Among the various surgical methods for reconstructing the nose, paramedian forehead flap surgery has proven to be the gold standard, especially for large and full-thickness defects of the nose. The tissue in the forehead area is used for the defect to be reconstructed on the nose in the form of a pedicled flap. The versatility of paramedian forehead flap surgery makes it possible to successfully reconstruct complex nasal defects in terms of size, shape and position, achieving both esthetic and functional results.
The reconstruction of defects on the nose is complex and demanding, as both esthetic and functional aspects must be taken into account. Substance defects on the nose are usually caused by the resection of malignant tumors. These can affect the skin in isolation or spread to the cartilage framework and inner lining, causing so-called full-thickness nasal defects. Among the various surgical methods for reconstructing the nose, paramedian forehead flap surgery has proven to be the gold standard, especially for large and full-thickness defects of the nose. The tissue in the forehead area is used for the defect to be reconstructed on the nose in the form of a pedicled flap. The versatility of paramedian forehead flap plasty, especially in combination with cartilage grafts, makes it possible to successfully reconstruct complex nasal defects in terms of size, shape and position, achieving both esthetic and functional results.
History
The technique of frontal lobe plastic surgery has its origins in the early 19th century, when Johann Dieffenbach developed basic surgical procedures for tissue transfer. Dieffenbach experimented for the first time with skin grafts from the forehead region for the reconstruction of nasal defects. During the First World War, the efforts of surgeons such as Harold Gillies and his colleagues contributed to the further development of frontal lobectomy [1]. They adapted the technique to treat facial injuries, including severe nasal defects, in war casualties. In the following decades, frontal lobe plastic surgery was continuously refined and further developed. Surgeons such as Gordon Burget and Frederick Menick revolutionized the technique in the 1980s with the introduction of paramedian forehead flap plasty for the reconstruction of nasal defects [2,3].
Aesthetic subunits of the nose
When reconstructing nasal defects, it is crucial to respect and reconstruct the esthetic subunits of the nose. These comprise the following nine units: Nasal bridge, nasal tip, nasal slope, nasal bridge, nasal wings and the so-called soft nasal triangle [3]. As a result, scars along the esthetic subunit are the least noticeable as they lie between the natural convexities and concavities of the nose. According to this principle, if the defect affects more than 50% of a subunit, the rest of the esthetic subunit should be excised to allow subsequent reconstruction of the entire subunit. However, this procedure must be discussed individually with the patient, particularly in view of the resulting defect size and the patient’s age and any comorbidities.
Principle of reconstruction of full-thickness nasal defects
The reconstruction of full-thickness nasal defects initially involves careful preoperative planning and informing the patient about the multi-stage procedure with intervals of approx. 3-4 weeks [4,5]. The size of the nasal defect and the need for cartilage and/or bone grafts are taken into account. If the size of the defect to be reconstructed does not allow primary closure on the forehead, expansion of the skin with a tissue expander or closure of the donor area with a skin graft can be discussed with the patient. However, the latter should be avoided due to the relatively poorer esthetic result.
The reconstruction of nasal defects using paramedian forehead flap surgery was originally conceived as a two-step procedure, although three operations are now generally required to achieve an aesthetically pleasing result. In the first operation, the paramedian frontal lobe is dissected, followed by transposition and rotation of the flap into the defect. After approx. 3-4 weeks, aesthetic refinement, e.g. thinning of the flap, possibly in combination with reconstruction of a cartilage or bone defect, can be performed. The actual separation of the flap pedicle takes place after another 3-4 weeks. At this point, autonomization of the blood supply can be assumed [5].
