The diagnosis of Meniere’s disease is based on history, audiometry, and instrumental vestibular function tests. Treatment should be provided by an experienced ENT specialist. A variety of therapeutic options exist, and a distinction is made between destructive and non-destructive treatments. The treatment is individual, it should be based on a graduated scheme. The most important and difficult differential diagnosis is vestibular migraine.
Meniere’s disease is named after the French physician Prosper Meniere, who first described the classic symptoms: immobilizing attacks of vertigo lasting several hours, fluctuating slowly progressive hearing loss, tinnitus and ear pressure. The only certainty is that there is increased pressure in the fluid-filled inner ear (endolymphatic hydrops). Whether this is due to excessive fluid production, insufficient resorption, or impaired endolymphatic flow (stenosis of the endolymphatic duct) remains unclear.
Various etiologies are discussed such as gap junction disorders leading to a dysbalance of inner ear homeostasis by altering ion concentrations and thus leading to hydrops, or dysregulation of the arginine-vasopressin-aquaproin-2 system in which excessive aqueous influx is thought to cause hydrops.
Definition of Meniere’s disease
The diagnosis of M. Meniere’s disease is made clinically. This is based on the guidelines of the American Academy of Otolaryngology and Head and Neck Surgery (AAO-HNS) [1]. These are shown in Table 1.

By definition, the spinning attacks last at least 20 minutes, typically several hours. Usually the dizziness is accompanied by nausea and vomiting, and patients are usually immobile and unable to walk during the attack. Afterwards, they are often very exhausted and there is still a rather diffuse uncertainty for a few hours. Torsional vertigo is always accompanied by nystagmus, which typically beats horizontally, with a mild rotatory component. From the direction of the nystagmus, the affected side cannot be determined with certainty, since initially there is often not a dropout nystagmus to the healthy ear (fast component), but a so-called stimulus nystagmus to the diseased ear may be present.
The hearing loss in Meniere’s disease is always sensorineural (inner ear) and usually occurs together with the vertigo attacks. Typically, there is a threshold elevation in the low frequency range during the first seizures, which initially recovers after the seizure. With increased seizures, this recovery is incomplete and a relapsing progressive hearing loss develops, which in the course also affects the high frequencies. In some cases, there is fluctuating hearing in the early stages, even in the seizure-free interval. Accompanying noise tinnitus and ear pressure often exist, and some patients report a feeling of fullness or absorbent cotton in the ear.
In only 20% does the disease begin with the typical triad of rotary vertigo attacks, hearing loss and noise tinnitus. At the beginning, only dizziness or vertigo occur in 40% of the cases. Ear symptoms. Therefore, it often takes several years from the first symptoms until the diagnosis is made.
It is characteristic of Meniere’s disease that its course is completely unpredictable. The severity of the hearing loss as well as the frequency and strength of the vertigo attacks can vary greatly from person to person.
In cases of recurrent vertigo attacks with or without accompanying ear symptoms, a neuro-otological examination by an ENT specialist is indicated.
Diagnostics
Primary diagnostics include sound audiometry in addition to the seminal history and clinical examination. In addition, various instrumental tests are available for vestibular function testing.
Clinical vestibular testing focuses on examination with Frenzel glasses to detect nystagmus. A peripheral vestibular nystagmus beats in the same direction for all gaze directions, increasing in intensity when looking in the direction of the fast phase and decreasing in intensity when looking in the opposite direction (Alexander’s law). Visual fixation can suppress or at least slow down the nystagmus. Nystagmus is detectable during or shortly after a vertigo attack in Meniere’s disease, but not during the seizure-free interval. In addition to otoscopy, the Weber tuning fork test should be performed. Normally, the tuning fork sound is lateralized to the healthy ear, but in certain cases it is lateralized to the diseased side. The audiogram typically shows a low-frequency sensorineural hearing loss (hydrops curve, low-frequency tub). Because hearing often fluctuates, there may be no detectable hearing loss at the time of the examination. In these cases, the patient should be urged to report promptly when hearing decreases so that the test can be repeated during the poor phase.
