At the DGHO congress in Vienna, the focus was on new targeted therapies designed to improve the quality of life of patients with malignant hematologic diseases. In particular, medical advances in the areas of myelodyplastic syndrome (MDS), myelofibrosis (MF), and chronic myeloid leukemia (CML) were highlighted.
By way of introduction, Prof. Dr. med. Wolf-Karsten Hofmann, Mannheim University Medical Center, posed the question of which patients benefit from iron chelation.
By means of transfusions of erythrocyte concentrates (EC), patients with myelodyplastic syndrome (MDS) can be treated supportively, but they run the risk of iron overload (serum ferritin >1000 ng/ml) after about 20 EC.
“Fundamentally, iron is an essential component of the body that participates in numerous important physiological functions such as O2 transport, gas exchange, biosynthesis, DNA synthesis and repair, and cell growth and proliferation. However, when the intestine can no longer absorb excess iron, genotoxic effects result, which are associated with damage to cell organelles, increased genomic instability, and premature cell death [1],” says Prof. Hofmann. “Since 80-90% of those with this condition are or become transfusion-dependent, iron chelation seems reasonable in low-risk MDS patients.”
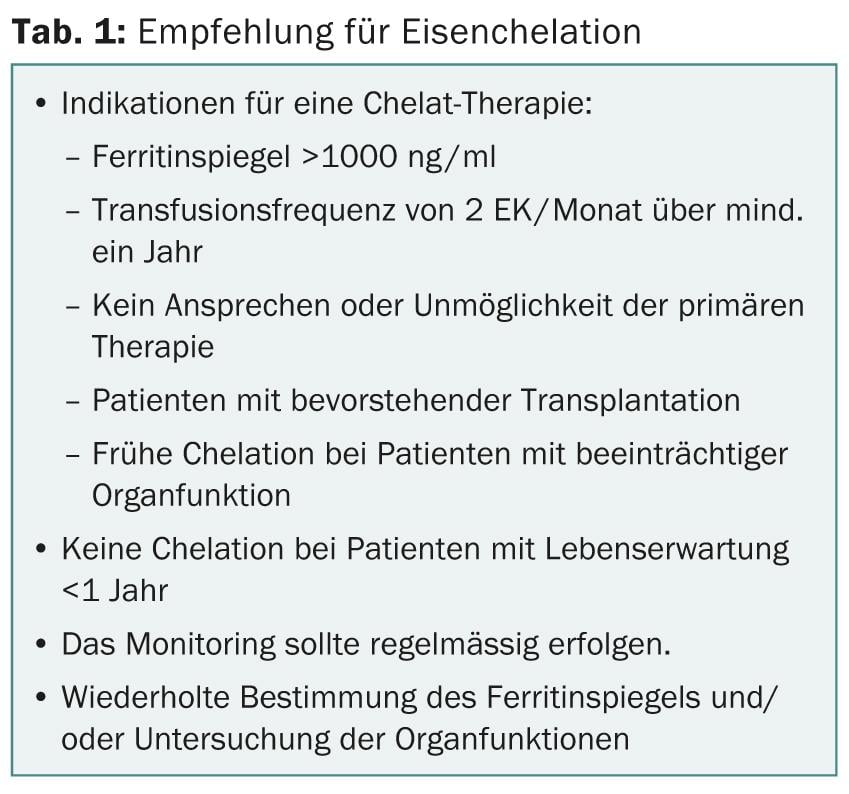
Specifically, several clinical studies, including one presented at ASH 2012, show a prolongation of overall survival in this study group [2–4]. Furthermore, chelation (e.g. with deferasirox, Exjade®) can lead to improved hematopoiesis, which in turn reduces the need for transfusion [5, 6]. The indications for iron chelation in MDS are summarized in Table 1.
The most common side effects are diarrhea and nausea, and somewhat less commonly vomiting, abdominal pain, bloating, rash, and constipation.
JAK1/2 inhibitor in myelofibrosis
“In myelofibrosis (MF), a neoplastic disease of the bone marrow, activation of JAK/STAT signal transduction is pathophysiologically crucial,” explained Prof. Andreas Reiter, MD, University Medical Center Mannheim, Germany.