Operation steps in detail
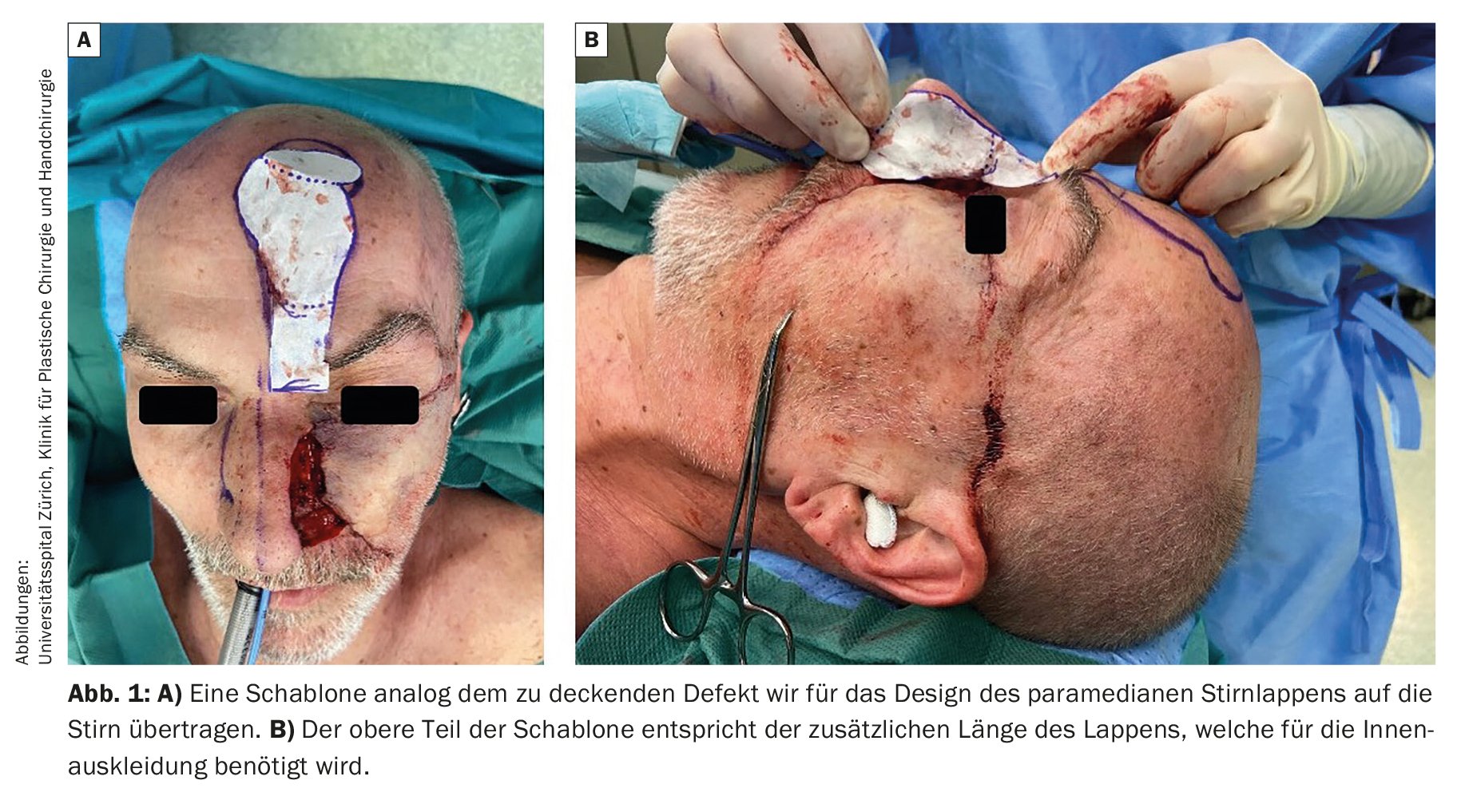
At the beginning of the operation, the design of the paramedian frontal flap is analogous to the defect to be covered. If additional reconstruction of the inner lining is necessary, this must be included in the size of the flap (Fig. 1A and 1B) . The supratrochlear artery is then marked on the skin in the area of the eyebrow using a Doppler (Fig. 2A). In addition, the incision is marked on the forehead region. Next, the frontal lobe is completely incised (Fig. 2B) and lifted subcutaneously in order to achieve the thinnest possible flap for the defect. Subsequently, a change is made to a submuscular preparation (Fig. 2C) . In order not to jeopardize the neurovascular structures, the flap pedicle is prepared subperiosteally from approx. 2 cm above the eyebrow (Fig. 2C) .
After sufficient mobilization, the flap can be rotated and fitted into the defect. The temporary flap pedicle can be covered with Epigard, for example, for protection (Fig. 3A). In the area of the eyebrow, the skin must be loosely closed to prevent the flap pedicle from being compromised. If primary closure in the forehead area is not possible, small defects can also heal secondarily (Fig. 3B and 3C).
The cartilage is usually reconstructed in a second step. The flap is lifted again after approx. 3-4 weeks (Fig. 4A) . Cartilage grafts can be harvested either from the nasal septum, retroauricularly or the ribs, depending on their size. These are then prepared according to the defect and fixed to the existing nasal framework (Fig. 4B) . The flap is then thinned out if necessary and sutured in place again (Fig. 4C and 4D).
