Treatment of main-stem stenosis and multivessel disease by PCI is equivalent to bypass surgery when the syntax score is low. The complexity of coronary stenoses is crucial for the therapeutic decision: the more complex, the more advantages bypass surgery has. Diabetics in particular benefit from bypass surgery for multivessel disease. The individual therapy decision – by a cardiac team including cardiac surgeons, cardiologists and, if necessary, experts from other specialties – taking into account the patient’s comorbidities is of crucial importance, especially in patients with more complex diseases.
Bypass surgery (CABG) was the only revascularization option for coronary artery disease (CAD) until Andreas Grüntzig performed the first percutaneous balloon dilatation (PCI) in 1977. However, in the early days of PCI, the complication rate from acute vascular occlusion and the risk for re-stenting were high, which prevented the use of PCI in complex CAD. With the introduction of stenting, the acute success of PCI was assured, and thus PCI rapidly gained acceptance as a therapy for acute myocardial infarction as well as one- and two-vessel disease. The development of drug-eluting stents (DES) also significantly reduced the high risk of in-stent restenosis when uncoated stents were used, and the spectrum of PCI use was expanded to include more complex lesions, multivessel disease, and the main stem. This resulted in a decrease in the number of surgical revascularizations and an increase in PCI.
Myocardial revascularization has been studied in a large number of randomized trials compared with most other medical interventions, with only smaller trials comparing surgical revascularization vs PCI with drug-eluting stents until 2009. Thus, the scientific evidence for the use of PCI in multivessel disease and/or main-stem stenosis was not available.
SYNTAX Study
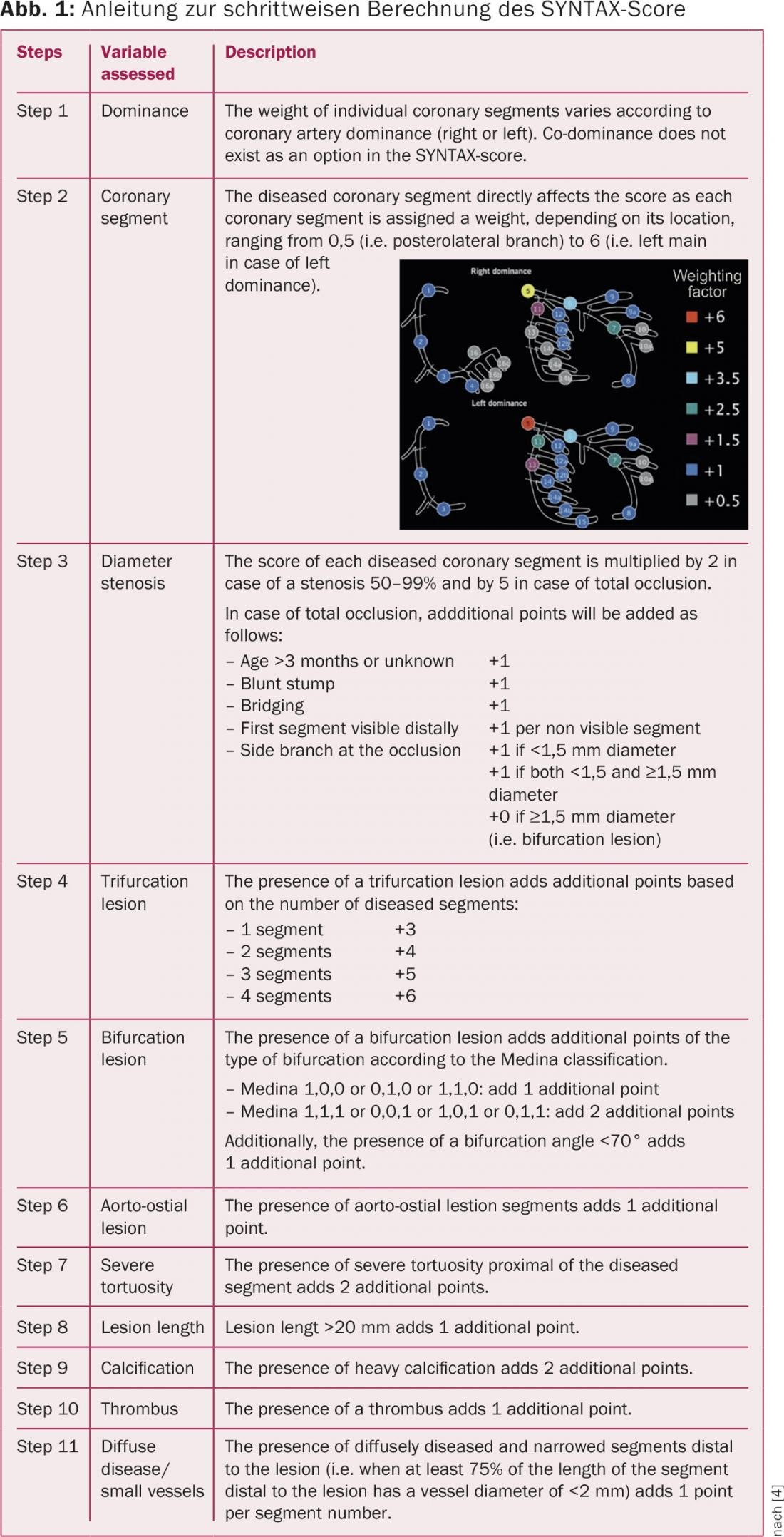
The SYNTAX (SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery) trial was designed to find the optimal treatment modality for patients with multivessel coronary artery disease and/or main stem stenosis [1]. The prospective randomized multicenter study included 1800 patients from 85 centers in Europe and the United States who had established coronary three-vessel disease and/or main stem stenosis. A significant novelty in the design of the SYNTAX trial compared with previous trials was that a team of an interventional cardiologist and a cardiac surgeon assessed patient eligibility for both forms of treatment. In addition, the complexity of coronary findings was quantified using the newly developed SYNTAX score (Fig. 1), which was used to divide the study population into groups with a low (<23), intermediate (23-32), or high (>32) score. Patients were randomized in a 1:1 ratio to an interventional procedure (PCI group) or to surgical myocardial revascularization (CABG group). PCI was performed with a first-generation DES, the paclitaxel-releasing Taxus stent. Furthermore, 1275 patients who were not suitable for PCI because of the complexity of the coronary findings were assigned to the CABG registry and inoperable patients with multiple comorbidities were assigned to the PCI registry and followed up in a prospective registry over the same period.
Results of the SYNTAX study
