If asthma patients use an inhaled corticosteroid (ICS) over a longer period of time and in high doses, even the additional combination with a long-acting β2-agonist (LABA) does not respond as desired, and they are still insufficiently controlled even with the additive use of a short-acting β2-agonist (SABA), then we are therapeutically approaching the end of that stepwise scheme that the GINA guideline for the treatment of bronchial asthma prescribes. Antibody therapy can then be considered as a next step. But which biologic is right for which patient?
The use of biologics should ideally be considered before the patient is permanently treated with systemic cortisone, advised Dr. Stephanie Korn of the Thorax Clinic in Heidelberg (Germany) and Medical Director of the Asthma Outpatient Clinic there [1]. Several antibodies are available today and have been used for some time. To determine which agent is most appropriate for which patient, she incorporates patient characteristics, biomarkers and comorbidities into decision-making.
Biomarker
If IgE as an allergy antibody is responsible for severe asthma, the use of the IgE antibody omalizumab may reduce the number of free IgE, resulting in improvement of asthma. In patients in whom the cytokines interleukin(IL)-4 and -13 play a role, the anti-IL-4 receptor antagonist dupilumab (anti-IL-4Rα) can be used to achieve success, as it blocks pathways mediated by IL-4/13. Patients who have very high numbers of eosinophils in the peripheral blood can be treated effectively with an antibody against interleukin-5 (mepolizumab, reslizumab) , since IL-5 recruits the eosinophils. In addition, Benralizumab is available here, which docks to the IL-5 receptor (anti-IL-5Rα), with the result that the eosinophils are completely destroyed and the patients no longer exhibit them at all.
Eosinophils, IgE and FeNO are the three biomarkers that are usually co-determined in all patients. This does not mean that a patient should be treated only according to biomarkers, the expert cautioned: “With a high IgE, he does not automatically get anti-IgE – but the biomarker fits into the overall picture as one piece of the puzzle.” The biomarkers are therefore helpful as a starting point for diagnostics: If a patient has an FeNO above 25 and eosinophils above 150, these are the best prerequisites for a response to dupilumab, Dr. Korn cited as an example. However, this does not mean that patients with other biomarker levels will not respond.
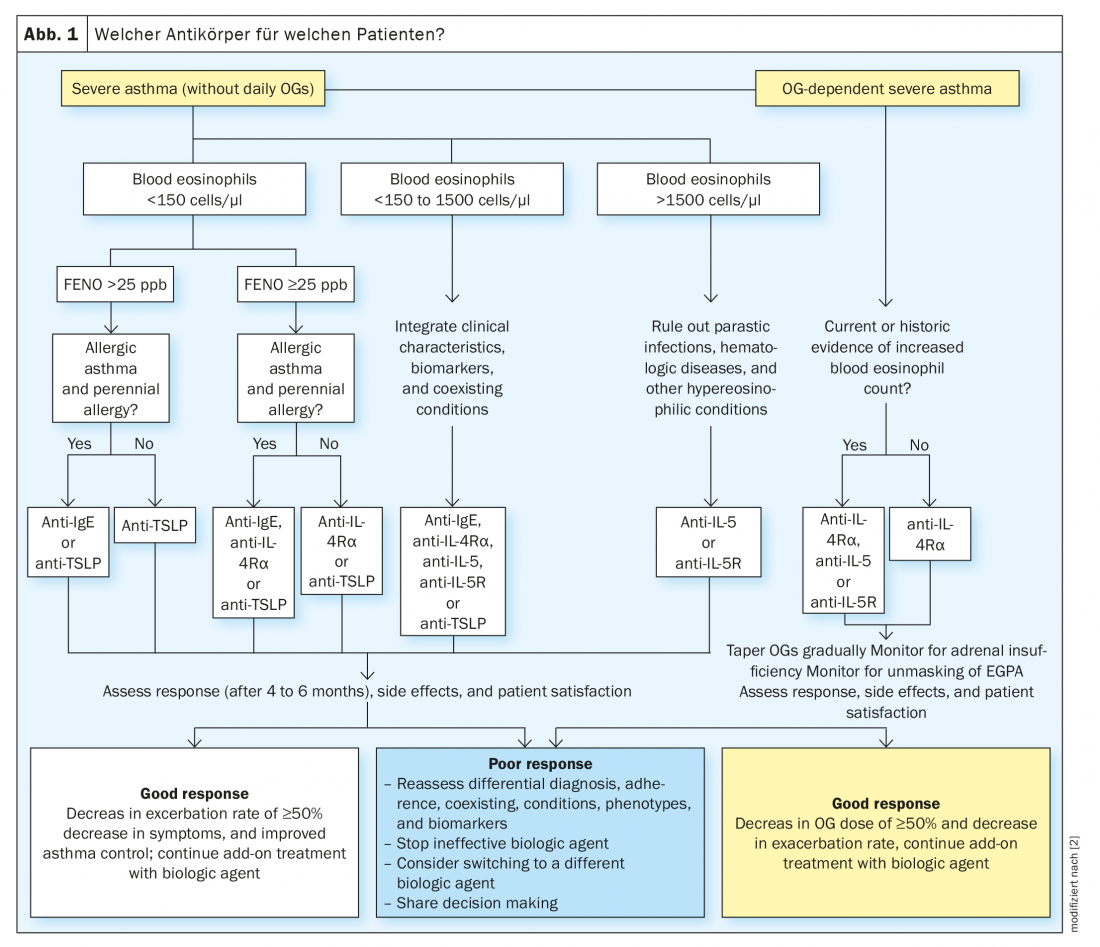
To determine which biologic to use in his or her patient, Dr. Korn referred to an algorithm developed by Brusselle and Koppelman [2] (Fig.1). “That’s an idea of how to proceed to end up with an antibody that you certainly can’t go wrong with.” However, it also follows from the algorithm that there are usually still two or even three options left. So at the end of the day, there is still a residual decision left with the treating physician. To facilitate this decision, Dr. Korn referred to the individual patient characteristics that should never be disregarded.
Patient characteristics
