Patients with kidney stones should be divided into low and high risk groups in terms of recurrence rate. Basic clarification and stone analysis serve as a basis. High-risk patients should receive extended metabolic evaluation and specific treatment.
Kidney stones occur frequently and may be associated with significant morbidity [1]. Repeat urologic stone removal does not reduce the high recurrence rate. However, the number of recurrences can be reduced with conservative measures [2]. Therefore, an assessment of the risk of recurrence and, if the risk is significant, appropriate recurrence prophylaxis (metaphylaxis) is necessary. A distinction must be made between low-risk and high-risk patients. The underlying clarification steps in our center are essentially based on the guidelines of the European Association of Urology (EAU) [3]. With knowledge of stone composition and a basic workup, patients can usually be assigned to one of the two risk categories. The subsequent metaphylaxis consists of nutritional measures on the one hand, but may also include drug treatment. With this article, we would like to convey to the primary care provider the essential aspects that need to be considered.
Epidemiology and recurrence rates
Kidney stone disease is highly prevalent in the Western world and beyond, with a marked increase in incidence rates [1,4]. Recurrence rates are generally high but vary widely. Within ten years after the first episode, recurrence occurs in nearly 30% of patients with a calcium oxalate stone, while this is as high as 70% for brushite stones (calcium hydrogen phosphate). However, some patients experience only one stone event in their lifetime. After a recurrence, the risk for further events increases significantly. In untreated cystinuria, the risk of recurrence is as high as 85%, and high recurrence rates are also assumed for uric acid and infectious stones [5].
Risk classification: stone analysis and basic clarification
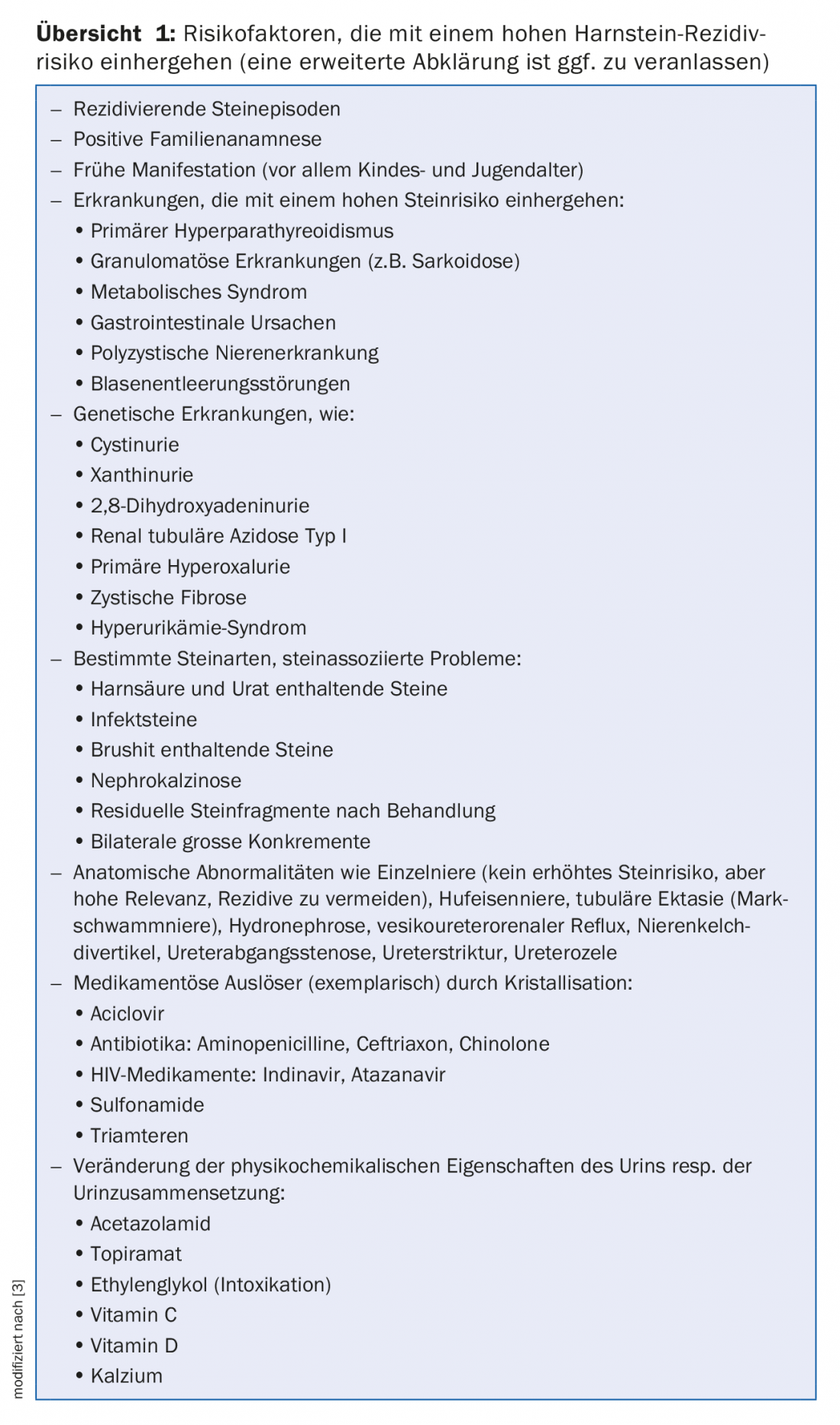
In most cases, stone analysis and a simple baseline workup allow patients to be classified into a low- or high-risk group with regard to the likelihood of recurrence. Despite the generally high risk of recurrence, there is considerable variation in this regard, and not every patient requires extended metabolic workup with a specialist or specific treatment. For many patients, general metaphylaxis measures are sufficient. Therefore, patients with a particularly high risk of recurrence and those requiring specific therapy should be filtered out during the initial workup. Risk factors leading to assignment to the high-risk group are listed in Overview 1. Stone composition and severity of the disease are essential.
Stone analysis
