The enzyme tryptase, which is produced almost exclusively by mast cells, is considered a significant parameter in suspected MCAS. If the event-related increase in tryptase compared with symptom-free intervals exceeds a certain threshold, this is indicative of mast cell involvement. Another important criterion is the response to therapy with mast cell-specific drugs such as antihistamines or mast cell stabilizers. With an individualized treatment strategy, mast cell syndrome can generally be managed well.
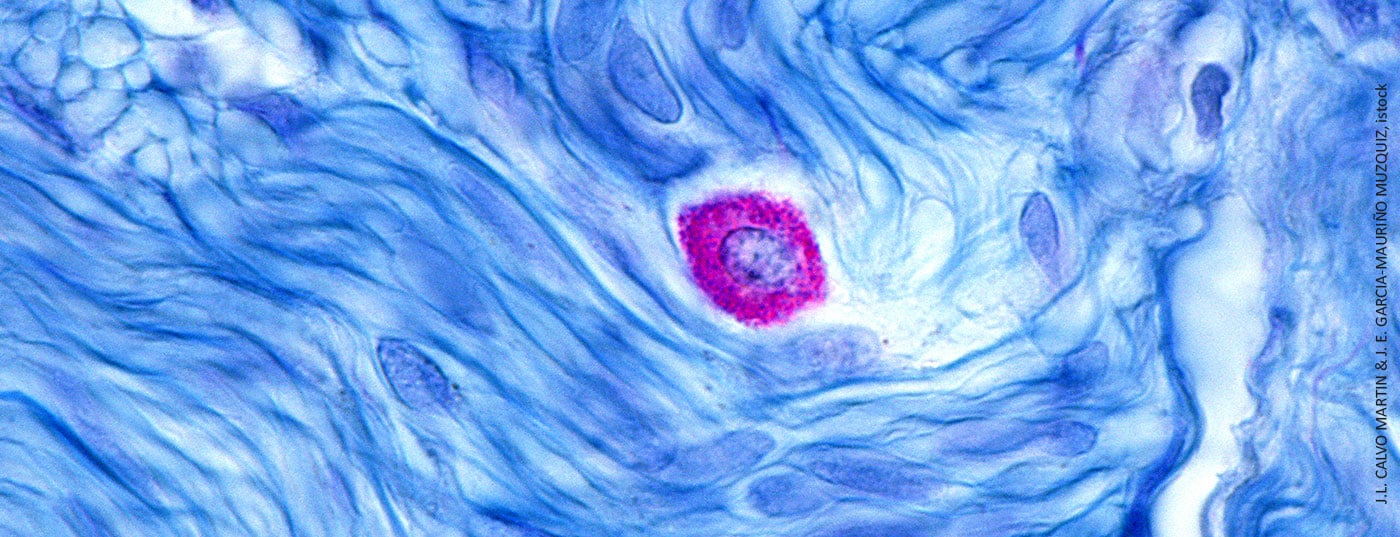
Mast cell diseases are characterized by excessive accumulation of mast cells in body tissues. Mast cell activation (MCA) occurs when certain trigger factors result in an unregulated increased release of vasoactive and proinflammatory mediators such as histamine, tryptase, prostaglandins, or leukotrienes (Table 1). Patients with recurrent symptoms of mast cell activation should be evaluated to determine whether they may have mast cell activation syndrome (MCAS). Symptom severity in MCAS is associated with the extent of mediator release. In severe cases of mast cell activation, the symptomatology is comparable to anaphylaxis. The likelihood of being an MCAS is increased if at least two of the following organ systems are involved: cutaneous, cardiovascular, pulmonary, gastrointestinal.

In the case of acute symptoms, the first step is to stabilize the condition. Subsequently, the following should be documented [1]: (i) Severity of reaction, (ii) Systemic response and organ systems involved. (iii) Course: recurrent vs. non-recurrent, (iiii) Mast cell activation (laboratory chemical evidence).
