As part of an afternoon of continuing education for general practitioners, renowned representatives of the Dermatological Outpatient Clinic at the Stadtspital Triemli provided an insight into the history of the department. They also discussed current research desiderata and went into more detail about the many therapeutic options. The focus was especially on the practical reference to problems in family medicine.
At the beginning, Prof. Dr. med. Stephan Lautenschlager, Chief Physician of Dermatology, traced the hundred-year history of the Dermatological Outpatient Clinic. The skin as an important barrier and protection against chemical, physical as well as microbial influences was recognized early on as an organ in need of medical care: In 1913, Prof. Dr. Max Tièche, together with his wife Sabine, also a physician, opened the doors for the first time to the outpatient clinic at Hohlstrasse 82, which soon became the central contact point for many patients with skin and venereal diseases. “This institution thus represents one of the first hospitals in Zurich,” says Prof. Lautenschlager. Tièche was followed by Walter Burckhardt, also a dermatologist by vocation, who was responsible for numerous publications and legendary lectures that could sometimes last until late in the evening. In 1971 he was succeeded by Kaspar Schwarz, who ensured the stabilization of the Polyclinic. Alfred Eichmann was finally succeeded in 2002 by Stephan Lautenschlager, who is still in charge of the Dermatological Outpatient Clinic today. “Our motto was to continue to maintain the tried and true, yet be open to new challenges. In particular, maintaining the open consultation hours for all social classes, which Tièche was already conducting, is a concern for us. Anyone who has a problem with their skin can still come by. All they have to do is take a number and wait a little while. Furthermore, high-quality education, training and continuing education is also a constant focus of the department,” says Prof. Lautenschlager.
Non-melanocytic skin tumors
The second speaker was Med. pract. Daniel Fleisch, senior physician at the Dermatological Outpatient Center, on light skin cancer. Epidermal skin malignancies include the subtypes of so-called non-melanoma skin cancer (NMSC), specifically basal cell carcinoma (BCC), spinocellular carcinoma (SCC), and Bowen’s carcinoma. Carcinoma in situ includes actinic keratosis and Bowen’s disease. “NMSC is the most common cancer in Caucasians, more common than lung, breast, or prostate cancer combined. One can speak of an epidemic. In Australia, a highly sun-exposed country, about 9% of cancer costs are for NMSC, making it the most expensive cancer,” said Med. pract. Meat. “Part of the reason, of course, is that we expose ourselves to the sun more lightly clothed than we did a hundred years ago.” Around the age of 50, the prevalence increases rapidly, and men are particularly affected. The lifetime risk of developing BCC is 30%, and that for SCC is 10%. The incidence continues to rise (3-8%/year). “While mortality is low, the death rate for SCC is not quite one percent. However, there is a very high probability of second tumors: Nearly half of those with SCC will have another within three years. So follow-up examinations are urgently needed,” says Med. pract. Meat.
In addition to UV exposure (sunburns in childhood are particularly dangerous), nicotine consumption, immunosuppression, radiation and HPV also play a role in the development of this disease. “80% of NMSC are found in chronically light-exposed skin areas. It is not only people who work outdoors who are at risk. A recently published study [1], for example, was able to show that sun exposure during driving is comparable to that of outdoor activities or gardening,” explained Med. pract. Meat. The therapeutic options are very diverse, which can be illustrated by the example of actinic keratosis (Tab. 1).

Top five skin infections
Siegfried Borelli, M.D., Senior Physician at the Dermatological Outpatient Center, presented the top five skin infections based on referral reasons and telephone inquiries: Recurrent boils, tinea, herpes zoster, verrucae vulgares, scabies.
Furuncles are painful nodules involving the entire hair follicle and melting into pus in a central abscess-like manner, possibly forming a conglomerate (carbuncle). They can be taken as indicative of immunodeficiency whenever they begin in childhood, there is a positive family history, specific patterns of organ involvement and unusual pathogens are present, or histology shows granuloma formation or absent neutrophils. “Predisposing factors for boils should be clarified by means of anamnesis (nicotine abuse, diabetes), laboratory or focus search of contact persons from the immediate environment. Therapy proceeds via incision or excision of fluctuating abscesses, antibiosis, decolonization and, not to be forgotten, environmental decontamination,” says Dr. Borelli.
Mycoses, specifically tinea corporis, are manifested by marginal erythema, flaking of the same, central draining, and centrifugal spread. The lifetime risk of developing the disease is just over 70%, with men three times more likely to be affected than women. Particularly insidious is tinea incognita, a fungal infection whose clinical appearance has been altered by the application of topical steroids, resulting in sometimes bizarre erythema. “Risk factors for tinea pedis are mainly familial disposition, foot deformities, male gender and diabetes mellitus, but the use of public baths can also cause this clinical picture,” Dr. Borelli emphasized.