If available, an assayed kidney stone should be analyzed for its exact composition. This valuable information can indicate etiology and significantly influences risk classification and metaphylaxis recommendations. Patients are therefore advised to urinate through a sieve during colic to collect outgoing concretions. Concrements recovered by the urologist should also be examined in the laboratory. Occasionally, patients have kept stones from previous episodes at home. These can also be sent in for analysis at a later date without any problems. X-ray diffraction and infrared spectrometry serve as the analytical methods of choice. Wet chemistry studies, on the other hand, are obsolete [6].
If no concrement is available for analysis, microscopic examination of the urine sediment may provide information on the stone composition. Certain crystals, such as cystine crystals, exhibit a characteristic morphology. Therefore, in cystinuria, for example, the sediment can be diagnostic (Fig. 1). In addition, the behavior in relation to X-rays can provide indirect indications of the stone composition and serve for classification. While calcium-containing stones (calcium oxalate and phosphate stones) are radiopaque, uric acid stones, for example, are permeable to X-rays. For larger calculi, computed tomographic density measurement or special procedures may provide clues to stone type [7–9]. It is important to note that urine sediment and imaging do not usually replace direct stone analysis. If this is not present, the assessment of the risk of recurrence is limited to whether other risk factors are present.

Kidney stones may consist of one or more components. Calcium oxalate is by far the most common component, both in mixed stones and alone. Calcium phosphate, uric acid, and struvite are the next most common components, while cystine and others are less common [10,11].
Kidney stones can be classified based on etiology in addition to chemical composition. Certain types of stones are associated with infections of the kidneys or urinary tract (magnesium ammonium phosphate, carbonate apatite, ammonium urate stones), so-called infectious stones. Other stones (e.g. calcium oxalate, calcium hydrogen phosphate, uric acid stones) occur independently. That is why they are called “non-infectious stones”. Stones that clearly have a genetic cause (e.g. cystine, xanthine, 2,8-dihydroxyadenine stones) should be distinguished. The earlier the onset, with a positive family history, and the more severe the phenotype, the more likely genetic causes should be considered, requiring differential workup and treatment. Drugs may also be lithogenic (crystallizing directly or by altering urine composition).
Basic clarification
History, clinical examination, and imaging: With a thorough history, many of the risk factors listed in Overview 1 can be obtained. Particular attention should be paid to previous stone events, age at initial manifestation, colic that has occurred, and urologic surgery. Urinary tract infections and pyelonephritis, gastrointestinal complaints (such as chronic diarrhea, pancreatitis, gastric ulcers), and gouty conditions must be specifically inquired about. In addition to family and medication history (including alternative medical substances, vitamin supplements), lifestyle, dietary habits, and previous surgery (especially bariatric or other abdominal surgery) should be clarified.