Calorics is the main focus of the apparative clarifications. Here, the vestibular organs are stimulated separately with 44°C warm and 30°C cold water for 30 seconds. In the early stages of the disease, excitability is often still symmetrical. In the course of the disease, however, hyperexcitability in the sense of peripheral vestibular dysfunction develops on the affected side. A fine-slice MRI of the inner ear/brainstem is usually obtained to rule out retrocochlear dysfunction (especially vestibular schwannoma). Recently, it has become possible to detect endolymphatic hydrops with special MRI sequences [2].
Therapy
Treatment of M. Meniere’s disease usually follows a stepwise scheme (Fig. 1), but it must always be individually adapted. Since several treatment options are often possible, the advantages and disadvantages of each treatment must be discussed in detail with the patient.
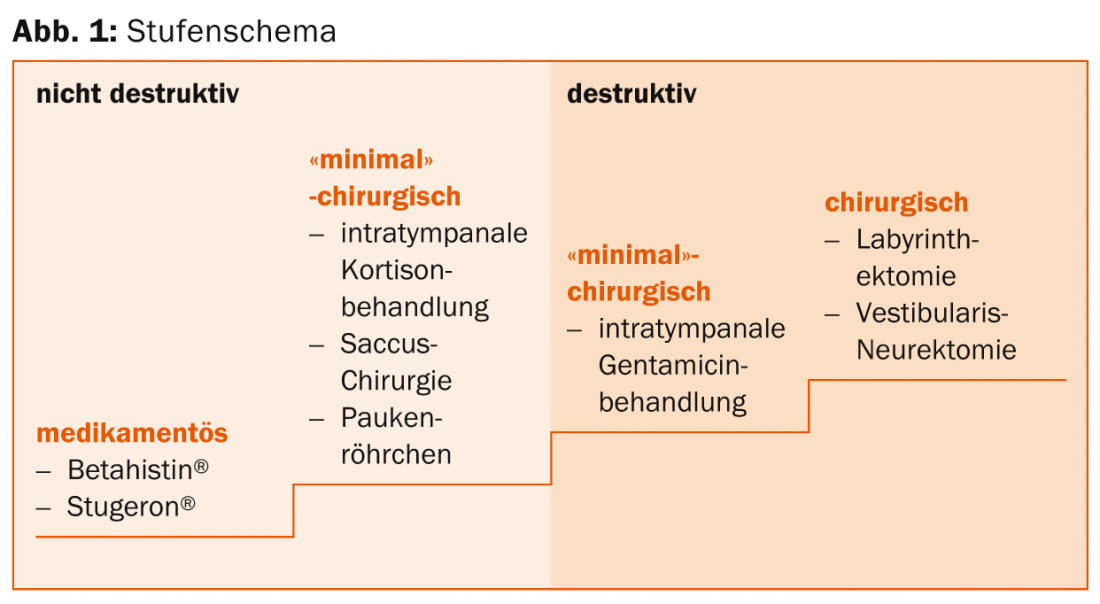
Common therapies can be divided into two main groups: low-risk non-destructive and higher-risk destructive. In the second group, targeted chemical or surgical damage is placed on the organ of equilibrium. Therefore, following these therapies, patients suffer from more or less pronounced dizziness and gait instability. The group of destructive therapies includes intratympanic gentamicin treatment as well as labyrinthectomy and vestibular neurectomy. These treatments carry the risk of hearing loss and even deafness. Low-risk nondestructive therapies are divided into drug and minimally surgical. In addition to oral medications, these include intratympanic steroid treatment, tympanostomy tube insertion, and saccus surgery.
