Although epinephrine is considered the treatment of choice for anaphylaxis, antihistamines or corticosteroids are used much more frequently in the acute situation. The latest research results and recommendations in this regard were discussed at the annual congress of the Swiss Society of Allergology and Immunology (SGAI) in Davos.
(rs) In light of the new Academy of Allergy and Clinical Immunology (EAACI) guidelines, current evidence on the epidemiology, prevention, diagnosis, and treatment of food allergy and anaphylaxis was summarized in systematic reviews.
Only three studies met the inclusion criteria for the systematic review on the epidemiology of anaphylaxis, so the power is likely to be limited [1]. Based on available studies, the overall prevalence of anaphylaxis in Europe was estimated to be over 0.3%. As shown, the incidence of anaphylaxis had increased globally during the periods studied (1990-1991, 2000-2001). However, on the basis of age stratification, it appeared that there had been an increase in anaphylaxis, particularly in the 0- to 4-year-old group. For the diagnosis of anaphylaxis, Prof. Phillipe Eigenmann, MD, University Children’s Hospital, Geneva, Switzerland, recommended the clinical criteria published in 2006 by Sampson et al. [2]. These take into account the different symptoms of anaphylaxis in adults and children.
For fear of an imminent circulatory collapse, the main focus in adults with acute anaphylaxis is usually on blood pressure. In contrast, anaphylaxis in children presents more frequently with respiratory or gastrointestinal symptoms. “It is quite possible that anaphylaxis in children starts with gastrointestinal symptoms, followed by skin symptoms and then respiratory symptoms,” the allergist said at the SGAI annual congress. For this reason, he said, monitoring oxygen saturation is more important than blood pressure control in children.
Different patient groups
Prof. Estelle Simons, MD, University of Manitoba, pointed out the characteristics of anaphylaxis in different age groups. Severe, sometimes fatal courses are known, especially in adolescents. The reasons for this lie in the behavior of adolescents, who accept exposure to triggers for social reasons, among others. Another cause is the failure to carry emergency medications. Fatal courses were observed mainly in adolescents suffering from severe uncontrolled asthma.
Pregnant women and the elderly are also among the most vulnerable groups. In the elderly, anaphylaxis may be the trigger for myocardial infarction or arrhythmias. Anaphylaxis in pregnancy is life-threatening and can cause severe neurological damage or death in both mother and child.
Common triggers
The main triggers identified on the basis of the systematic review were food, drugs, insect bites, and latex. The frequency of anaphylactic reactions to the specific allergens varied widely among the studies.
“It is also safe to say from practical experience that food allergies are most frequently observed in children,” Prof. Eigenmann said. One of the included studies identified cow’s milk as the most common cause of anaphylaxis in children. Common triggers also include peanuts and other nuts such as hazelnuts, as well as foods that lead to latex cross-allergy. Studies of drug triggers showed a high risk for blood plasma and penicillin i.v. Anaphylactic reactions to insect venom occurred most frequently after bee stings. An increased risk of systemic reaction was seen in individuals who also had atopic disease.
Anaphylaxis Management
The systematic review on acute and long-term therapy of anaphylaxis is based on an analysis of 55 studies [3]. Of these, 15 studies investigated the efficacy of epinephrine in the acute treatment of anaphylaxis. “These showed that prompt use of epinephrine can reduce the incidence of fatal anaphylaxis,” Prof. Eigenmann said.
Main risk factors for lethal outcome were preexisting asthma disease, delayed, incorrect, or nonuse of the autoinjector. The authors recommend prescribing prefilled syringes containing 0.3 mg epinephrine in children with a body weight of 25 kg or more. Below this limit, pre-filled syringes containing 0.15 mg epinephrine are available in Switzerland. Due to good absorption, injection into the thigh muscle (Musc. vastis lateralis) is recommended in both adults and children. An important question in the review was the need for a second epinephrine injection. As one study showed, multiple epinephrine injections were most needed in people who had additional asthma. “But that doesn’t mean you have to prescribe more than one autoinjector in all of these patients,” Prof. Eigenmann said. Increased body weight per se was not associated with repeated epinephrine injection, according to a study presented by Prof. Simons.