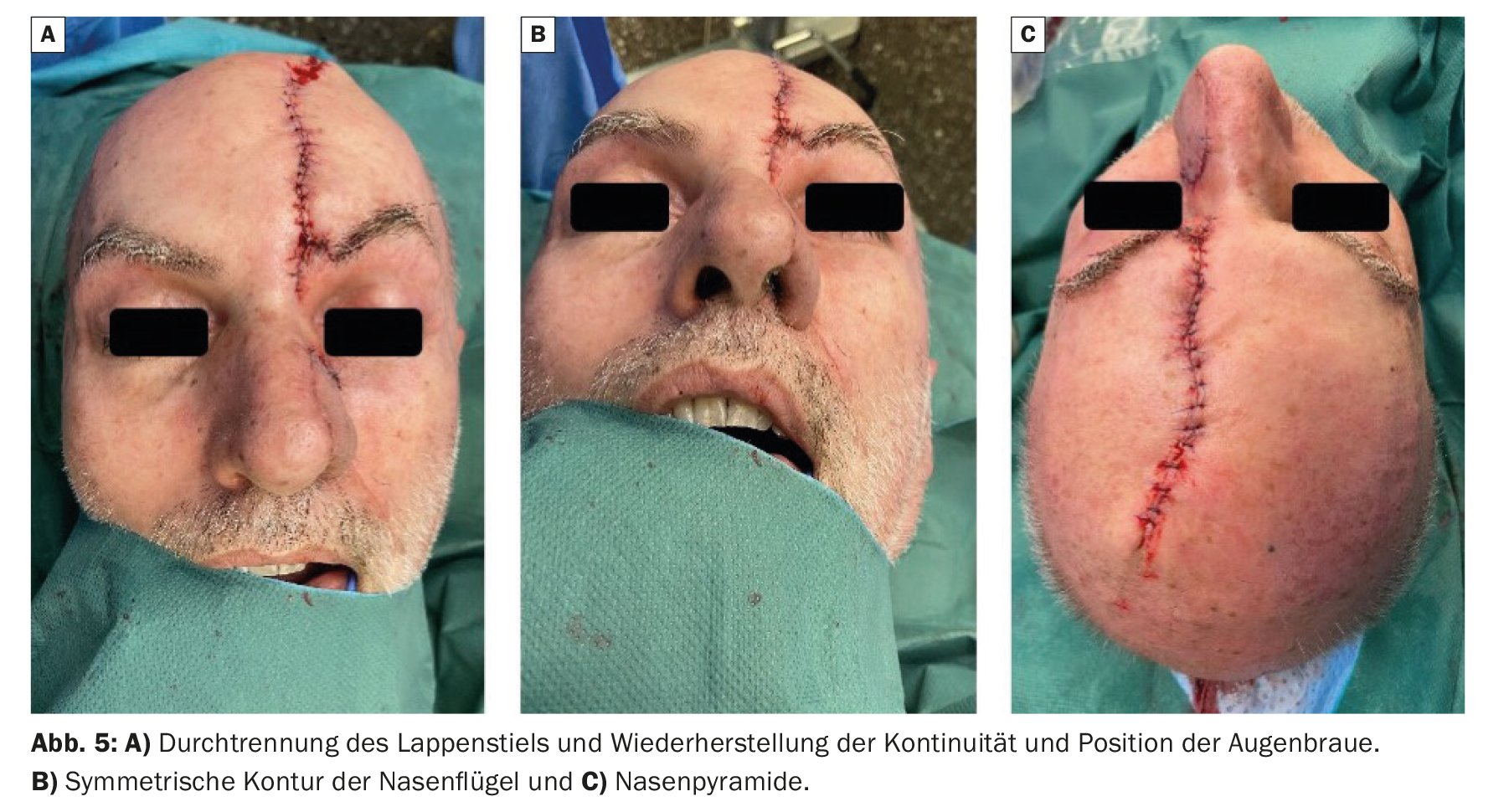
After a further four weeks, if the result is aesthetically and functionally satisfactory, the flap pedicle can be cut and the correct position of the eyebrow restored (Fig. 5A and 5B). At this point, the vertical scar on the forehead can be surgically corrected again if necessary (Fig. 5C) .
Postoperative care
Between operations, patients receive close outpatient care, especially as the repeated operations can be psychologically stressful and some patients feel ashamed and socially withdrawn due to the conspicuously connected flap pedicle. Caring and professional patient care is therefore essential.