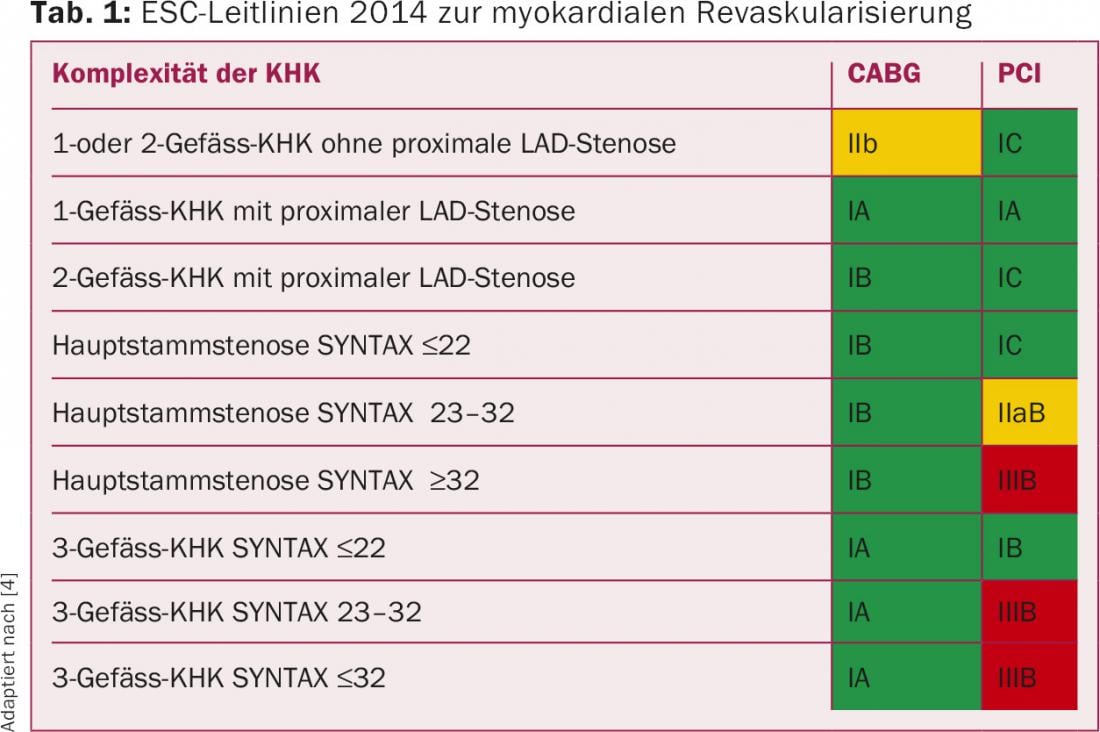
At one year, 12.4% of CABG and 17.8% of PCI patients met the primary combined endpoint (p=0.002), with no statistical difference in mortality (3.5% vs. 4.4%; p=0.37) or rate of myocardial infarction (4.8 vs. 3.3%). The key factor for the significant difference was the higher rate of repeat revascularization (5.9% vs. 13.5%; p=0.001), with a higher stroke rate in the operative arm (2.2% vs. 0.6%; p=0.003). It was found that the complexity of the CAD was crucial: in the low-risk group with simple multivessel coronary disease (SYNTAX score <22), PCI was equal to surgery, but the more complex the CAD, the more advantages surgery had. Treatment of main-stem stenosis by PCI now appeared evidence-based approachable for interventional cardiologists for the first time, as the combined end point was not significantly different between PCI and CABG (15.8% vs 13.7%). However, the 2010 European Society of Cardiology (ESC) guidelines did not yet incorporate the data of equivalence of PCI for less complex multivessel disease (SYNTAX score <22) and main stem stenosis (class IIb B recommendation for PCI vs. an IA for surgery) [2].
Five-year follow-up in the SYNTAX trial showed that the rate of major cardiac or cerebrovascular events (death, myocardial infarction, stroke, repeat revascularization) was significantly lower after cardiac surgery than after PCI in the overall population (26.9% vs. 37.3%). However, all-cause mortality was not significantly different (11.4% vs. 13.7%), and the slightly increased rate of stroke after bypass was also not significantly different after five years (3.7% vs. 2.4%).