Imaging is usually performed for an acute urinary stone episode or for follow-up/stone balancing. The two most important methods are ultrasound and so-called “low-dose” spiral computed tomography. In addition to information with an impact on urologic stone management, such as calculus size, location, and stone load, anatomic abnormalities can also be found and diagnosed. After urologic treatment, imaging is used to determine the absence of stones or the presence of residual calculi and to monitor progress. Considerations such as radiation exposure, examiner expertise, sensitivity, specificity, availability, and cost all play a role in method selection. In acute diagnostics, sonography (with less radiation exposure) still has a place [12].
- Laboratory: The basic workup should include the following determinations in laboratory testing and should be performed in all kidney stone patients:
- Urine: urine test strips with leukocytes, hemoglobin, nitrite, pH; if necessary, urine culture if there are indications of infection; microscopic urine sediment
- Blood: creatinine, calcium (ionized or albumin-corrected), uric acid
Extended metabolic workup in high-risk patients
Patients in the high-risk group (overview 1) are recommended to have an extended metabolic workup with a specialist. Here, the focus is on a 24h urine collection (ideally on two consecutive days) under everyday diet, under which the stones were also formed. This should therefore not be done in hospital and also no earlier than three to four weeks after stone removal or urological treatment [13]. Urine volume and pH, creatinine, sodium and urea are determined, among others. Creatinine clearance can be calculated via creatinine determination and the completeness of the collection can be estimated. The excretion of the examined substances is set in relation to creatinine and thus corrected. The sodium determination is used to estimate the daily consumption of table salt, and the urea determination is used to estimate the daily protein intake. In young children, urine collection is omitted and spot urine analyses are performed.
The following additional laboratory values are usually determined from the urine: Calcium, oxalate, citrate, phosphate, uric acid and possibly magnesium, potassium and cystine.
Table 1 gives an overview of the relevant parameters depending on the stone type. In addition to the parameters of the basic clarification, the determination of bicarbonate, parathormone and 25-OH-vitamin D3 from the blood has proven to be useful. This allows diagnosis of causes such as primary hyperparathyroidism, renal tubular acidosis (along with urine pH), or hypervitaminosis D3.

As a rule, after three months, especially if drug metaphylaxis has been started, a 24h urine follow-up is performed. Further follow-up examinations are determined depending on the risk constellation.
Treatment
General measures are generally recommended for all patients with kidney stone disease. All stone formers should maintain a high drinking rate [2,14]. The goal is a urine volume of more than 2-2.5 liters/day to prevent oversaturation of urine with substances that cause stones. The urine should always be light yellow in color and the specific gravity should be less than 1.010 g/ml. This usually requires a drinking quantity of at least 2.5-3 liters/day, and correspondingly more in the case of physical activity with sweating. Drinking should also be done before going to bed so that nocturia occurs and nocturnal urinary oversaturation is also avoided. Not all drinks are equally suitable for metaphylaxis. There is epidemiologic evidence of increased stone risk associated with sweetened beverages (possibly due to increased fructose content) [1,15]. For certain occupational groups, such as bus drivers, it is not easy to implement high levels of drinking with frequent trips to the toilet. Here, strategies are to be worked out together with the patient.
A balanced mixed diet is generally recommended [1]. Numerous studies have shown risk reduction by reduced salt consumption (high sodium intake and consecutive natriuresis lead to increased urinary calcium and decreased urinary citrate excretion) [1]. The current WHO recommendation includes a salt intake below 5 g/day for adults. This is also recommended for stone patients. As an alternative to table salt, patients can use herbs and spices to prepare their meals. The previously prevailing opinion that stones can be prevented by reduced calcium consumption has turned out to be a misconception. A study by Borghi et al. showed that a diet with salt and protein restriction but normal calcium intake resulted in a significant reduction in the risk of recurrence after five years compared to a low calcium diet [16]. Other observational studies also suggest an association between low calcium consumption and increased stone risk [1,17]. A recommendation for a normal calcium consumption of 1-1.2 g/day is derived from this. Calcium intake should be covered by natural sources. Calcium supplements are usually recommended only for enteric hyperoxaluria. 250 mg of calcium is equivalent to, for example, 2 dl of whole milk, 180 g of yogurt, 30 g of hard cheese, 50 g of soft cheese, or 250 g of cottage cheese. Recommendations regarding the benefit of reducing oxalate intake are so far without clear evidence, although this seems reasonable when hyperoxaluria is detected [1]. It is probably more important to decrease enteral oxalate intake. This can be achieved by a simultaneous calcium intake, e.g. in the form of cheese or calcium-rich mineral water (>400 mg/l). Calcium complexes oxalate in the intestine to calcium oxalate, which in this compound cannot be absorbed into the blood [18].
