Cervical syndrome causes tension and hardening in the muscles, which can result in pain and impaired function. In addition to headaches, dizziness, and other mood disorders, swallowing difficulties may also occur. Often, the primary care physician is the first point of contact. Differential diagnosis requires imaging studies of the cervical spine. Treatment of functional dysphagia is primarily conservative.
In the series “Dysphagia”, various organic changes in the upper part of the digestive tract have already been described as causes of dysphagia. The current article deals with a dysfunction of the swallowing act, which can be regarded as functional, triggered by a dysstatism of the cervical spine with consecutive muscular imbalance and tension reactions. There are no isolated pathognomonic signs of vertebragen provoked disorder in the head and neck region [2]. The symptoms (overview 1) are manifold and require close interdisciplinary cooperation of several specialties for clarification and differential therapy.
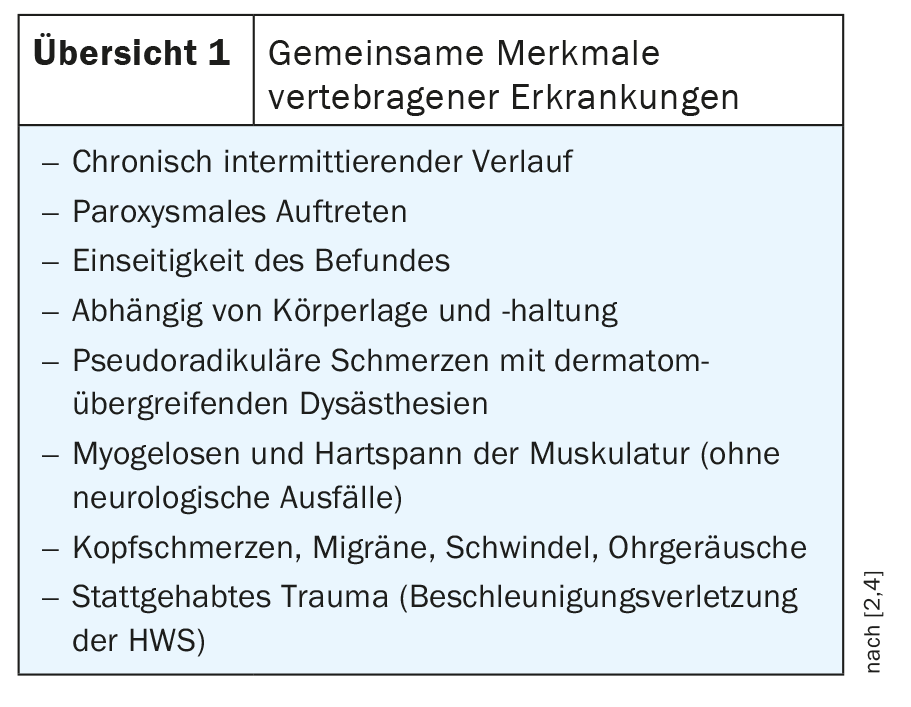
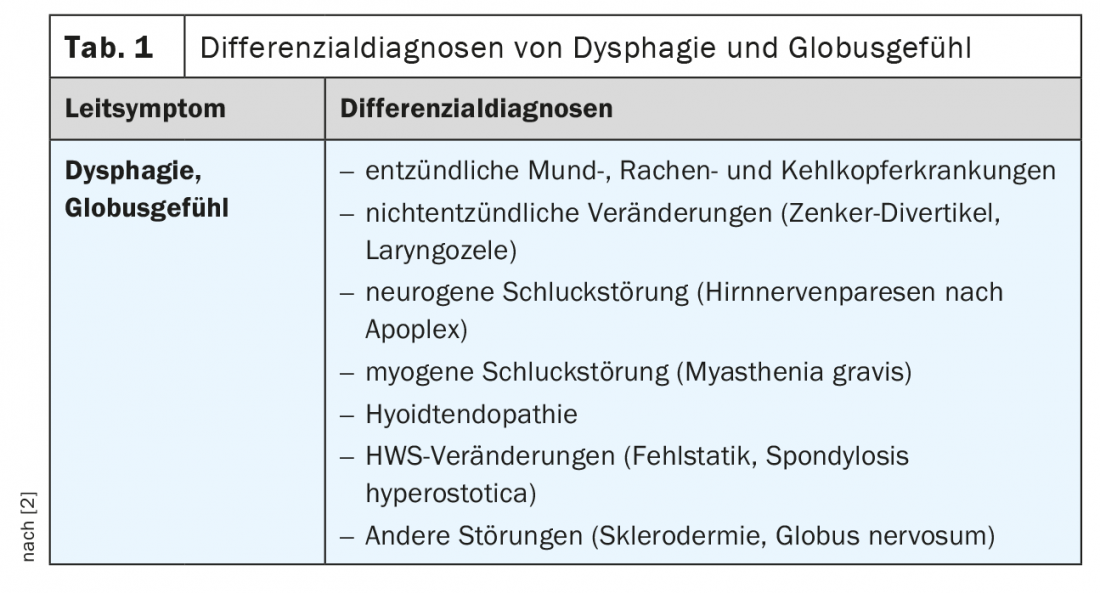
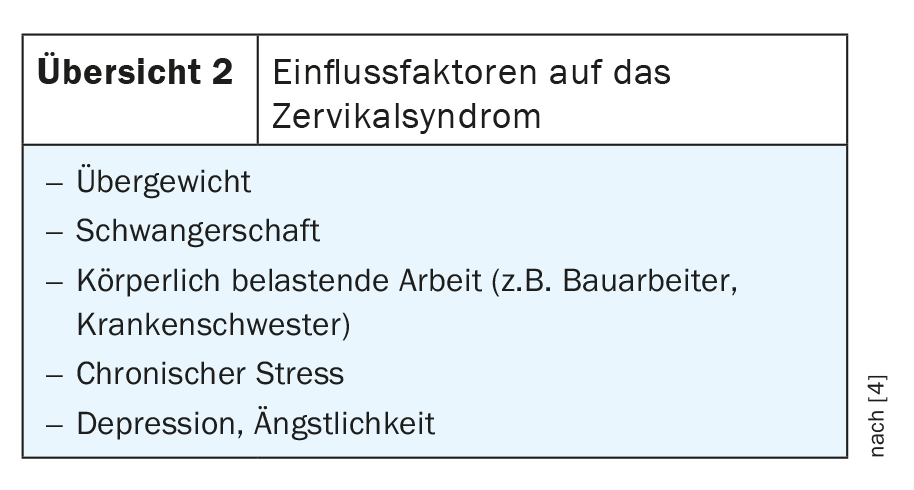
Dysphagia and dysphonia may be causally related to organic diseases. Several differential diagnoses must be clarified (Table 1) . The disorder of the musculoskeletal system in the cervical region is subject to several influencing factors (overview 2).
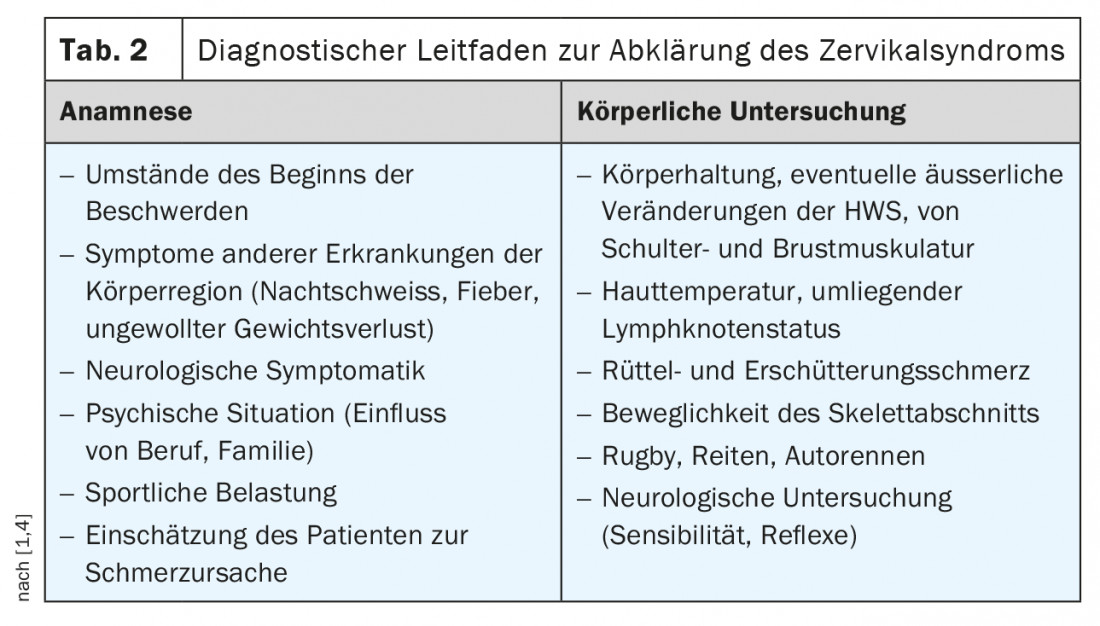
Often, the primary care physician is the primary point of contact for affected patients. The exact anamnesis and the physical as well as orienting neurological examination set the course for supplementary diagnostic measures, in particular imaging measures, and the resulting therapy. Misstatics with consecutive problems is not only a consequence of overload or trauma, it is also part of the changes in various syndromes [3].