Transient increase in tryptase levels as an important marker
Claudia Lang, MD, from the Dermatology Clinic of the University Hospital Zurich, reports that experience has shown that patients who present to a physician/dermatologist often suffer considerably [2]. Due to the wide range of symptoms, they often go through a years-long odyssey of medical investigations until the correct diagnosis is made [3]. The suspected diagnosis of MCAS is confirmed when an event-related transient increase in serum tryptase levels is detected, the speaker explained [2]. Since tryptase is specific for mast cells and significantly more stable than histamine, it is a well-suited parameter for detecting mast cell activation [4]. It is true that tryptase is also present in basophils, but in much smaller amounts. The most favorable time to detect a tryptase increase is 1-4 h after an anaphylactic event [1,5]. The measured values are to be compared with the individual baseline tryptase levels. If baseline values are not available, they can be obtained at the earliest 24-48 h after the disappearance of all symptoms [1]. Regarding threshold, after studies on tryptase kinetics, it has emerged that an acute tryptase value of ≥20% above the individual basal value plus 20 ng/ml makes mast cell activation likely as the cause of the reaction [1]. An event-related tryptase increase is among the three consensus-based MCAS criteria [1,6]:
- typical clinical signs of severe recurrent acute systemic MCA (especially clinical features of anaphylaxis)
- Demonstrable mast cell involvement with an event-related increase in tryptase compared with symptom-free intervals: 20% from baseline plus 20 ng/ml
- Response to therapy with mast cell specific drugs.
All three criteria must be met for a diagnosis of MCAS [1]. Differential diagnosis should exclude secondary causes (e.g., mastocytosis, IgE-dependent allergy, inflammatory diseases) [7,8]. If baseline tryptase levels remain elevated after an event (>20 ng/ml) this may be indicative of underlying diseases such as hereditary α-tryptasemia or systemic mastocytosis.
Therapeutic measures include avoidance of trigger factors and the use of H1 antihistamines or mast cell stabilizers. It is taken as a permanent medication or as needed. Other agents to be considered include leukotriene antagonists or prostaglandin synthesis inhibitors. A histamine-reduced diet may be helpful, but a blanket recommendation for a histamine-free diet is not necessarily useful [2].
When MCAS patients face surgery : What to do?
Anesthesiologic techniques have improved in recent years. Complications can be avoided by adjusting preoperative, intraoperative, and postoperative management, Dr. Lang explained [2]. For this purpose, the following points should be considered:
- Avoidance of certain anesthetics, analgesics, antibiotics, and muscle relaxants if known intolerance.
- In patients with documented previous anaphylaxis: premedication with prednisolone and H1 and H2 antihistamines approximately 30 min before the procedure.
- Premedication should also be considered in situations that are difficult to assess
- in severe cases, omalizumab can be considered as a prophylactic treatment.(Omalizumab binds to IgE and thus prevents IgE from binding to the high-affinity FcεRI receptor. At the same time, the activation threshold of mast cells increases [12])
Congress: Swiss Society of Allergology and Immunology
Literature:
- Valent P, et al: J Allergy Clin Immunol Pract 2019; 7(4): 1125-1133.
- Lang C: Mast Cell Activation Syndrome (MAS) / Unspecific Histamine Liberation: Myths and Facts. Claudia Lang, MD. Allergology and Immunology Update AIU. 28.-30.01.2022.
- “The Causes of Post-Covid Syndrome – Treating Corona Long-Term Consequences Causally/How Persistent Viruses, Autoimmune Inflammation, and Mast Cell Activation Lead to Long Covid,” https://drjacobsinstitut.de (last accessed 04/05/2022).
- Pejler G, et al: Mast cell proteases. Adv Immunol 2007; 95: 167-255.
- Kristensen T, et al: Allergy 2017; 72: 1737-1743.
- Valent P, et al: Int Arch Allergy Immunol 2012; 157: 215-225.
- Vitte J, et al: J Allergy Clin Immunol Pract 2021; 9(8): 2994-3005.
- Ebo DG, et al: J Allergy Clin Immunol Pract 2021; 9(8): 3051-3059.
- Thermo Fisher Scientific Inc (SE): ImmunoCAP tryptase. Directions for use, www.phadia.com (last accessed Apr. 05, 2022).
- Swiss Histamine Intolerance Society (SIGHI), www.mastzellaktivierung.info, (last accessed 04/05/2022).
- Afrin LB, et al: The Amercian Journal of the Medical Sciences 2017; 353(3): 207-215.
- Lemal R, et al: The journal of allergy and clinical immunology In practice 2019; 7(7): 2387-95.e3.
DERMATOLOGIE PRAXIS 2022; 32(3): 36-37 (published 6/14/22, ahead of print).