Proteins, especially animal proteins, lead to an increased acid load. This causes a reduction in citraturia and an acidic urine pH. Citrate and calcium in urine complex, making calcium unavailable for stone formation. Hypocitraturia therefore favors calcium stone formation [19]. Therefore, a moderate consumption of animal proteins of 0.8-1 g/day/kg bw is recommended. A diet high in fiber, fruits, and vegetables is generally recommended (high citrate, high urine pH) [20]. It makes sense to distribute the citrate intake throughout the day. Purine-rich foods (hyperuricosuria), e.g. offal, should be avoided, especially in the case of uric acid stone formers.
Since there is a positive association between BMI and stone risk, it is recommended to aim for a normal BMI . Observational studies also suggest that regular moderate physical activity is associated with a lower risk of stones.
Stone-specific features and treatment options
Calcium stones (calcium oxalate and phosphate): Certain conditions such as hyperparathyroidism, renal tubular acidosis, granulomatous disease, primary hyperoxaluria (genetic condition requiring specialized care), and enteric hyperoxaluria are associated with calcium stones and require clarification or specific treatment. Therapy measures are:
- Reduced salt intake
- Reduced intake of animal (non-dairy) proteins
- Normal calcium intake
- No oxalate excesses (food and beverages)
- High citrate intake: dietary or as potassium citrate. Administration of potassium citrate may reduce the risk of idiopathic calcium oxalate stones in both hypocitraturia and normal citraturia [1,2]. Side effects such as nausea, meteorism, and diarrhea are unfortunately common, especially at high doses, and decrease adherence. Alternatively, if urinary alkalinization is the primary concern, sodium bicarbonate may be used [21]. It should be noted that alkalinization of urine pH with sodium bicarbonate could increase the risk of calcium phosphate stones [21,22].
- Thiazide diuretics: A large number of studies have shown a significant reduction in the recurrence rate with thiazide diuretics. A halving of the recurrence rate has been described [2]. An essential role is played by increased proximal tubular calcium absorption and a consecutive decrease in calcium excretion [1]. Side effects include hypotension, hyponatremia and -kalemia, and hyperuricemia. Currently, a study is being conducted in almost all major nephrology clinics throughout Switzerland to address the methodological deficits of older studies and to test the efficacy of hydrochlorothiazide as a function of dosage (www.nostone.ch). Older studies primarily used high doses of thiazide, whereas much lower doses are usually used in clinical practice. The results of this study are expected in 2022.
- Allopurinol is beneficial in hyperuricosuric calcium stone patients [23]. High-dose febuxostat reduced uricosuria more than normal-dose allopurinol, but failed to show a benefit in terms of stone formation in six months of study [24]. However, the role of hyperuricosuria in calcium stone patients has not been conclusively determined. According to in vitro data, hyperuricosuria may decrease calcium oxalate solubility, but epidemiological data are conflicting [1].
Special form of enteric hyperoxaluria as a cause of calcium oxalate stones: Various conditions/diseases such as bariatric surgery (especially malabsorptive surgery such as gastric bypass), short bowel syndrome, exocrine pancreatic insufficiency, celiac disease as well as Crohn’s disease can lead to enteric hyperoxaluria. Pathophysiologically, saponification of unabsorbed fatty acids with calcium in the intestine plays an essential role. Calcium is then no longer available for intestinal binding of oxalate, which subsequently leads to increased oxalate uptake into the blood and marked hyperoxaluria [25]. Reduction of oxalate and fat consumption seems reasonable because of the pathomechanism. These patients need to increase calcium consumption in conjunction with meals to several grams daily. Most phosphate binders also bind oxalate in the intestinal lumen and can be used [7]. Enteric bicarbonate losses in diarrhea additionally provide an increase in reabsorption of citrate through intracellular acidosis of renal tubule cells, resulting in unfavorable hypocitraturia [26]. For this reason, an additional treatment with alkali citrate is often useful. Furthermore, pancreatic enzymes may be used if indicated. Substances that complex with bile acid, if indicated, can also reduce the absorption of oxalate. Colestyramine or colestipol also bind oxalate [7]. In our experience, patients are often inadequately informed about this risk prior to bariatric surgery.
