Diabetic foot syndrome is a common and serious complication of diabetes mellitus and contributes to impaired quality of life. Adequate multidisciplinary treatment can reduce these burdens. In addition to regular debridement and callus removal, infection control, protection from maceration, and exudate management using appropriate wound dressings are important treatment components.
Often, two or more risk factors are present simultaneously in diabetics. Diabetic peripheral neuropathy and peripheral arterial disease promote the development of foot ulcers [1]. Due to neuropathy, pain insensitivity and foot deformities may occur, often resulting in abnormal biomechanical loading of the foot. In affected individuals, even minor trauma (e.g., from acute mechanical or thermal overstimulation) can result in foot ulcers. Thickened skin (callus) forms, leading to a further increase in stress, often accompanied by subcutaneous bleeding and skin ulcers. Peripheral arterial disease (PAVD) is present in up to 50% of patients with a diabetic foot ulcer. PAOD is an important risk factor for wound healing disorders and lower extremity amputations.
Local therapy as part of a multifactorial approach
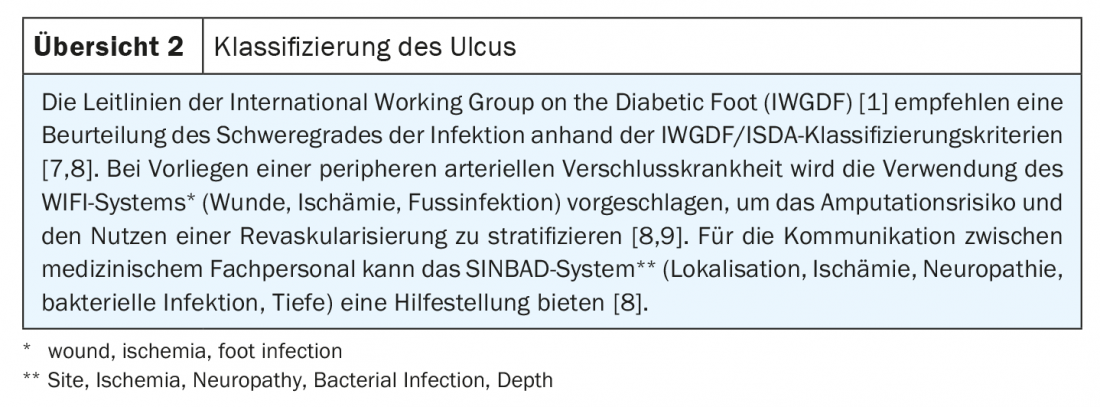
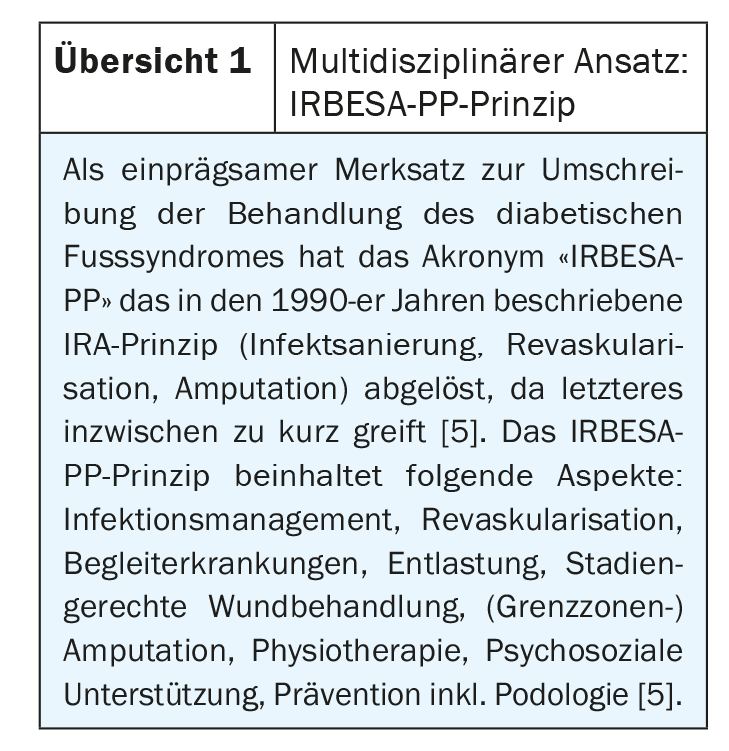
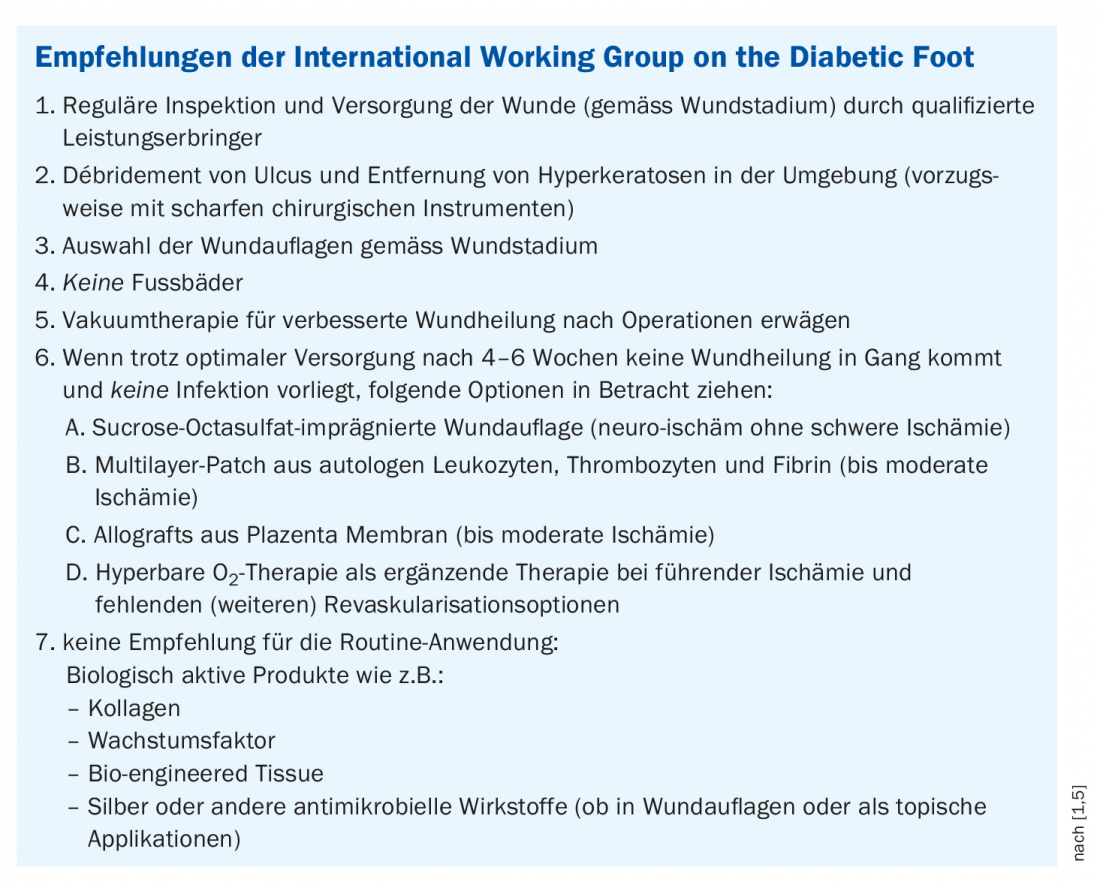
Local wound treatment makes an important contribution to the treatment of diabetic foot ulcers, but is only one of many factors in the overall concept of diabetic foot ulcer management (Overview 1). In the 2019 by the International Working Group on the Diabetic Foot (IWGDF) treatment guidelines, local ulcer management in diabetic foot is summarized as follows. (Box) [1]:
- Regular medical review of the ulcer is essential. The frequency depends on the severity of the ulcer and the underlying pathology, the presence of infection, the amount of exudation, and the intended wound treatment.
- Debridement of the ulcer, removal of the surrounding callus (preferably with sharp surgical instruments). Repeat this if necessary.
- Selection of dressings to control excess exudation.
- Do not soak feet (=no footbaths), as this may cause maceration of the skin.
- Consider low-pressure therapy procedures to aid in the healing of postoperative wounds.
