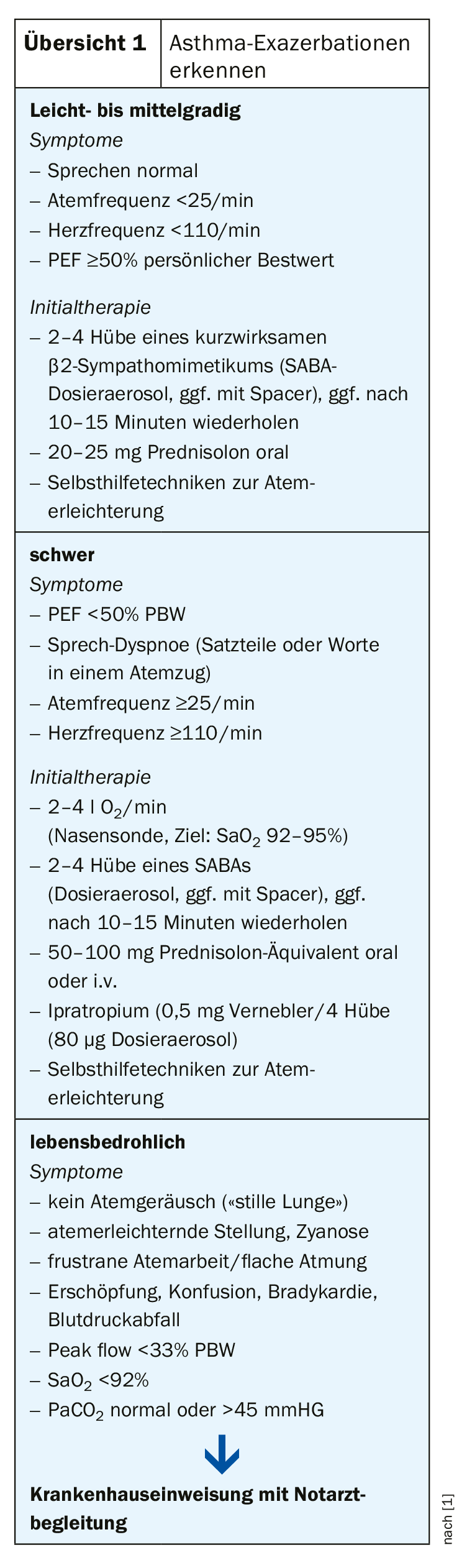
Asthma exacerbations always increase progressively, under a wide variety of conditions. The classic asthma symptoms such as chest tightness, wheezing and shortness of breath are typical. Condition deterioration necessitates an increase in treatment intensity. “And importantly, even patients with very mild asthma can get very severe exacerbations,” warned Professor Roland Buhl, M.D., head of the pneumology focus at the III Medical Clinic and Polyclinic of the University Medical Center Mainz, at the congress of the German Society of Internal Medicine (DGIM) in Wiesbaden, Germany.
Unholy Alliance Leads to Thunderstorm Asthma
As an example, the expert cited the phenomenon of a so-called “Thunderstorm Asthma” in November 2016 in Australia. Within a few hours, nine people had died in Melbourne and several thousand (!) had to visit the emergency departments there within five hours. In thunderstorm asthma, the season and a severe thunderstorm unholy ally with each other, Prof. Buhl said. Pollen from plants that have just bloomed freshly and that often trigger allergies there are torn out of the plants in the thunderstorm. In the air, they break up under the high humidity, becoming even more allergenic, and eventually come back down to the ground with the rain and moist air. People breathe it in, and in the case in Australia, this has led to very severe exacerbations in a very short time in a very large number of people.
Prof. Buhl reminded the audience of various risk factors that increase the risk of an exacerbation and to which physicians should pay attention during their consultations. For example, the warning bells should ring if patients need their emergency sprays frequently, i.e., have high SABA use, or if they are unwilling to use regular therapy with ICS, the drug that is critical for asthma. Patients with poor lung function or mental health problems and smokers are also predisposed to seizures. And again and again we can observe allergies that are not addressed, like the famous cat, which has an important social function and is not abolished despite allergy. Very important, according to Prof. Buhl: “Do blood work on your asthma patients once in a while, because eosinophils indicate risk populations.”
In prevention, it is important to communicate very clearly to the patient that regular use of inhaled cortisone during seizures is crucial. “And the best metered dose inhaler won’t help if it’s sprayed behind the ear, so please train your inhalation technique,” said the Mainz-based pulmonologist. The same is true for self-management, i.e., action plans and symptom monitoring. Individual risk factors should be identified and named in the consultation, as well as non-pharmacological interventions: Flu vaccination, smoking cessation, etc. If all these things are taken to heart, Prof. Buhl concludes, it is now possible to limit the frequency of at least higher-grade asthma exacerbations in patients to a very low level.
Source: DGIM 2019, Wiesbaden (D)
Literature:
- German Respiratory League, DGP & ÖGP. Pulmonology 2017; 71(12): 849-919
InFo PNEUMOLOGY & ALLERGOLOGY 2019; 1(2): 34 (published 9/26/19, ahead of print).