“A patient who states that he has suffered from asthma since the age of 50, which was immediately relatively severe, who is constantly taking cortisone tablets, and who also states that he cannot smell, is typical of severe eosinophilic asthma. Such a patient is predisposed to anti-IL-5 treatment.” In contrast, another patient who says he had on-and-off allergies and mild asthma symptoms in childhood, which at times disappeared altogether, but over the years slowly got worse and worse, is typical of severe allergic asthma and accordingly a candidate for anti-IgE therapy. “So talking to the patient should give us an initial indication of the direction we’re going with them.”
Course and comorbidities
Further factors are the biomarkers in the course as well as the comorbidities: During therapy with dupilumab, eosinophil counts increase at baseline. “In most patients, it has no consequence clinically at all,” Dr. Korn reassured. However, if a patient has over 1500 eosinophils, for example, she would be cautious about treating that patient with dupilumab, as an increase of up to 40% may well occur. Therefore, in patients with very high eosinophils, the expert would still prefer anti-IL-5.
Since an asthma patient often has other conditions as well, a look at the other approvals of the biologics can be very helpful. “If a young person comes to you with asthma who also has atopic dermatitis, the obvious thing to do is to treat him with dupilumab, because this is also approved for atopic dermatitis.” So the principle of killing two birds with one stone could well work here. If the patient ultimately responds successfully to neuroderminis but continues to suffer from his asthma, it may be considered to maintain dupilumab for AD and additionally use another antibody to treat the asthma. “In such cases, however, the situation has always been that we ended up with two antibodies for two different indications – I have not yet used two antibodies in parallel just for severe asthma,” Dr. Korn urged caution in such considerations.
Anti-TSLP
Very rare, but occasionally occurring, are patients who have no biomarkers at all, i.e., who do not have high IgE or FeNO and whose eosinophil counts are low. One reason may be that they are taking cortisone. Occasionally, however, there are patients who do not have these values from the outset, and in whom it is then correspondingly difficult to use the antibodies in accordance with the approvals.
In the future, a new antibody could provide a remedy here: TSLP is an epithelial cytokine whose antibody (tezepelumab) can be used to go into both the allergic and eosinophil pathways and into structural cells. “The question ultimately is, does this work more broadly and can I possibly use it in a less differentiated way or in patients where the biomarkers are not as high?”
It is possible, then, that future therapy will move in the direction of treating patients who have several of the pathways with an antibody such as anti-TSLP that targets much higher up and thus blocks those pathways completely, rather than using a biologic that takes away only one pathway, according to Dr. Korn’s outlook.
62nd Congress of the German Society for Pneumology and Respiratory Medicine e.V. in Leipzig (D), May 25-28, 2022.
Literature:
- Korn S: Severe asthma and biologic therapy – the agony of choice? Symposium “State of the Art Asthma” in the context of the DGP Congress, 26.05.2022.
- Brusselle GG, Koppelman GH: Biologic Therapies for Severe Asthma. N Engl J Med 2022; 386: 157-171; doi: 10.1056/NEJMra2032506.
InFo PNEUMOLOGY & ALLERGOLOGY 2022; 4(3): 22-24.