Essentially, calcium phosphate stones are treated like calcium oxalate stones [1]. Calcium phosphate occurs in brushite rocks (calcium hydrogen phosphate) and carbonate apatite rocks. Both are formed preferentially in alkaline urine. Reasons for calcium phosphate stones may include renal tubular acidosis (complete or incomplete) or hyperparathyroidism. These causes should be clarified and treated if possible. Carbonate apatite stones are typically associated with urinary tract infections.
Uric acid stones: Uric acid stones are associated with low urine pH, low drinking volume, and hyperuricosuria [1,27]. There is an association with metabolic syndrome and the prevalence is increased in obese and type 2 diabetics [27]. Therapy measures are:
- Urinary alkalinization with alkali citrate or sodium bicarbonate to achieve a urine pH of 6.2-6.8 for prevention or 6.5-7.2 for chemolitholysis [3].
- Moderate consumption of animal proteins to reduce acid load.
- Reduction of foods containing purine
- Weight reduction
- Allopurinol in hyperuricosuria and hyperuricemia [3].
- Limited benefit of allopurinol and febuxostat in acid urine [7,28].
Infectious stones: Struvite (magnesium ammonium phosphate or triple phosphate), carbonate apatite and ammonium urate stones are usually associated with urinary tract infections caused by urease-producing bacteria in alkaline urine and can rapidly increase in size. Stone treatment is often very difficult.
- Antibiotic treatment alone (short-term or permanent) is not sufficient for infectious stones.
- A complete urological stone rehabilitation should be aimed for (stone free).
- Occasionally, acidification of the urine, e.g. with methionine or ammonium chloride, is also used to dissolve the calculus [3]. Therapy should be limited in time and under close monitoring for metabolic acidosis, hypercalciuria, and hypocitraturia.
- Urease inhibitors (e.g., acetohydroxamic acid) may be considered in severe cases, although these have not yet been approved in some European countries [3] and Switzerland.
Cystine stones: Cystinuria is an important genetic cause of kidney stone disease (autosomal recessive inheritance). Due to a defective tubular transport protein, high concentrations of cystine occur in the urine. Therapy measures are:
- Urine volume of >3 l/day in adulthood
- Salt reduction
- Urine pH should be adjusted to >7.5 (increased solubility of cystine), e.g., with potassium citrate or sodium bicarbonate [3].
- Moderate consumption of animal proteins (reduces acid load and methionine intake)
- Penicillamine can be used to chelate cystine in cystinuria greater than 3 mmol/day with close monitoring of therapy. The goal is cystinuria <1 mmol/l [7].
- The use of captopril, an ACE inhibitor, should be considered in hypertensive patients because it binds cystine and the compound is many times more soluble than cystine alone [29]. However, the benefit has not yet been clearly proven.
To reduce the recurrence rate and associated morbidity of kidney stones, possible causes must be clarified and general and, if necessary, specific metaphylaxis measures must be taken. Optimal treatment requires good interdisciplinary interaction between the attending primary care physician, emergency medicine physician, urologist, and nephrologist.
Take-Home Messages
- Kidney stones have a high recurrence rate that is not reduced by urologic stone removal alone.
- Metaphylaxis measures can reduce the recurrence rate.
- Patients are to be divided into a low-risk and high-risk group with regard to recurrence rate, based on the baseline workup and stone analysis.
- While general metaphylaxis measures are recommended for patients in the low-risk group in light of the type of stone, patients in the high-risk group should undergo an extended metabolic workup and, if possible, specific treatment.
Literature:
- Zisman AL: Effectiveness of Treatment Modalities on Kidney Stone Recurrence. Clin J Am Soc Nephrol 2017; 12(10): 1699-1708.
- Fink HA, et al: Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann Intern Med 2013; 158(7): 535-543.
- Turk C, et al: EAU Guidelines on Urolithiasis. https://uroweb.org/guideline/urolithiasis/2017 (Mar 01, 2018).
