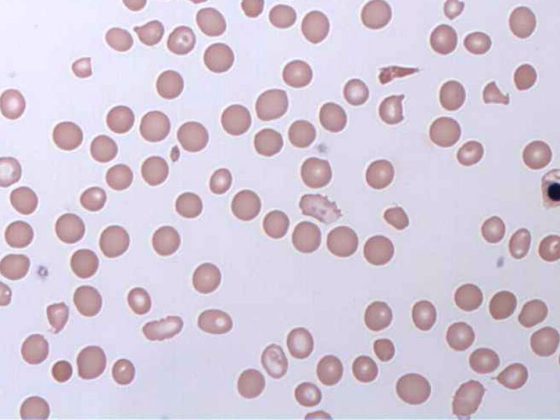
More than three quarters of all strokes are caused by an occlusion or narrowing of a blood vessel supplying the brain. This results in a reduced supply of oxygen and nutrients to this area of the brain. Permanent damage can only be prevented if the blood supply is restored as quickly as possible. Because the therapeutic window for neuroprotective measures is short – or is it?
In ischemic stroke, arteries supplying the brain are blocked and parts of the brain have a reduced blood supply, resulting in a lack of oxygen. Over time, the affected brain tissue dies. Approximately 16,000 strokes occur in Switzerland every year. Since the risk of stroke increases with age, a further increase in the stroke rate can be expected due to demographic change. The extent of tissue damage depends on the duration and severity of blood flow reduction. Care should be restored within 4.5 hours of the event, according to conventional wisdom.
Either the thrombus is dissolved with intravenous lysis therapy, or removed by vascular catheter intervention. However, a large proportion of those affected do not reach an appropriate hospital quickly enough. Only about 20% of all stroke patients receive drug therapy within the time window according to guidelines. The reasons are manifold, whether the affected person lives in a rural region or the symptoms are recognized too late. However, it is not uncommon for a stroke to occur while the patient is asleep, so that it is not until the patient wakes up that he or she realizes that something is wrong. Therefore, valuable time is often lost.
Is the time window longer than expected?
Recent study results now give hope [1]. They suggest that patients may benefit from thrombolysis beyond the 4.5-studen time window. At least if you showed a “diffusion-FLAIR mismatch” on MRI, which is considered a favorable pattern of findings. That is, all patients had an ischemic lesion visible on MRI diffusion-weighted imaging but no parenchymal hyperintensity in fluid-attenuated inversion recovery (FLAIR). In the multicenter study, they were then randomized to receive either intravenous alteplase (n=254) or placebo (n=249). After 90 days, a significantly better functional outcome and numerically more intracranial hemorrhages were observed in the alteplase group.
Thrombolysis also effective in the later course
In another study, the results were also positive [2]: in patients in whom the stroke occurred more than 4.5 hours (but not more than 9 hours) ago, lysis therapy was associated with a better clinical outcome. 225 patients were randomized in a 1:1 ratio. This was preceded by perfusion-diffusion MRI or CT to visualize the extent of infarction as well as at-risk tissue. The primary outcome was a score of 0 or 1 on the modified Rankin scale. The use of alteplase resulted in a higher percentage of patients with no or minor neurologic deficits than did the use of placebo. Accordingly, this treatment option should be available to more patients in clinical practice without completely disregarding time. Stroke patients must nevertheless be cared for as quickly as possible.
Registry study confirms study results
Studies usually examine highly selective patient groups. The results cannot always be reproduced in clinical practice. A German industry-independent registry study [3] analyzed a total of 2794 patients. Thrombectomy restored blood flow in 2143 patients (83%). Accordingly, good therapeutic results can also be achieved in daily routine.
Double is better for transient ischemic attack
If the stroke is not severe but merely a transient ischemic attack (TIA), the latest recommendations suggest that aspirin should not be the only treatment [4]. For a limited time (ten to 21 days), combination therapy of aspirin and clopidogrel is preferred. Thus, the rate of stroke recurrence, including cerebral hemorrhage, can be significantly reduced compared with only one antiplatelet agent [5]. In the study group that received aspirin and clopidrogrel, only 121 of 2432 patients experienced a major subsequent ischemic event. By contrast, in the group that had taken only aspirin and a placebo, 160 of 2449 patients did.
Literature:
- Thomalla G, Simonsen CZ, Boutitie F, et al: WAKE-UP Investigators. MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. N Engl J Med 2018; 379 (7): 611-622.
- Ma H, Campbell BCV, Parsons MW, et al: EXTEND Investigators. Thrombolysis Guided by Perfusion Imaging up to 9 Hours after Onset of Stroke. N Engl J Med. 2019; 380(19): 1795-1803.
- Wollenweber FA, Tiedt S, Alegiani A, et al: Functional Outcome Following Stroke Thrombectomy in Clinical Practice. Stroke 2019 Sep; 50 (9): 2500-2506.
- Prasad K, Siemieniuk R, Hao Q, et al: Dual antiplatelet therapy with aspirin and clopidogrel for acute high risk transient ischaemic attack and minor ischaemic stroke: a clinical practice guideline. BMJ. 2018; 363: k5130
- Johnston SC, Easton JD, Farrant M, et al: Clopidogrel and aspirin in Acute Ischemic Stroke and High-Risk TIA. N Engl J Med. 2018 Jul 19;379(3): 215-225.
InFo NEUROLOGY & PSYCHIATRY 2020; 18(1): 30.