Urinary incontinence and urinary tract infections are among the most common conditions in women, both of which are also difficult to manage. In addition to standard medications, hormone supplements may be considered off-label in postmenopausal women with proven hormone deficiency. The possibilities of such a therapy were discussed at the DGU Congress in Hamburg.
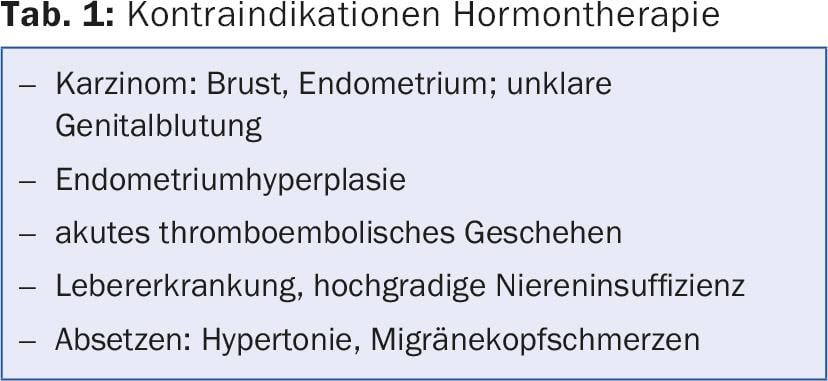
Hormone replacement after menopause is approved for vaginal symptoms that indicate estrogen deficiency, such as dryness, itching and dyspareunia, and atrophic vaginitis.Off-label, local hormone therapy can also be considered for urethral syndrome, urinary incontinence and recurrent urinary tract infections,” reported PD Dr. med. Winfried Vahlensieck, head physician of urology at the Kurpark-Klinik Bad Nauheim (D) – provided there is a hormone deficiency and there are no contraindications. (Tab. 1). A hormone deficiency can be detected very easily by vaginal pH measurement. Values ≤5 are normal.
Urinary incontinence
There are positive data on hormone therapy for urinary incontinence, especially in postmenopausal women with urge incontinence, for the vaginal use of estrogen. This option is also recommended in the European guidelines for the management of urinary incontinence [1]. In contrast, there is no evidence of benefit from systemic estrogen administration. “Taking the pill does not improve incontinence,” Dr. Vahlensieck said. Rather, the complaints increase.
Urinary tract infections
In patients with recurrent urinary tract infections (UTIs), i.e., ≥3 symptomatic UTIs per year or ≥2 within six months, alternatives to long-term prophylaxis with antibiotics are urgently sought. According to the urologist, problems are caused by candidiasis and other side effects of long-term use, which often lead to discontinuation of therapy, as well as insufficient compliance and resistant intestinal bacteria, which are usually the triggers of UTIs. In addition, many patients return to their old UTI frequency relatively quickly after antibiotic prophylaxis is discontinued.
In women at low risk for severe UTIs, other options for prevention include immune stimulation, probiotics, herbal medications, and, in post-menopausal women, hormone therapy with estrogens. As with urinary incontinence, intravaginal use is most appropriate, preferably with estriol at the low dose of 0.5 mg – equivalent to about 1 cm of ointment strand. During the first two to three weeks, therapy should be administered daily, then twice a week. Progesterone was not necessary. Three placebo-controlled trials have demonstrated the efficacy of vaginal estriol therapy in the prophylaxis of postmenopausal UTI [2,3].
As further options for prophylaxis, Dr. Vahlensieck mentioned influencing the vaginal apron colonization by intravaginal application of probiotics, especially lactobacilli (once or twice a week), as well as acidification of the urine, e.g. with L-methionine. “Antibacterial washing of the genital region, on the other hand, is counterproductive,” says Prof. Hansjürgen Piechota, MD, Johannes Wesling Klinikum, Minden (D). Because this could impair lactobacilli and even promote UTIs.
How to stimulate the immune system?
The urologist from Minden went into more detail about the possibilities of immune stimulation. In addition to nonspecific immunostimulation, specific immunoprophylaxis can be provided by peroral or systemic vaccination with cell wall fractions of uropathogenic pathogens such as E. coli. In E. coli-associated UTIs, vitamin D can also be supplemented for several months as a supportive measure, thereby achieving endogenous immune stimulation. Vitamin D promotes the release of the antimicrobial peptide cathelicidin from urothelial cells in the presence of coliform bacteria.
More options
Phytopharmaceuticals and cranberry products have a long tradition in the therapy of uncomplicated UTI or as an add-on in high-risk patients. According to Prof. Piechota, there is increasingly better evidence for the sugar D-mannose, which has a similar mechanism of action to cranberry extracts (inhibiting the attachment of bacteria to the urothelium). Two teaspoons of mannose are recommended once daily for prophylaxis, and two tablespoons three times daily for chronic recurrent UTI.
In addition, intravesical instillation of hyaluronic acid and chondroitin sulfate to build up the urothelial glucosaminoglycan layer has been well studied and effective. In a study of 40 women, instillation of 40 mg hyaluronic acid (once weekly for the first month, then once monthly for four months) reduced the UTI rate from an average of 4.3 per year to only 0.3 per year and extended the infection-free interval from 100 to 500 days [4,5].
There are no good data on acupuncture, Prof. Piechota added. In one study, efficacy was only slightly better than in patients treated with sham acupuncture.
Source: Forum session “Urological diseases in women and therapy options”, during the 67th Annual Meeting of the German Society of Urology (DGU), September 24, 2015, Hamburg.
Literature:
- Lucas MG, et al: EAU guidelines on assessment and nonsurgical management of urinary incontinence. Eur Urol 2012 Dec; 62(6): 1130-1142. update online 2015, http://uroweb.org/wp-content/uploads/EAU-Guidelines-Urinary-Incontinence-2015.pdf.
- Raz R, Stamm WE: A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. NEJM 1993; 329: 753-756.
- Perotta C, et al: Estrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev 2008 Apr 16; (2): CD005131.
- Constantinides C, et al: Prevention of recurrent bacterial cystitis by intravesical administration of hyaluronic acid: a pilot study. BJU Int 2004; 93(9): 1262-1266.
- Cicione A, et al: Intravesical treatment with highly-concentrated hyaluronic acid and chondroitin sulphate in patients with recurrent urinary tract infections: results from a multicentre survey. Can Urol Assoc J 2014 Sep; 8(9-10): E721-E727.
HAUSARZT PRAXIS 2015; 10(11): 36-37