- Romero V, Akpinar H, Assimos DG: Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol 2010; 12(2-3): e86-96.
- Tiselius HG: Metabolic risk-evaluation and prevention of recurrence in stone disease: does it make sense? Urolithiasis 2016; 44(1): 91-100.
- Siener R, et al: Quality Assessment of Urinary Stone Analysis: Results of a Multicenter Study of Laboratories in Europe. PLoS One 2016; 11(6): e0156606.
- Mabillard HR, Tomson CRV: Investigation and management of renal stone disease. Nephrol Dial Transplant 2017; 32(12): 1984-1986.
- Stolzmann P, et al: In vivo identification of uric acid stones with dual-energy CT: diagnostic performance evaluation in patients. Abdom Imaging 2010; 35(5): 629-635.
- Stolzmann P, et al: Characterization of urinary stones with dual-energy CT: improved differentiation using a tin filter. Invest Radiol 2010; 45(1): 1-6.
- Ferraro PM, et al: A London experience 1995-2012: demographic, dietary and biochemical characteristics of a large adult cohort of patients with renal stone disease. QJM 2015; 108(7): 561-568.
- Seeger H, et al: Changes in urinary risk profile after short-term low sodium and low calcium diet in recurrent Swiss kidney stone formers. BMC nephrology 2017; 18(1): 349.
- Smith-Bindman R, et al: Ultrasonography versus computed tomography for suspected nephrolithiasis. N Engl J Med 2014; 371(12): 1100-1110.
- Gambaro G, et al: Metabolic diagnosis and medical prevention of calcium nephrolithiasis and its systemic manifestations: a consensus statement. J Nephrol 2016; 29(6): 715-734.
- Borghi L, et al: Urinary volume, water and recurrences in idiopathic calcium nephrolithiasis: a 5-year randomized prospective study. J Urol 1996; 155(3): 839-843.
- Ferraro PM, et al: Soda and other beverages and the risk of kidney stones. Clin J Am Soc Nephrol 2013; 8(8): 1389-1395.
- Borghi L, et al: Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. N Engl J Med 2002; 346(2): 77-84.
- Curhan GC, et al: A prospective study of dietary calcium and other nutrients and the risk of symptomatic kidney stones. N Engl J Med 1993; 328(12): 833-838.
- Hess B, et al: High-calcium intake abolishes hyperoxaluria and reduces urinary crystallization during a 20-fold normal oxalate load in humans. Nephrol Dial Transplant 1998; 13(9): 2241-2247.
- Ferraro PM, et al: Dietary protein and potassium, Diet-Dependent Net Acid Load, and Risk of Incident Kidney Stones. Clin J Am Soc Nephrol 2016; 11(10): 1834-1844.
- Taylor EN, Fung TT, Curhan GC: DASH-style diet associates with reduced risk for kidney stones. J Am Soc Nephrol 2009; 20(10): 2253-2259.
- Pinheiro VB, et al: The effect of sodium bicarbonate upon urinary citrate excretion in calcium stone formers. Urology 2013; 82(1): 33-37.
- Parks JH, et al: Clinical implications of abundant calcium phosphate in routinely analyzed kidney stones. Kidney Int 2004; 66(2): 777-785.
- Ettinger B, et al: Randomized trial of allopurinol in the prevention of calcium oxalate calculi. N Engl J Med 1986; 315(22): 1386-1389.
- Goldfarb DS, et al: Randomized controlled trial of febuxostat versus allopurinol or placebo in individuals with higher urinary uric acid excretion and calcium stones. Clin J Am Soc Nephrol 2013; 8(11): 1960-1967.
- Asplin JR: The management of patients with enteric hyperoxaluria. Urolithiasis 2016; 44(1): 33-43.
- Hess B: Metabolic syndrome, obesity and kidney stones. Arab J Urol 2012; 10(3): 258-264.
- Sakhaee K: Epidemiology and clinical pathophysiology of uric acid kidney stones. J Nephrol 2014; 27(3): 241-245.
- Asplin JR: Uric acid stones. Semin Nephrol 1996; 16(5): 412-424.
- Sloand JA, Izzo JL: Captopril reduces urinary cystine excretion in cystinuria. Arch Intern Med 1987; 147(8): 1409-1412.
HAUSARZT PRAXIS 2018; 13(4): 26-31