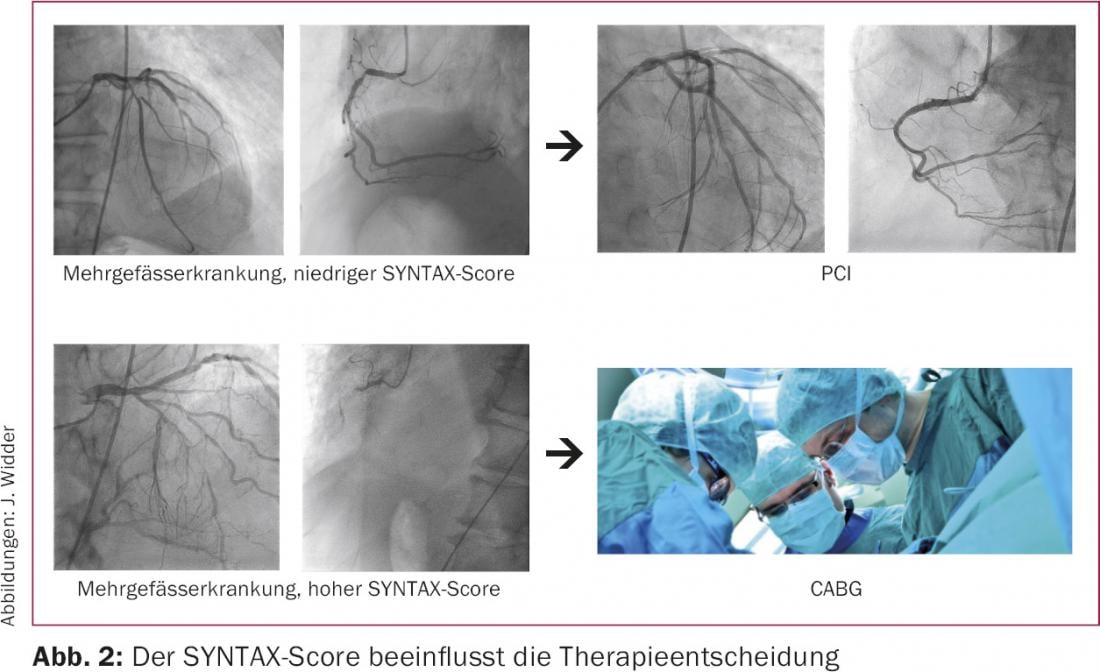
The 5-year data confirmed the equivalence of PCI and surgery even over the longer time course in the presence of low-complexity multivessel disease and/or main stem stenosis (SYNTAX score <23) [3]. In patients with intermediate SYNTAX score, the overall rate of cardiac and cerebrovascular events (25.8% vs. 36.0%), the rate of myocardial infarction (3.6% vs. 11.2%), and the rate of repeat revascularization (12.7% vs. 24.1%) each remained significantly lower after CABG than after PCI. The benefits of coronary surgery were particularly evident in the group of patients with high SYNTAX scores (combined end point: 26.8% vs. 44.0%; all-cause mortality: 11.4% vs. 19.2%; myocardial infarction: 3.9% vs. 10.1%, repeat revascularizing procedures: 12.1% vs. 30.9%). Thus, it has been demonstrated that there is a survival advantage with coronary surgery compared with PCI in complex CHD. However, simple main stem stenosis and less complex multivessel disease are clearly no longer the sole domain of surgical care; this was reflected in the new ESC guidelines published in 2014 and was also incorporated into the National CHD Care Guidelines (Table 1, Fig. 2) [4,5].
Comparative studies according to SYNTAX
The first-generation paclitaxel-eluting Taxus stent used in the SYNTAX trial has now given way to more modern stents with thinner struts and biocompatible polymers. These have a significantly lower risk of stent thrombosis as well as re-stenting. Doesn’t this already render the SYNTAX data invalid? The randomized BEST trial published this year compared PCI with everolimus-eluting second-generation DES against surgery in 880 patients [6]. Regarding the primary end point of death, myocardial infarction, or repeat revascularization, the data (PCI 17% vs. CABG 11.7%) seem to clearly confirm the SYNTAX trial. Diabetic patients benefited more clearly from surgery, as in the Freedom trial [7], and again CABG was shown to benefit in more complex multivessel disease; however, PCI was again equivalent in low SYNTAX score. It must be taken into account that, as in SYNTAX, only the higher revascularization rate was decisive for the significant difference of the primary end point. Bypass surgery did not show fewer myocardial infarctions or a survival benefit compared with PCI.
In the same issue of the New England Journal of Medicine, a retrospective analysis of registry data was published that retrospectively compared outcomes for 9223 PCI with an everolimus-eluting stent versus 9332 operated patients [8]. Here, there was again no mortality difference; again, the repeat revascularization rate was lower but the stroke rate was higher after CABG. The incidence of myocardial infarction was the same when complete revascularization was achieved in both groups but higher in the PCI group when complete revascularization was not possible. This, like the data from the SYNTAX trial, indicates the importance of complete revascularization [9].