Usually, primary therapy for suspected M. Meniere’s disease is betahistine 2× 24 mg/d for six to eight weeks. Betahistine acts as a partial histamine H1 receptor agonist and a histamine H3 receptor antagonist. Pharmacological tests in animals have shown that blood circulation in the stria vascularis of the inner ear improves, probably by relaxing the precapillary sphincters of the microcirculation of the inner ear. With a good response, therapy should be given for at least six months. If attacks recur after a discontinuation attempt, continuous treatment may be necessary. If therapy is unsuccessful, group 4 calcium antagonists or intratympanic steroid treatment may be considered as alternatives. Most commonly, cinnarizine (Stugeron®) is used 3× 25 mg/d. In patients with known migraine, flunarizine (Sibelium®) 10 mg/d in the evening is a good alternative, as it can have a positive effect on both Meniere’s disease and migraine. Intratympanic steroid treatment involves the application of a cortisone-containing fluid (usually dexamethasone) under surface anesthesia through the tympanic membrane directly into the middle ear. In up to 75% of cases, this therapy leads to significant improvement, and 50% of patients are seizure-free in the long term. A good third of patients experience a significant improvement in hearing during treatment [3]. Why the tympanostomy tube insertion in Meniere’s disease has a positive effect on vertigo attacks is not clear. The success rate, as with most non-destructive therapies, is approximately 67%.
Destructive therapies are usually used only when the treatments listed above do not help sufficiently and the diseased side is known. In patients suffering from migraine, one must be sure that the vertigo attacks are caused by Meniere’s disease. Gentamicin is an aminoglycoside antibiotic with vestibulotoxic effects. When applied intratympanally, it causes a deterioration of vestibular function, which is manifested in diffuse fluctuating vertigo or dizziness. of an unsteady gait. The risk of therapy-related hearing loss is approximately 20% [4]. During vestibular neurectomy, the vestibular nerve is cut, disconnecting the vestibular organ from the brain. In labyrinthectomy, the organ of balance is surgically removed, leaving the cochlea in place. Since this procedure results in deafness, it is performed only in cases of highly impaired hearing. Neurectomy is performed with good resp. only slightly impaired hearing to the application. The risk of postoperative hearing loss is less than 10%. Both operations cause a complete loss of function of the corresponding organ of equilibrium. Initially, there is severe vertigo as in neuronitis vestibularis. As part of central compensation, the balance returns to normal within two to three months. In most cases, it is useful to perform balance training under physiotherapeutic guidance. However, certain limitations of balance in everyday life may persist, especially during rapid movements and in the dark.