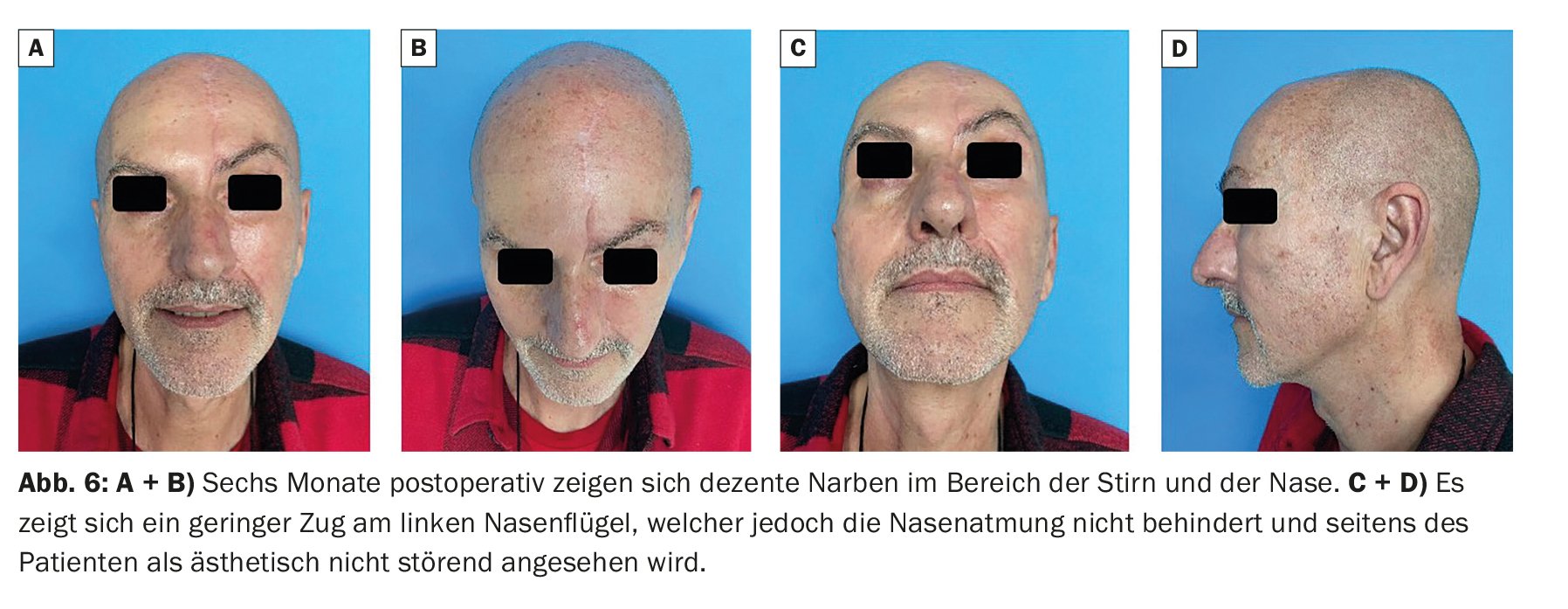
Regular follow-up examinations are also carried out after flap stalk transection (Fig. 6). The focus here is on both aesthetics and function, especially nasal breathing. Further fine adjustments can be made to achieve optimum results.
Take-Home-Messages
- When reconstructing defects on the nose, esthetic and functional aspects must be taken into account.
- When reconstructing defects on the nose, the esthetic subunits should be respected.
- Paramedian forehead flap plasty involves a multi-step procedure with intervals of 3-4 weeks, in which tissue from the forehead is rotated into the defect in the form of a pedicled flap.
- Additional cartilage or bone grafts are required to reconstruct the nasal framework.
Literature:
- Correa BJ, Weathers WM, Wolfswinkel EM, et al: The forehead flap: the gold standard of nasal soft tissue reconstruction. Semin Plast Surg 2013; 27(2): 96-103.
- Menick FJ: Aesthetic refinements in use of forehead for nasal reconstruction: the paramedian forehead flap. Clin Plast Surg 1990; 17(4): 607-622.
- Burget GC, Menick FJ: The subunit principle in nasal reconstruction. Plast Reconstr Surg 1985; 76(2): 239-247.
- Santos Stahl A, Gubisch W, Haack S, et al: Aesthetic and Functional Outcomes of 2-Stage Versus 3-Stage Paramedian Forehead Flap Techniques: A 9-Year Comparative Study With Prospectively Collected Data. Dermatol Surg 2015; 41(10): 1137-1148.
- Santos Stahl A, Gubisch W, Fischer H, et al: A Cohort Study of Paramedian Forehead Flap in 2 Stages (87 Flaps) and 3 Stages (100 Flaps). Ann Plast Surg 2015; 75(6): 615-619.
DERMATOLOGY PRACTICE 2024; 34(1): 8-11