A diagnostic guide can be found in Table 2 for guidance.
In addition to analgesic drug therapy measures and acupuncture, physical-physiotherapeutic treatments are used. In the long term, exercise and sports (walking, swimming, back exercises and yoga) can help improve.
X-ray examinations of the cervical spine in 2 planes, supplemented if necessary by functional images to document restricted or even segmental hypermobility, can document degenerative changes and faulty statics. Occasionally, an impression of the esophageal posterior wall is also apparent on lateral images in esophageal wide swallow and hypertrophic spondylosis deformans, which can lead to dysphagia spondylotica. The stretching or kyphotic bad posture alone can trigger myogelosis with a feeling of pressure and a feeling of lumpiness.
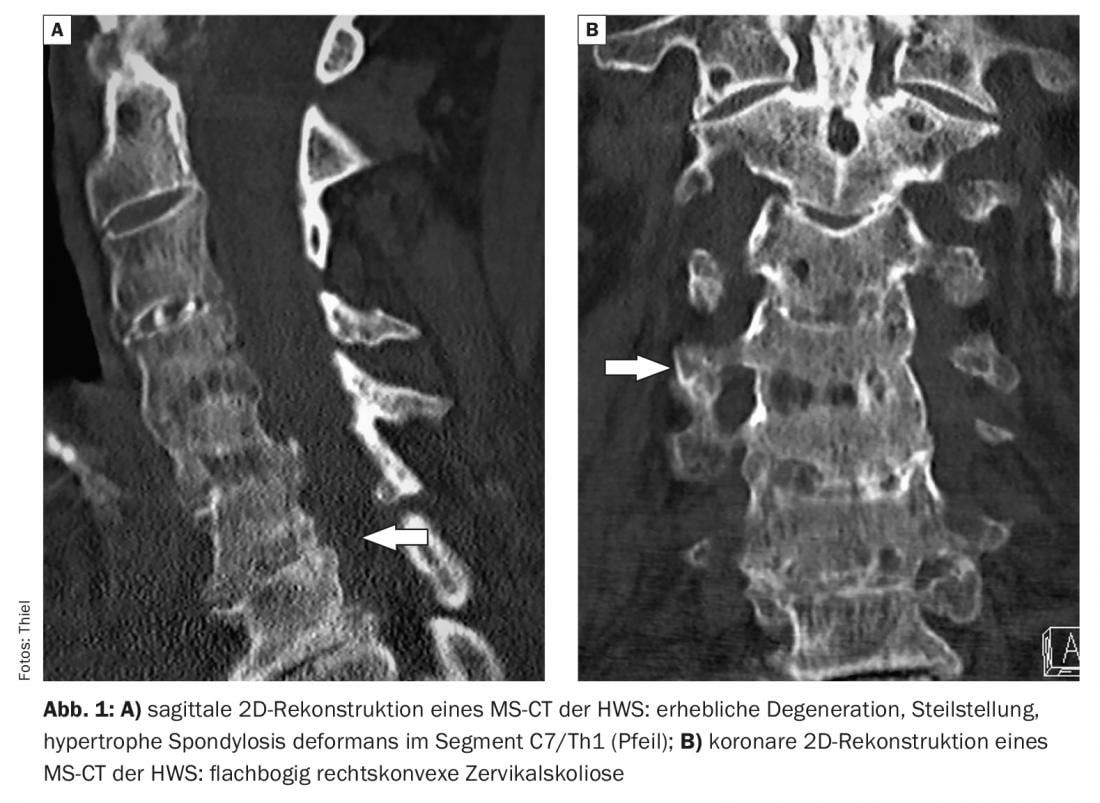
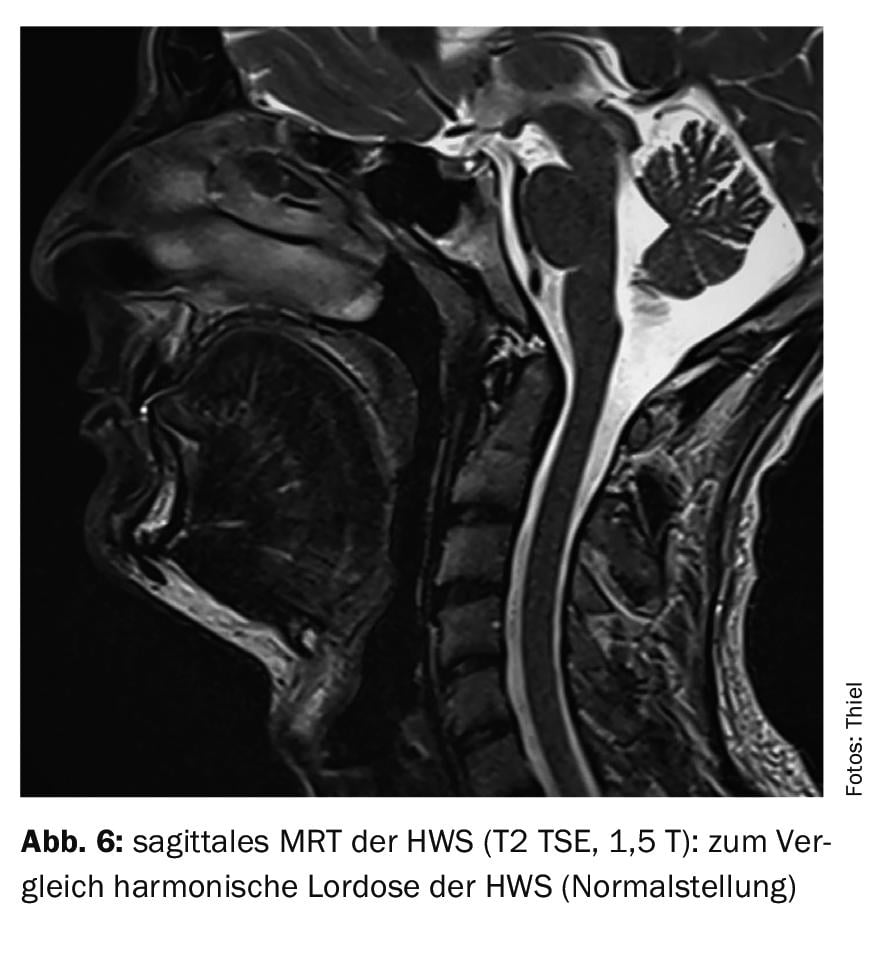
Sonography of the soft tissues of the neck is helpful in ruling out soft tissue space involvement or goiter. Computed tomography shows very precisely the bony extent of the degenerative changes, and with the 2D sagittal and coronary reconstructions, malstatics can be detected very well. Magnetic resonance imaging, with its high soft tissue contrast, offers advantages in the assessment of the intervertebral disc situation, myelon, ligaments, and musculature and is very good at detecting overload-related changes in the vertebrae (Modic classification).
Case studies
In case study 1 (Fig. 1A and B) a fracture should be excluded in a 77-year-old patient after distortion trauma of the cervical spine. Pre-existing cervical spine syndrome, also feeling of pressure and lumpiness in the throat with apparent dysphagia. In addition to the pronounced degenerative changes with hypertrophic spondylosis deformans in the cervicothoracic junction, misalignment was also demonstrated. For case 2 a porridge swallow was performed to exclude a diverticulum of the esophagus. Lateral radiography documented significantly marked synostosing spondylosis deformans of the upper cervical spine, as in disseminated idiopathic skeletal hyperostosis (DISH), with resultant stenosis of the lumen of the upper esophagus (Fig. 2) .