Differential diagnosis
Rarely, a retrocochlear disorder (vestibular schwannoma) can mimic Meniere’s disease, so an MRI scan is useful. Benign paroxysmal positional vertigo can be easily distinguished from Meniere’s disease by history, since the vertigo attacks last only a few seconds and no ear symptoms are present. In acute cochleo-vestibular dysfunction, the spinning vertigo lasts for several days and the hearing loss is usually pancochlear and not low-pitched.
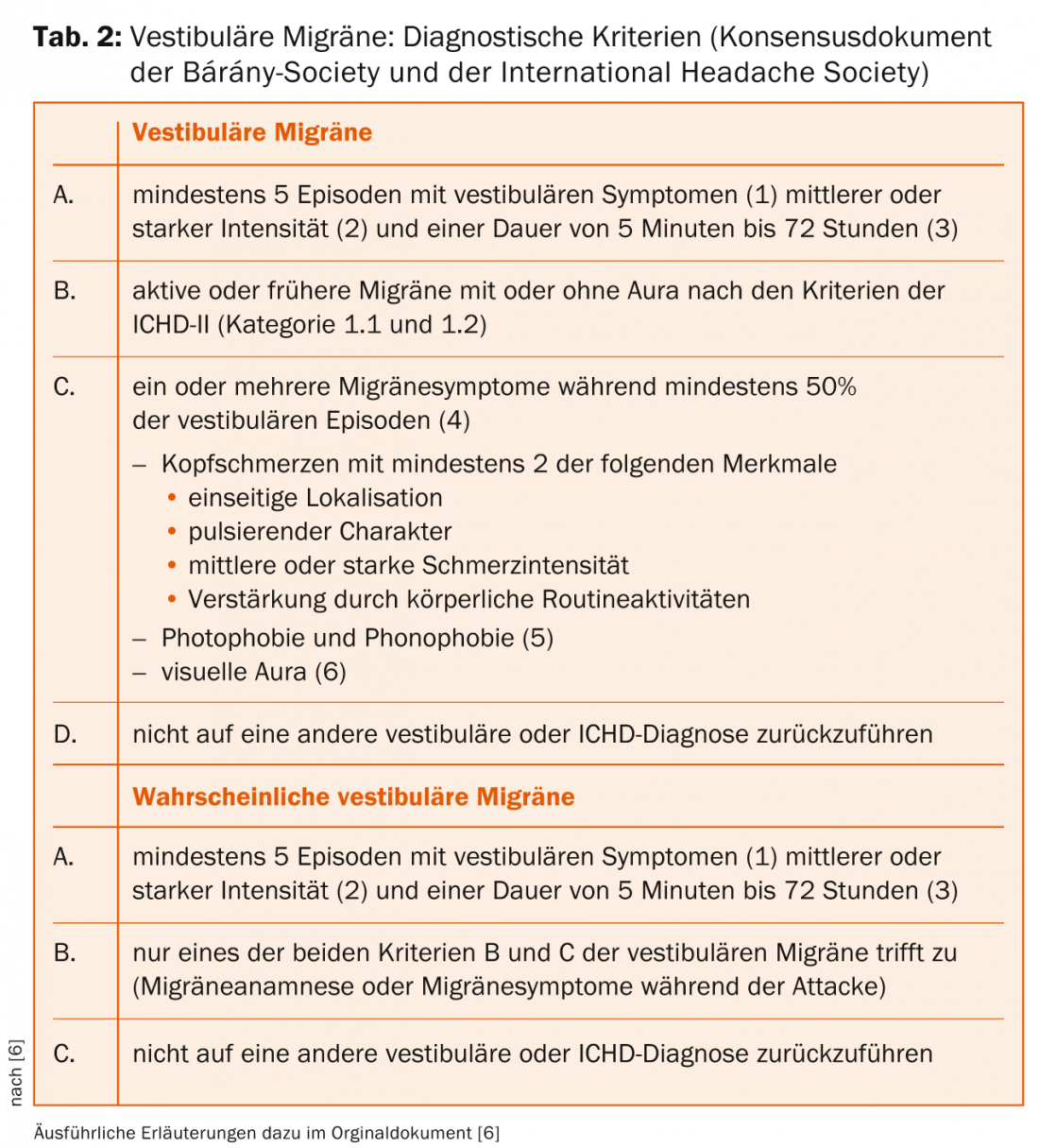
Vestibular migraine is the most important differential diagnosis to M. Meniere’s disease in patients with rotary vertigo attacks lasting for hours. For several years, vestibular migraine has been described as a special form of migraine [5], which typically presents with attacks of spontaneous or positional vertigo for seconds to days and migraine symptoms. Ear symptoms are rare, but may also occur. The International Headache Society (IHS) and the Bárány Society, an international society for the study of vestibular disorders, developed a consensus document with uniform diagnostic criteria for vestibular migraine and published it in 2012/2013 (Table 2) [6].
The probability of migraine in women is 12-15%, in men 6-8%. According to various authors, however, significantly more (25-40%) Meniere’s patients suffer from migraine at the same time. It is not clear why the two diseases occur together in clusters. Because Meniere’s disease often presents with inconspicuous findings in the early stages (especially in the interval), it is not possible to make a definitive diagnosis in some cases. In such cases, addressing resp. Failure to respond to appropriate Ménière’s resp. Migraine treatment helpful. In some patients, it may be necessary to treat both conditions, for example, betahistine combined with high-dose magnesium.
Literature:
- Committee on Hearing and Equilibrium Guidelines for the diagnosis and evaluation of therapy in Meniere’s disease. Otolarnygol Head Neck Surg 1995; 113: 181-185.
- Baráth K, et al: Am J Neuroradiol 2014; 35: 1387-1392.
- Garduño-Anaya MA, et al: Otolaryngol Head Neck Surg 2005; 133: 285-294.
- Lange G, Mann W, Maurer J: ENT 2003; 51: 898-902.
- Dieterich M, Brandt T: J Neurol 1999; 246(10): 883-892.
- Lempert T, et al: Neurologist 2013; 84: 511-516.