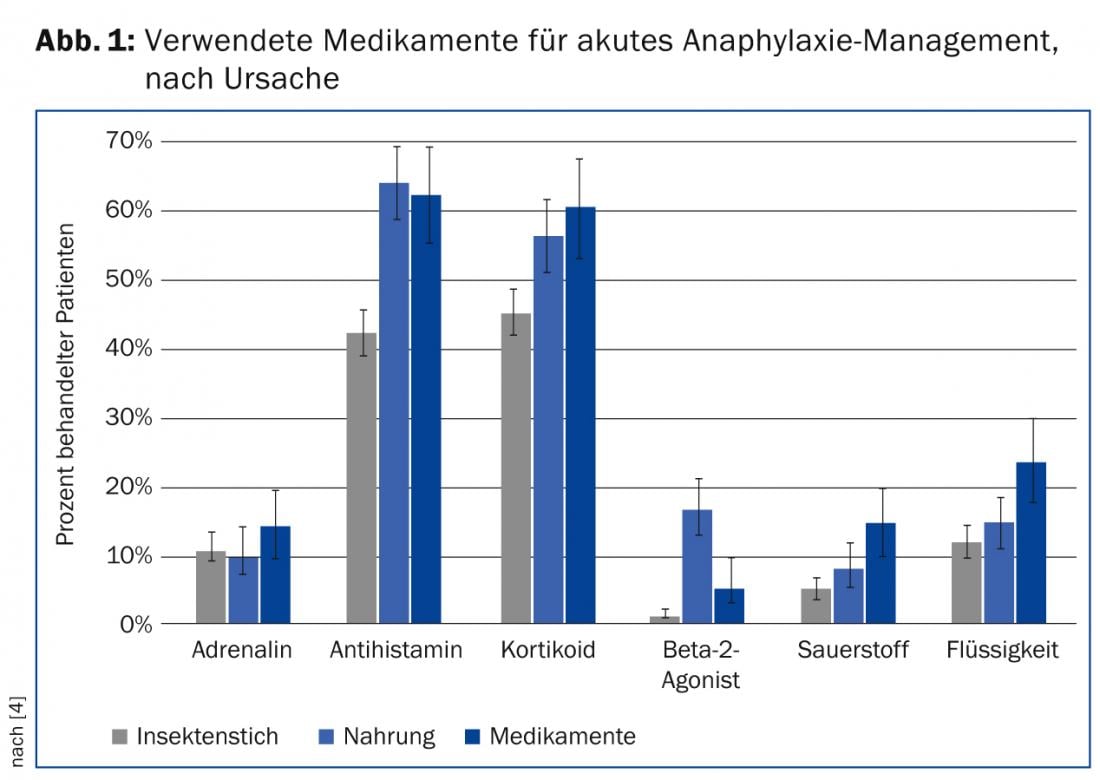
Adrenaline is recommended in guidelines as well as by the WHO for first-line treatment of acute anaphylaxis. However, the practice looks quite different, as an evaluation of the anaphylaxis registry with German, Austrian and Swiss data showed: Only 13% of the affected persons received adrenaline injections regardless of the trigger of the anaphylactic reaction – the majority of them i.v. It is estimated that half of the affected persons were primarily treated with antihistamines and corticoids (Fig. 1) [4]. Treatment was influenced by the age of the patient as well as by the trigger of the anaphylaxis. Children and young adults in particular received antihistamines and corticosteroids more frequently, which was attributed in part to the oral route of administration. Anaphylaxis from food and drugs led to increased therapy with corticosteroids and antihistamines, whereas insect bites were more likely to be treated with epinephrine.
Although antihistamines and corticosteroids are commonly used in the acute treatment of anaphylaxis, there are no studies demonstrating the benefit of this approach. Two Cochrane reviews of H1 antihistamines and corticosteroids concluded that none of the identified papers met the required inclusion criteria of a randomized controlled trial. Limited evidence was found for the use of H2 blockers. Similar conclusions were reached by the EAACI systematic review on the management of anaphylaxis.
Regional knowledge is essential
“The most important thing for the general practitioner is to have a good knowledge of the regional characteristics that can contribute to triggering anaphylaxis (such as a high number of beekeepers) and of his patients in general,” Prof. Eigenmann said. Turning to allergists, he said, “It is important that we train parents, schools, other institutions, and people involved in the care of children in the management of anaphylaxis.” This includes handling emergency medications, he said. “For fear of causing pain to children, many parents are unable to use the auto-injector,” Prof. Eigenmann said. “In Sweden, parents are therefore allowed to practice injecting with the used auto-injector under supervision.” Initial trials with this procedure at the University Hospital in Geneva have been positive.
Source: Annual Congress of the Swiss Society of Allergology and Immunology (SGAI/SSAI) and World Immune Regulation Meeting (WIM), March 20-21, 2014, Davos.
Literature:
- Panesar SS, et al: The epidemiology of anaphylaxis in Europe: a systematic review. Allergy 2013 Nov; 68(11): 1353-1361.
- Sampson HA, et al: Second symposium on the definition and management of anaphylaxis: summary report–Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol 2006 Feb; 117(2): 391-397.
- Dhami S, et al: Management of anaphylaxis: a systematic review. Allergy 2014 Feb; 69(2): 168-175.
- Grabenhenrich L, et al: Implementation of anaphylaxis management guidelines: a register-based study. PLoS One 2012; 7(5): e35778.
DERMATOLOGIE PRAXIS 2014; 24(2): 39-41











