From top to bottom, PD Dr. med. Sandro F. Fucentese, Balgrist University Hospital, worked his way through the most common orthopedic diseases in family practice at the Update Refresher General Internal Medicine. He gave useful diagnostic and therapeutic tips on problems of the shoulder, hip, knee and foot.
“About one third of consultations in the practice are problems of the musculoskeletal system. One consequently encounters these ailments extremely frequently, which is why one should know where the possibilities of diagnosis and treatment lie and when a referral to the specialist is advantageous,” says PD Sandro F. Fucentese, MD, Balgrist University Hospital. First to the rotator cuff, which is often affected by pathologies. Rupture manifests with pain during overhead activities such as tennis or throwing sports, or as night pain. The pain normally radiates distally. Therapeutically, one should start conservatively, e.g. with physiotherapy/water therapy, occasionally combined with an injection. It is about the restoration of passive mobility. If there is no response to these measures, a high degree of suffering and, at the same time, adequate muscle and tendon quality, surgical reconstruction should be considered. “However, the joint or shoulder must be centered in order to be reconstructed,” the speaker explained. “In addition, there must be no infectious situation or frozen shoulder.”
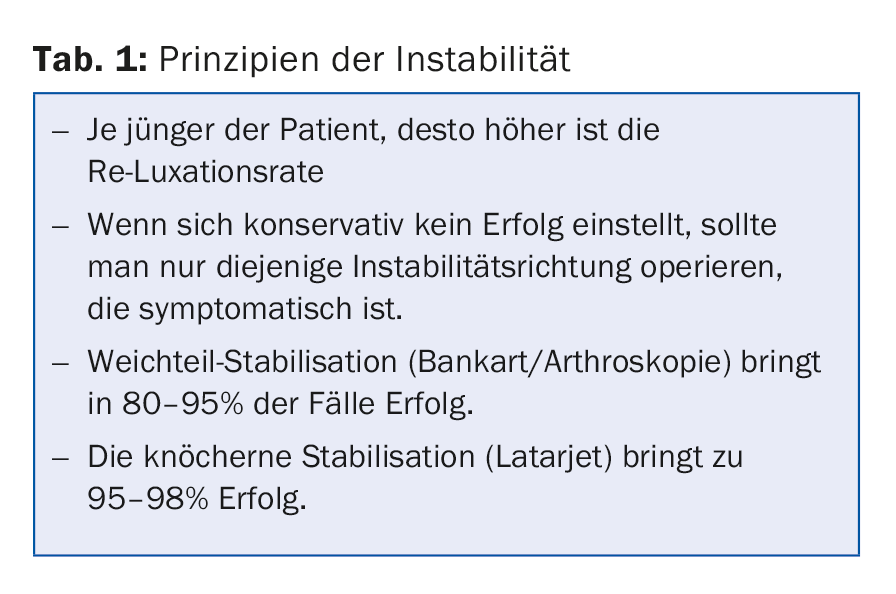
Also common is shoulder dislocation, with over 90% of cases dislocating anteriorly. If dislocation is suspected, an X-ray is indicated before reduction to rule out fracture, otherwise the femoral head is at risk of destruction. If the feeling of instability persists after reduction, the “apprehension sign” to the front or back (defensive posture) represents a classic finding. A surgical procedure with very low recurrence rates that is favored, especially in young athletes, is the Latarjet procedure [1]. Important notes on instability are listed in Table 1.
Hip diseases
Hip disease often manifests itself in the form of pain and limping. Etiologic possibilities are varied, ranging from idiopathic to inflammatory/toxic to mechanical causes. Dr. Fucentese elaborated on the latter.
Hip dysplasia is typically associated with pain on the side and a waddling gait. The Trendelenburg sign can also be observed (tilting of the pelvis to the healthy side while standing on one leg on the diseased leg). Key clinical findings are acetabular rim syndrome (when you stress the acetabular rim, the patient has pain), apprehension, and just lateral pain. Reorientation of the acetabulum in space is achieved by periacetabular pelvic osteotomy, i.e., hip surgery.
Another mechanical cause of hip problems is femoroacetabular impingement (FAI). This is a conflict between the femur and acetabulum, which manifests as groin pain in a flexed hip position (typically when sitting) and limited hip mobility. “We see a lot of patients with this pathology who had been treated repeatedly with a diagnosis of ‘adductor strain,'” he said. “Typical examination findings are decreased internal rotation and a positive impingement test. In the past, FAI was more commonly treated with open surgery, but today it is more commonly treated with hip arthroscopy, which produces the same results.”
Regarding osteoarthritis, it should be said that the indication for a prosthesis should be strict. “Don’t operate too fast,” is the motto. “Survival of the prosthesis is limited, especially in boys, so this is something to keep in mind.”
Knee injuries
Immediate intra-articular effusion after trauma is common and very painful. Differential diagnoses for knee distortion are:
- intra-articular fracture
- Patellar luxation
- ligamentous injury
- Meniscus lesion
- Cartilage damage.
An MRI is also performed relatively quickly in Switzerland compared to other countries – but the question of whether it is really needed immediately is justified.
