Worldwide, about half of the adult population suffers from vitamin D deficiency (<50 nmol/l). This increases the risk of bone fractures and falls. At this year’s EULAR Congress in Madrid, several studies were presented that point to a possible role for vitamin D in risk reduction of rheumatoid arthritis and osteoarthritis.
At the beginning of her presentation at this year’s EULAR Congress in Madrid, Prof. Heike Bischoff-Ferrari, MD, Chair of Geriatrics and Aging Research at the University of Zurich, gave an overview of the epidemiology of vitamin D deficiency. Studies show that approximately half of the adult population worldwide has a blood 25-hydroxyvitamin D level of <50 nmol/l [1]. Such a deficiency supply entails risks. For persons over 60 years of age, falling below the daily intake of 800 IU places them at increased risk for hip and other non-vertebral fractures. “Specifically, a daily intake of 800 IU has been shown to reduce the risk of hip fracture by 30% and non-vertebral fracture by 14% in seniors [2],” said Prof. Bischoff-Ferrari. “The same is true for falls. With 800 IU of vitamin D per day, one in three falls can be prevented [3].”
Vitamin with hormone character
Vitamin D performs endocrine and paracrine functions. It acts via a highly specific intracellular receptor (VDR) present, for example, in T and B cells, macrophages, but also muscle cells, cardiovascular, brain and cartilage cells. Thus, vitamin D has hormonal character and has functions that go far beyond the regulation of calcium metabolism. The skin is the main source of absorption: The human body produces vitamin D via UVB radiation. Food contributes only a small share to the supply, since considerable amounts are essentially limited to fatty fish.
Vitamin D and Rheumatoid Arthritis
“In the case of rheumatoid arthritis (RA), vitamin D has interesting potential mainly because of its anti-inflammatory and muscle-strengthening effects, as well as its VDR-mediated role in cartilage maturation,” Prof. Bischoff-Ferrari explained. “Vitamin D deficiency is very common in RA patients.” RA increases the risk of hip and vertebral fractures twofold [4], as well as falls, because RA is associated with joint pain and loss of strength. Moreover, the inflammatory activity leads to local but also general bone loss.
The relationship between RA and vitamin D has been investigated by several studies. The Iowa Women’s Health Study demonstrated that supplemental vitamin D intake of 400 IU/day was associated with a 34% reduction in the risk of RA [5]. In the Norfolk Arthritis Registry, an inverse relationship was found between 25(OH)D level and “tender joint count” (index of the number of painful joints) [6]. As early as 1998, Larsson et al. in mice with collagen-induced RA show that prior treatment with a vitamin D analogue prevented RA in 50% of cases, and in those animals that did develop the disease, symptoms were milder [7]. In contrast to the results of the Iowa Women’s Health Study, the Women’s Health Initiative study was the only intervention study to demonstrate no significant effects of vitamin D administration (400 IU/day) on the incidence of RA in 36 282 postmenopausal women [8]. However, it was discussed that the dosage of 400 IU vitamin D per day was too small in this study.
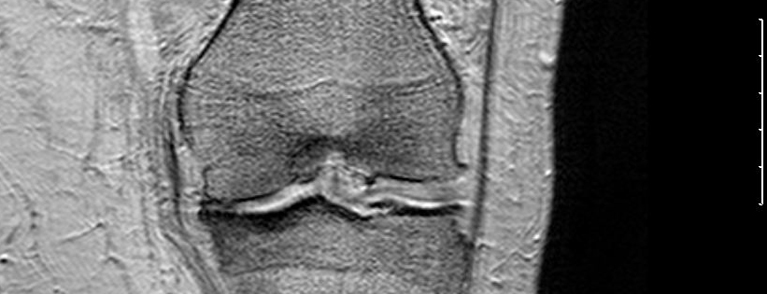
Vitamin D and osteoarthritis
“Vitamin D deficiency is also prevalent in osteoarthritis patients. In 2005, we were also able to show in the Framingham study that in knee osteoarthritis patients, higher 25(OH)D levels correlate with higher bone mineral density (“BMD”) [9],” said Prof. Bischoff-Ferrari. “Osteoarthritis leads to muscle weakness, increased falls, and increases the risk of hip fracture twofold compared to the normal population. Thus, it makes sense to address vitamin D deficiency in osteoarthritis patients. To this end, large observational studies show that individuals with higher 25(OH)D levels or vitamin D intake have a lower risk of progression to existing hip and knee osteoarthritis [10, 11], yet studies also exist that postulate no association [12].”
In summary, Prof. Bischoff-Ferrari points to the increased risk of falls and fractures in patients with RA and osteoarthritis, which should be considered an important basic rationale for general vitamin D supplementation in practice. Whether vitamin D also has a disease-modulating effect in these patients has not yet been established. However, there is mechanistic evidence from basic science work that may explain a protective effect of vitamin D on disease progression in RA and osteoarthritis observed in large cohort studies via a direct effect of vitamin D on cartilage and immune cells. Evidence from large clinical intervention trial with sufficiently high vitamin D dose is pending. The EU study “Intervention Study DO-HEALTH” has been running since 2012 and will be evaluated in 2017 (http://do-health.eu/wordpress/).
Source: “D-hormone and inflammation – clinical aspects”, EULAR, June 12-15, 2013, Madrid.
Literature:
- Van Schoor NM, Lips P: Best Pract Res Clin Endocrinol Metab 2011 Aug; 25(4): 671-680. doi: 10.1016/j.beem. 2011.06.007.
- Bischoff-Ferrari HA, et al: N Engl J Med 2012; 367: 40-49. doi: 10.1056/NEJMoa1109617.
- Bischoff-Ferrari HA, et al: BMJ 2009; 339. doi: http://dx.doi.org/10.1136/bmj.b3692.
- Kröger H, et al: Scand J Rheumatol 1993; 22(4): 172-177.
- Merlino LA, et al. (Iowa Women’s Health Study): Arthritis Rheum 2004 Jan; 50(1): 72-77.
- Patel S, et al: Arthritis Rheum 2007 Jul; 56(7): 2143-2149.
- Larsson P, et al: Clin Exp Immunol 1998 Nov; 114(2): 277-283.
- Racovan M, et al: Rheumatol Int 2012 Dec; 32(12): 3823-3830. doi: 10.1007/s00296-011-2268-1. epub 2011 Dec 22.
- Bischoff-Ferrari HA, et al: Arthritis Rheum 2005 Dec 15; 53(6): 821-826.
- McAlindon TE, et al: Ann Intern Med 1996 Sep 1; 125(5): 353-359.
- Lane NE, et al: Arthritis Rheum 1999 May; 42(5): 854-860.
- Konstari S, et al: Scand J Rheumatol. 2012 Mar; 41(2): 124-131.