Basal cell carcinoma is the most common form of skin cancer. Increasing incidence rates have been observed in recent decades. Predilection sites are sun-exposed skin areas in the head and neck region. According to the current guideline, photodynamic therapy (PDT) can be used for the treatment of superficial basal cell carcinoma, especially when contraindications to surgery are present.
Photodynamic therapy (PDT) is an established procedure for actinic keratoses and superficial basal cell carcinoma. Although basal cell carcinoma (BCC) has low rates of metastasis and mortality, BCC can lead to significant morbidity: on the one hand, due to its clustered occurrence in cosmetically sensitive areas and, on the other hand, due to its locally infiltrative and destructive growth, which, in the absence of or inadequate therapy, can lead to advanced findings years later [1]. In Switzerland, PDT is approved for the treatment of superficial basal cell carcinoma (sBCC) and thin nodular BCC (nBCC). Advantages of photodynamic therapy are good to very good aesthetic results, and outpatient performance – therapy of immunosuppressed patients is also possible [2,3]. For pain relief, the current guideline recommends local anesthesia or the administration of cold air [4]. Typically, pain begins during red light exposure and lasts only a few hours.
PDT with 5-ALA or MAL: largely selective effect on tumor tissue.
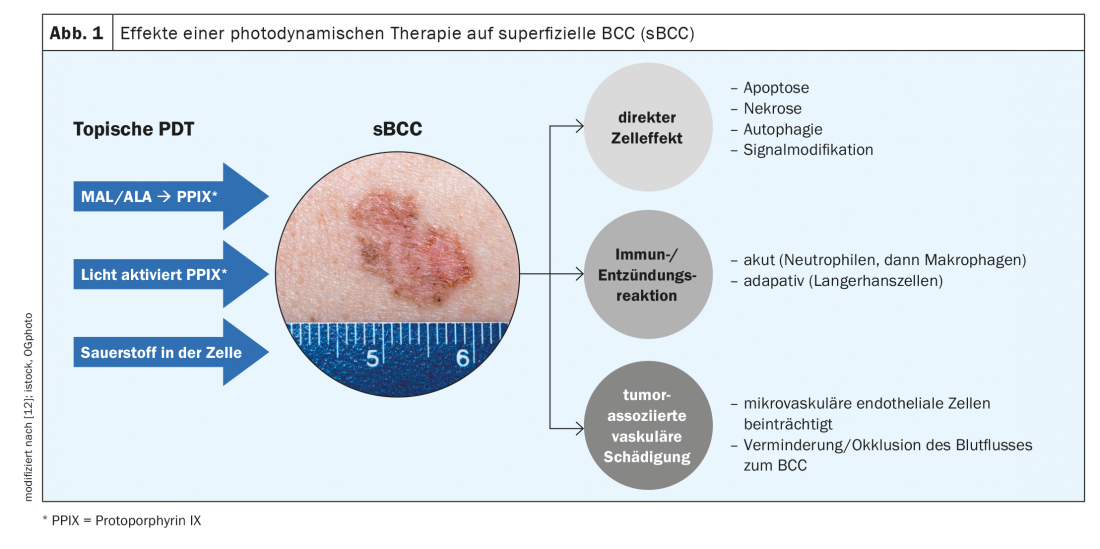
The principle of photodynamic therapy is based on the selective accumulation of so-called photosensitizers in the diseased tissue. In conventional PDT, 5-aminolevulinic acid (5-ALA) or methyl-aminolevulinate (MAL) are applied topically and converted to the photosensitizer protoporphyrin IX (PPIX) in tumor tissue [4]. This is followed by red light irradiation with a wavelength of 570-670 nm [4]. The singlet oxygen generated intracellularly in the course of PPIX activation leads to tumor cell destruction. Photodynamic therapy has a largely selective effect on the tumor tissue (Fig. 1) . Two therapy sessions are performed per treatment cycle at intervals of one week [1]. Pretreatment to remove crusts is recommended [5]. Side effects such as pain, redness, and crusting are usually well tolerated and rarely lead to treatment discontinuation after detailed explanation [6].
High healing rates for superficial and thin nodular basal cell carcinomas
Randomized trials showed a 92-97% cure rate for sBCC with MAL-PDT, with a 9% recurrence rate after one year [7,8]. Healing rates up to 89% have also been achieved for ALA-PDT in sBCC [9]. For MAL-PDT in thin nodular BCC, cure rates of 91% have been reported, with 76% of patients still tumor-free at 5 years. In a meta-analysis including 596 nBCC from 5 RCTs, tumor freedom of 79% was achieved after MAL-PDT at 5 years [10].
While PDT with daylight can also be used for the treatment of actinic keratoses, only irradiation with a special red light lamp is currently approved for BCC in Switzerland [2,11].
Literature:
- Seidl-Philipp M, et al. Journal of the German Dermatological Society 2021; 19(7): 1021-1043.
- Collier NJ, Ali FR, Lear JT: Lasers Med Sci 2015; 30(4): 1407-1409.
- Alter M, et al. Journal of the German Dermatological Society 2015; 13(9): 863-874.
- S2k guideline basal cell carcinoma of the skin, long version, 032-021, (2017/18 update).
- Kuijpers D, et al: J Drugs Dermatol 2006; 5: 642-645.
- Hommel T, Szeimies RM: Akt Dermatol 2018; 44: 30-36.
- Basset-Seguin N, Ibbotson SH, Emtestam L: Eur J Dermatol 2008; 18: 547-553.
- Szeimies RM, Ibbotson S, Murrell DF: J Eur Acad Dermatol & Venereol 2008; 22: 1302-1311.
- Peng Q, et al: Cancer 1997; 79: 2282-2308.
- Zou Y, et al: Journal of Cosmetic Dermatology 2016; 15, 374-382.
- Wiegell SR, Skødt V, Wulf HC: J Eur Acad Dermatol & Venereol 2014; 28(2): 169-175.
- Collier NJ, Rhodes LE: Molecules 2020; 25: 5398.
DERMATOLOGY PRACTICE 2022; 32(3): 33
InFo ONCOLOGY & HEMATOLOGY 2022; 10(4): 18.