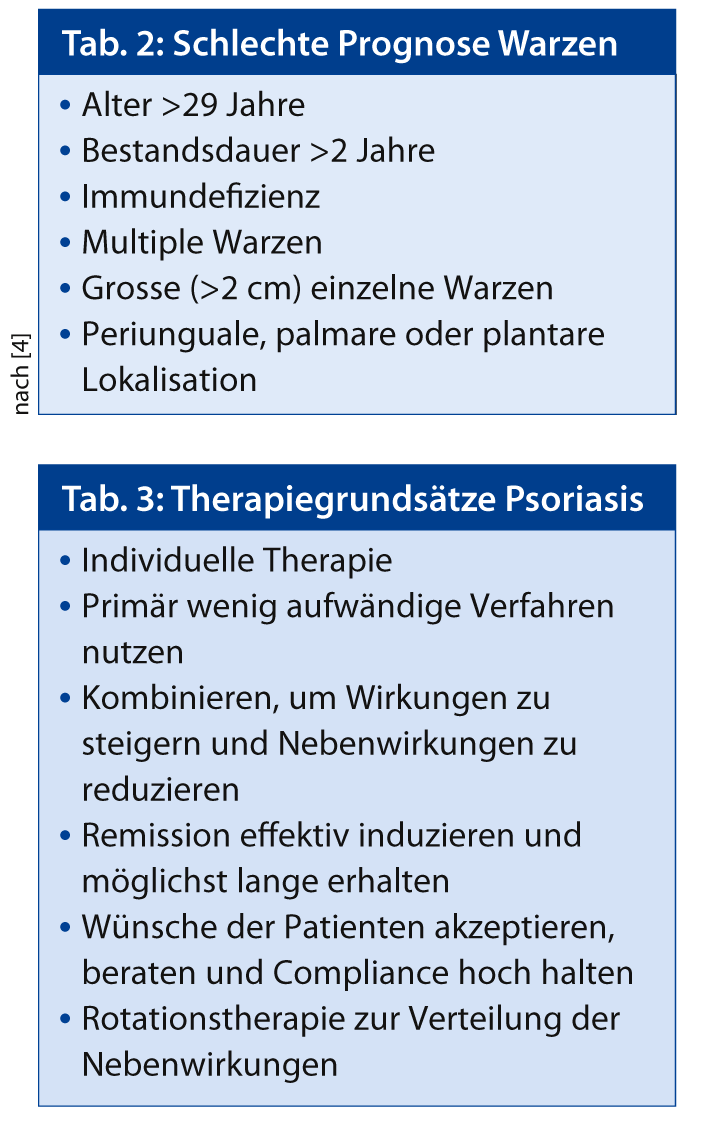
Regarding viral infections, verrucae vulgaris were discussed in more detail. Warts represent a common reason for referral. They have a high prevalence, especially in the first three decades of life, and are also refractory to treatment because there is no efficient antiviral therapy. In particular, the patient should be made aware of prognostically unfavorable factors (Tab. 2). “In the case of herpes zoster, viral detection can confirm the diagnosis and provide a decision-making aid for systemic therapy,” said Dr. Borelli.
Scabies does not only occur in poor and war-torn areas. In addition to a large number of sporadic cases, there were also two smaller epidemics in the Zurich area in 2001 and 2006, specifically in a nursing and residential home. The therapy is carried out with permethrin 5% (1×, possibly repeat after 14 days). In any case, disinfection measures must be taken to accompany the therapy and the persons in the close environment must be included in the treatment.
News on psoriasis vulgaris
Prof. Lautenschlager closed the series of lectures with a contribution on psoriasis. This disease is defined by chronic, sharply demarcated erythrosquamous plaques that occur primarily on the joint extensor surfaces and scalp. However, there is extraordinary variability in disease progression, extension, and morphology. “Psoriasis is a disease of the Western world: in Europe, the prevalence is 2-3% of the population. As this disease is chronic and lifelong, it imposes an immense emotional and physical burden, similar to that of diabetes,” says Prof. Lautenschlager. There is a wide range of comorbidities. Some associations, e.g. with obesity or metabolic syndrome, have been noted in recent studies [2, 3].
“In therapy, Imiquimod should not be used under any circumstances, this can lead to sometimes grotesque inflammation in psoriasis within a few days. Topical therapy with corticosteroids, vitamin D analogues, tar or dithranol is useful for treating mild psoriasis (about 75% of all patients). In the remaining 25% with moderate to severe expression, light therapy (UVB/PUVA) with up to 30 sessions or systemic therapy with retinoids, methotrexate, fumaric acid, cyclosporin A, hydroxyurea, biologics (such as adalimumab, etanercept, infliximab, ustekinumab) should be considered. In any case, some therapeutic principles (Tab. 3) must be observed in practice,” Prof. Lautenschlager explained in conclusion.
Source: Stadtspital Triemli: 100 years of dermatology & venereology for the population of the city of Zurich (1913-2013), August 29, 2013, Zurich.
Literature:
- Kim DP, et al: Sunscreen use while driving. J Am Acad Dermatol 2013 Jun; 68(6): 952-6. doi: 10.1016/j.jaad.2012.12.964. epub 2013 Feb 4.
- Armstrong AW, et al: The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutrition and Diabetes 2012; 2: e54. doi:10.1038/nutd.2012.26. Published online December 2012.
- Armstrong AW, et al: Psoriasis and metabolic syndrome: a systematic review and meta-analysis of observational studies. J Am Acad Dermatol. 2013 Apr; 68(4): 654-62. doi: 10.1016/j.jaad.2012.08.015. epub 2013 Jan 27.
- Rübben A: Clinical algorithm for the therapy of cutaneous extragenital HPV-induced warts. Dermatologist 2011; 62: 6-16.