Instead of “stage-adapted” or “phase-adapted” wound treatment, one could also speak of “environment-adapted” wound treatment, explained PD Dr. med. Gunnar Riepe from the Central Rhine Wound Center, Boppard (D), at this year’s virtual DGIM Congress [2]. First, he said, it is important to determine the location of the wound. If this is located in the forefoot, it is prognostically better compared to wounds of the hindfoot. Wound cleansing or debridement is a central treatment component in all cases. If the wound is infected, antibiotics, disinfection, dry dressing and immobilization are important further measures. If necrotization is suspected, the circulation should be controlled, and further steps include disinfection, pressure relief, and a dry dressing, as well as revascularization if necessary. Maceration is common in diabetic foot ulcers, and pressure on the wound promotes secretion of wound fluid. Besides pressure relief, coarse foam and superabsorbent are helpful. If there is a circulatory disorder, you should not use foil, as this promotes bacterial colonization. Superabsorbent foam is preferable for very moist, viscously exuding wounds. For pressure relief, “Total Contact Cast” is the more effective method than a heel cap or PU foam, summarizes Dr. Riepe.
Poorly healing non-infected ulcers: what to do?
Clinical studies have demonstrated the superiority of negative pressure wound therapy compared with standard therapy in terms of efficacy, wound healing, and amputation rate [3]. There was no increase in undesirable side effects. The use of negative pressure wound therapy is particularly advocated postoperatively in secondary wound healing for improved wound healing and wound base conditioning. If non-infected ulcers do not progress in wound healing after 4 to 6 weeks despite optimal clinical care, the International Working Group on the Diabetic Foot (IWGDF) guidelines suggest the following approach, each combined with patient education for foot ulcer care [1]:
- for neuroischemic ulcers without severe ischemia: a dressing impregnated with sucrose octasulfate
- in ulcers with or without moderate ischemia: treatment with an autologous leukocyte preparation
- for ischemic ulcers that do not heal despite revascularization: systemic hyperbaric oxygen therapy as an additional treatment
- for ulcers with or without moderate ischemia: placental membrane allografts
The highly publicized double-blind, two-arm randomized-controlled EXPLORER trial evaluated 240 patients with neuroischemic diabetic foot ulcers until complete healing [4]. Significant promotion of wound healing was demonstrated by the use of a wound dressing impregnated with sucrose octasulfate (NOSF). Considering the subject population restricted to neuro-ischemic cases without severe ischemia and without infection, there was a 48% healing rate within 20 weeks compared with 30% in the group with pads without NOSF. Biologically active products (collagen, growth factors, bioengineered tissue) and dressings or topical applications containing silver or another antimicrobial agent are not recommended for routine treatment of neuropathic ulcers.
Literature:
- IWGDF Guidelines on the prevention and management of diabetic foot disease 2019, German translation, https://ag-fuss-ddg.de (last accessed 05.05.2021).
- Riepe G: Wundmanagement, PD Dr. med. Gunnar Riepe, DGIM Annual Meeting, Interdisciplinary Clinical Symposium, 18.04.2021.
- Borys S, et al: Negative pressure wound therapy use in diabetic foot syndrome – from mechanisms of action to clinical practice. European Journal of Clinical Invest 2019; 49(4): e13067.
- Edmonds M, et al: Sucrose octasulfate dressing versus control dressing in patients with neuroischaemic diabetic foot ulcers (Explorer): an international, multicentre, double-blind, randomised, controlled trial. Lancet Diabetes Endocrinol 2018; 6(3): 186-196.
- Eckhard M: Diabetic foot ulcer needs interdisciplinary treatment. Diabetic foot syndrome – more than just a wound on the foot. In|Fo|Diabetology 2019; 13 (6).
- Vollmar J: Reconstructive surgery of the arteries, 4th edition, Thieme, Stuttgart, 1996; pp. 194-206.
- Armstrong DG, Peters EJ: Classification of wounds of the diabetic foot. Current diabetes reports 2001; 1(3): 233-238.
- González de la Torre H, et al: Clasificaciones de lesiones en pie diabético: Un problema no resuelto. Gerokomos 2012; 23(2): 75-87.
- Monteiro-Soares M, et al. Diabetic foot ulcer classifications: a critical review. Diabetes Metab Res Rev 2020; 36 Suppl 1:e3272.
FAMILY DOCTOR PRACTICE 2021