In acute therapy, surgery is not mandatory, but rather depends on additional injuries (menisci, ligaments) and the expectation resp. Patient activity. “Not operating, then, doesn’t mean not doing anything,” Dr. Fucentese explained. “In the conservative line of therapy, you start with a rehabilitation program to reduce swelling, promote mobility, proprioception and build strength.” Later, with chronic anterior instability, surgery is an option if there are feelings of unsteadiness, irritable effusion, load-dependent knee pain and clinically a positive Lachman/pivot shift test.
The meniscus is designed to absorb pressure and is a stabilizer, Dr. Fucentese said, summarizing the two most important functions of the joint body. Meniscal injuries can be traumatic (common in younger patients) or degenerative (sudden or slow onset of symptoms, no history of trauma). Pain provocation by rotational movements is a classic meniscus sign. Again, the MRI scan is not always necessary, but is frequently done these days. In older patients, conservative measures (physio, infiltration) are more likely to be used first, and surgery only if pain persists. The latter includes knee arthroscopy with suturing (in younger patients) or partial meniscectomy.
Gonarthrosis can also be managed conservatively with NSAIDs, intra-articular steroids and physiotherapy. Operatively, a joint-preserving (young patient) or joint-replacing (old patient) procedure is chosen. Joint-preserving valgization osteotomy (goal: overcompensate for load line). “Arthroplasty is a one-way street,” Dr. Fucentese noted. “It is used when the patient is suffering a lot and the deformity is increasing with bone loss, limitation of movement or ligamentous insufficiency. But you have to let the patient know that this is a replacement and not a new knee.” Patients are often satisfied with even a partial prosthesis.
“We shun infections in knee arthroplasty like the devil shuns holy water,” the speaker said. This is a very rare but extremely serious complication. Treatment is always surgical; it is best for the patient to return to the surgeon. It is important to force the diagnosis. Antibiotic therapy before knee puncture is not indicated. “Such blind flights should be avoided at all costs; germs are becoming more aggressive and resistance is increasing,” Dr. Fucentese warned.
Hallux valgus – when to operate, how to follow up?
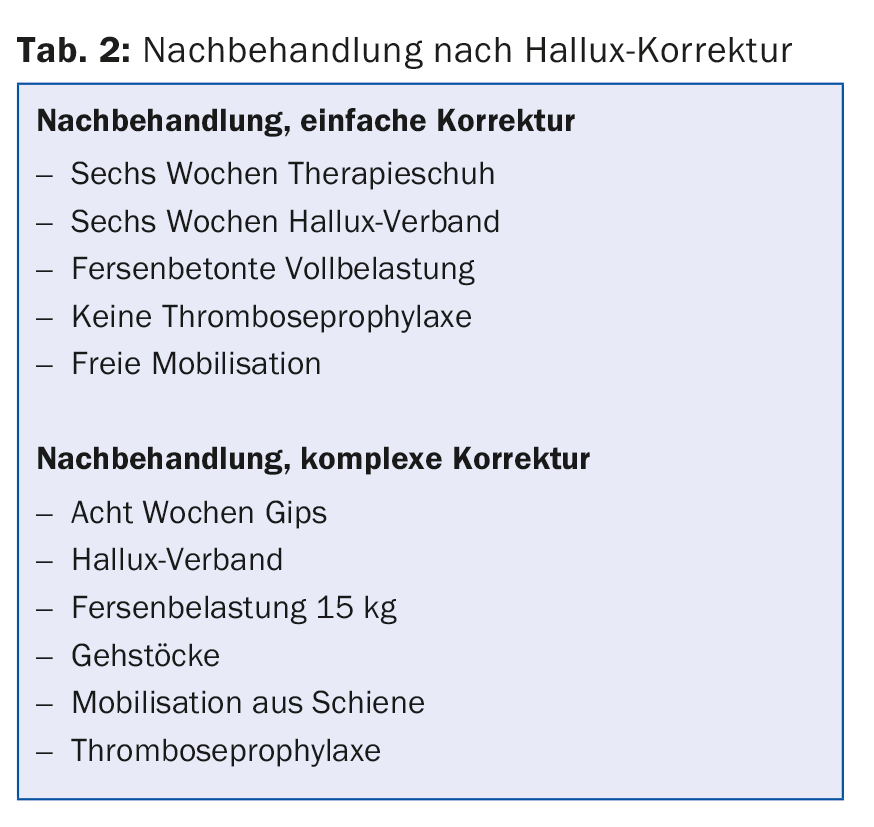
Hallux valgus affects women up to four times more often than men (onset usually between the ages of 30 and 50). Both genetics and footwear play a role in its development. Hallux valgus is a dynamic problem, which is why night splints, functional splints, silicone wedges or hallux socks work well for a while, but ultimately cannot prevent the hallux. After conservative therapy (physio, insoles, shoes) has been exhausted, in the case of pressure points and pain, but not for purely cosmetic reasons, the problem can be corrected surgically. The differences in aftercare following simple or complex hallux correction are shown in Table 2.
Metatarsalgia
Causes of metatarsalgia can be overloading of the bony or nervous structures. There are good conservative treatment options: Shoe insoles with support, stretching of calf muscles, local injection (nerves).
Source: General Internal Medicine Update Refresher, May 10-13, 2016, Zurich.
Literature:
- Latarjet M: [Treatment of recurrent dislocation of the shoulder]. Lyon Chir 1954 Nov-Dec; 49(8): 994-997.
HAUSARZT PRAXIS 2016; 11(6): 30-32