The recently published 5-year data of the PRECOMBAT trial (600 patients 1:1 sirolimus stent vs. CABG) confirmed the feasibility of PCI in main stem stenosis, although the power is limited due to the underpowered nature of the trial [10]. The ongoing Excel study (Everolimus-eluting DES vs CABG in main stem stenosis with SYNTAX score <32) will provide further evidence in this regard.
Thus, with modern second-generation DES, there now appears to be no mortality advantage in favor of bypass surgery, at least for less complex multivessel disease and main stem stenoses, even in the long-term course.
Concomitant diseases
Patients in the SYNTAX trial and in the Best trial were still relatively young (about 65 years) and well operable. However, more and more of our patients are of advanced age and often have multiple comorbidities, so that the extent to which surgical treatment offers advantages must be carefully weighed up. The SYNTAX-II score attempts to weight this as it takes into account not only coronary anatomy but also age, pAVK, gender, and COPD, which influence outcome after CABG and PCI [11]. Risk assessments are helpful, but they also have their limitations. Therefore, individualized decision-making by a cardiac team including cardiologists, cardiac surgeons, and other subject matter experts as appropriate is essential in more complex patients. The cardiac team is also clearly called upon in the guidelines to make treatment decisions in complex cases.
Summary
Since the introduction of percutaneous balloon dilatation (PCI), the question for patients with coronary artery disease (CAD) has been: PCI or bypass grafting (CABG)? Rapid advances in the technical capabilities of PCI and drug-eluting stents (DES) led to the expansion of PCI use, but without hard scientific evidence in stable CHD. Through the SYNTAX trial with first-generation Taxus DES, PCI became evidence-based even in multivessel disease and low-complexity main stem stenosis and has been guideline-eligible since 2014. However, in more complex cases and especially in diabetic patients, PCI is inferior to CABG.
More modern DES have a significantly lower risk of complications (especially stent thrombosis). However, recently published comparative studies and registry data with second-generation DES continued to confirm a higher rate of reintervention after PCI, although not as clearly as in the past. On the other hand, a clear survival advantage for CABG no longer seems clearly present. Thus, PCI approaches the results of CABG in cases of multivessel disease and/or main stem stenosis; however, PCI still does not achieve the results of CABG, especially in cases of complex stenosis morphology.
Considering that a large proportion of CHD patients are not represented in studies due to older age and concomitant diseases, the need for an individual therapy decision made jointly by the heart team is obvious for these patients.
Literature:
- Serruys PW, et al: Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360(10): 961-972.
- Wijns W, et al: Guidelines on myocardial revascularization. Eur Heart J 2010; 31(20): 2501-2555.
- Mohr FW, et al: Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013; 381(9867): 629-638.
- Windecker S, et al: 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2014; 35(37): 2541-2619.
- German Medical Association (BÄK), K.V.K., Association of the Scientific Medical Societies (AMWF): Nationale Versorgungsleitlinie Chronische KHK – Langfassung 3. Auflage Version 1, www.khk.versorgungs leitlinien.de, 2014. DOI: 10.6101/AZQ/000217.
- Park SJ, et al: Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med 2015; 372(13): 1204-1212.
- Farkouh ME, et al: Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012; 367(25): 2375-2384.
- Bangalore S, et al: Everolimus-eluting stents or bypass surgery for multivessel coronary disease. N Engl J Med 2015; 372(13): 1213-1222.
- Farooq V, et al: Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation 2013; 128(2): 141-151.
- Ahn JM, et al: Randomized Trial of Stents Versus Bypass Surgery for Left Main Coronary Artery Disease: 5-Year Outcomes of the PRECOMBAT Study. J Am Coll Cardiol 2015; 65(20): 2198-2206.
- Farooq V, et al: Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet 2013; 381(9867): 639-650.
CARDIOVASC 2015; 14(6): 4-8