Case report 3 documents a hypertrophic spondylosis deformans in segment C3/4 and an extensor deformity in a 50-year-old patient with ankylosing spondylitis in addition to the initial bamboo rod aspect (Fig. 3) . Dysphagia was present.

A kyphotic buckling of the degenerated cervical spine (Fig. 4) of a 58-year-old female patient is demonstrable in case report 4, and there was considerable myogelosis. In case study 5 , there is a long-stretch deformity of the cervical spine and upper thoracic spine in a 56-year-old female patient with cervical spine syndrome including myogelosis and dysphagia (Fig. 5). Figure 6 is intended to provide a comparative view of the normal position (lordosis) of the cervical spine in a young patient with an MRI of the head.


Take-Home Messages
- In addition to true space-occupying lesions on the region of the hypopharynx, larynx, and the esophagus, degenerative changes of the cervical spine and faulty statics can also lead to dysphagia.
- Important indications of causative noxae can already be elicited from the anamnesis.
- The symptomatology requires interdisciplinary collaboration.
- Imaging techniques are important for differential diagnosis.
- The treatment of functional dysphagia can be done primarily with conservative measures.
Literature:
- Armstrong B, McNair P, Taylor D: head and neck position sense. Sports Med 2008; 38(2): 101-117.
- Ernst A, Freesmeyer B: Functional disorders of the head and neck. Georg Thieme Verlag Stuttgart, New York: 2008, pp. 32-42.
- Unger S, et al: Diastrophic Dysplasia. In: GeneReviews. Seattle (WA): University of Washington, Seattle: 1993-2022. 2004 Nov 15.
- Cervical syndrome. www.minimed.at/medizinische-themen/bewegungsapparat/zervikalsyndrom, (last accessed 07/13/2022)
HAUSARZT PRAXIS 2022; 17(8): 28-30