Long-term data from a phase III trial comparing the JAK1/2 inhibitor ruxolitinib with “best available therapy” (BAT) showed a significant reduction in splenic volume [7]. In addition, the symptoms most commonly associated with MF improved significantly and persistently. These include: abdominal discomfort, pain under the left costal arch, rapid feeling of fullness, night sweats, itching, bone and muscle pain, and fatigue. In contrast, these factors worsened in the control group. The most common side effects during early treatment initiation included anemia and thrombocytopenia [8].
However, the initial decrease in mean hemoglobin value later converges back to the value of the BAT arm and remains stable in the long term [7]. “If the dip is too severe, it can be mitigated by temporarily reducing the dose,” Prof. Reiter explained.
Chronic myeloid leukemia
The BCR-ABL tyrosine kinase inhibitor (TKI) nilotinib (Tasigna®) has been available to patients with chronic myeloid leukemia (CML) for several years: According to Prof. Andreas Hochhaus, MD, University Hospital Jena, rapid response to TKI is the most important prognostic factor in the therapy of CML patients. Failure of therapy may cause progression to blast crisis (BK) and accelerated phase (AP) after a short period of time, which in turn significantly increases the risk of death.
“The first few years after diagnosis are quite crucial, as this is when progressions are particularly common, so in the early stages the disease must be addressed with efficient and fast-acting therapies,” Prof. Hochhaus added.
Early and profound response to new TKIs such as nilotinib in newly diagnosed CML patients, including those with prior imatinib therapy, appears to provide protection against progression and thus benefit life expectancy [9]. “Several independent studies showed that achieving a molecular response of <10% BCR-ABL as early as three months can be prognostic for longer overall survival. The European Leukemia Network (ELN) refers to this as an optimal response [10]. About 91% of nilotinib patients achieve this value,” Prof. Hochhaus said.
New concepts no longer aim only at progression prevention, but also at the possibility of safe and relapse-free discontinuation of therapy after prior reduction of disease burden to a level to be discussed.
Source: “Hematology Symposium: Patient Cases from Practice,” Novartis satellite symposium at the DGHO Congress, October 18-22, 2013, Vienna.
Literature:
- Gattermann N, Rachmilewitz EA: Ann Hematol 2011 Jan; 90(1): 1-10. doi: 10.1007/s00277-010-1091-1. Epub 2010 Oct 12.
- Leitch HA, et al: Leuk Res 2012 Nov; 36(11): 1380-6. doi: 10.1016/j.leukres.2012.08.001. Epub 2012 Aug 24.
- Remacha A, et al.: The IRON2 Study. A retrospective observational study to describe the evolution of iron overload in patients with low-risk myelodysplastic syndrome. ASH Annual Meeting Abstracts 2012; 120: #1723.
- Lyons RM, et al: Relationship between chelation and clinical outcomes in 600 lower-risk MDS patients : registry analysis at 36 months. ASH Annual Meeting Abstracts 2012; 120: #3800.
- Gattermann N, et al: Haematologica 2012 Sep; 97(9): 1364-71. doi: 10.3324/haematol.2011.048546. epub 2012 Mar 14.
- List AF, et al: J Clin Oncol 2012 Jun 10; 30(17): 2134-9. doi: 10.1200/JCO.2010.34.1222. epub 2012 Apr 30.
- Vannucchi AM, et al: Long-Term Outcomes From a Phase 3 Study Comparing Ruxolitinib With Best Available Therapy (BAT) for the Treatment of Myelofibrosis (MF): a 3-Year Update of COMFORT-II. Haematologica 2013; 98: Abstract #1111.
- Verstovsek S, et al: N Engl J Med 2012 Mar 1; 366(9): 799-807. doi: 10.1056/NEJMoa1110557.
- Hochhaus A, et al: Nilotinib shows sustained benefit compared with imatinib in patients (pts) with newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP): ENESTnd 4-year follow-up (f/u). Haematologica 2013; 98: Abstract #P712.
- Baccarani M, et al: Blood 2013 Aug 8; 122(6): 872-84. doi: 10.1182/blood-2013-05-501569. epub 2013 Jun 26.
InFo Oncology & Hematalogy 2013; 1(1): 37-38.