Switzerland occupies an inglorious top position in Europe with regard to the incidence of syphilis. The following article shows which venereal diseases can be treated well and what the importance of the sexual anamnesis is all about.
Sexually transmitted infections (STIs) are a significant medical and public health problem. They disproportionately affect people with high-risk contacts (especially men who have sex with men [MSM] ), women, and marginalized people, which is why STIs have been a focus of European health policy for years. In Switzerland, too, there has been an increase in STI for years, which has been observed for ten years for syphilis, for example, and has been continuing for gonorrhea since 1996.
Importance of the STI
More than 30 sexually transmitted pathogens are known worldwide, which include bacteria, viruses, fungi, protozoa and ectoparasites (Table 1). Twelve pathogens have been newly discovered since 1975 alone, including, for example, the various mycoplasmas – especially Mycoplasma genitalium -, the human herpes virus type 8, the hepatitis C virus, bacteria such as Mobiluncus and, as the most important pathogen, HIV. The fact that in 20-50% of patients with urethritis the responsible pathogen cannot be determined [1, 2] supports the possibility that certain germs are either not yet known or their significance has not yet been appreciated. Recently, papers have been published emphasizing, for example, the importance of viruses from the herpes group such as Epstein-Barr or herpes simplex [3] or even adenoviruses [4] as causative agents of urethritis. Infections are most frequently transmitted sexually with human papillomaviruses (HPV), herpes viruses, chlamydia and gonococci, while infections with hepatitis B, HIV or syphilis are comparatively less common. According to estimates by the World Health Organization (WHO, 2005), 448 million (curable) STIs (syphilis, gonorrhea, chlamydial infection, and trichomoniasis) occur in 15- to 49-year-olds worldwide each year. With adequate diagnosis and therapy, these diseases are curable with effective antibiotics, with the limitation of the daunting resistance problem in gonorrhea [5].
However, inadequate diagnosis and treatment can have serious consequences for affected individuals, as well as for pregnancies and newborns. Untreated early syphilis during pregnancy leads to transmission to the newborn in over 60% of cases, resulting in death in over one-third and, in some cases, pronounced, stigmatizing changes. Lues connata must again be expected in Switzerland, which is why the comparatively inexpensive screening should be performed during pregnancy [6]. In the newborn, severe long-term neurological sequelae or death may also result from herpes simplex infection (herpes neonatorum). In women, the most important complications are ascending infection, extrauterine pregnancy, and infertility, especially in the case of chlamydial infection. In addition, STIs (HPV, hepatitis B) are important co-factors in the development of malignancies. For all STDs – and to a greater extent for the ulcerative forms(Fig. 1) – it is additionally significant that they are associated with an increased risk of acquisition and transmission of HIV [7].
After a clearly decreasing incidence of classical STI could be documented in Western Europe at the beginning of the 1990s, trends since 1995 show an increased occurrence again, which could be confirmed with a delay also in Switzerland by the available surveillance data [8, 9]. According to the FOPH (mandatory laboratory reporting of infections with Chlamydia trachomatis, Neisseria gonorrhoeae, Treponema pallidum, and hepatitis A, B, C and HIV), an unbroken trend in classical STIs is also expected for 2013 [10].
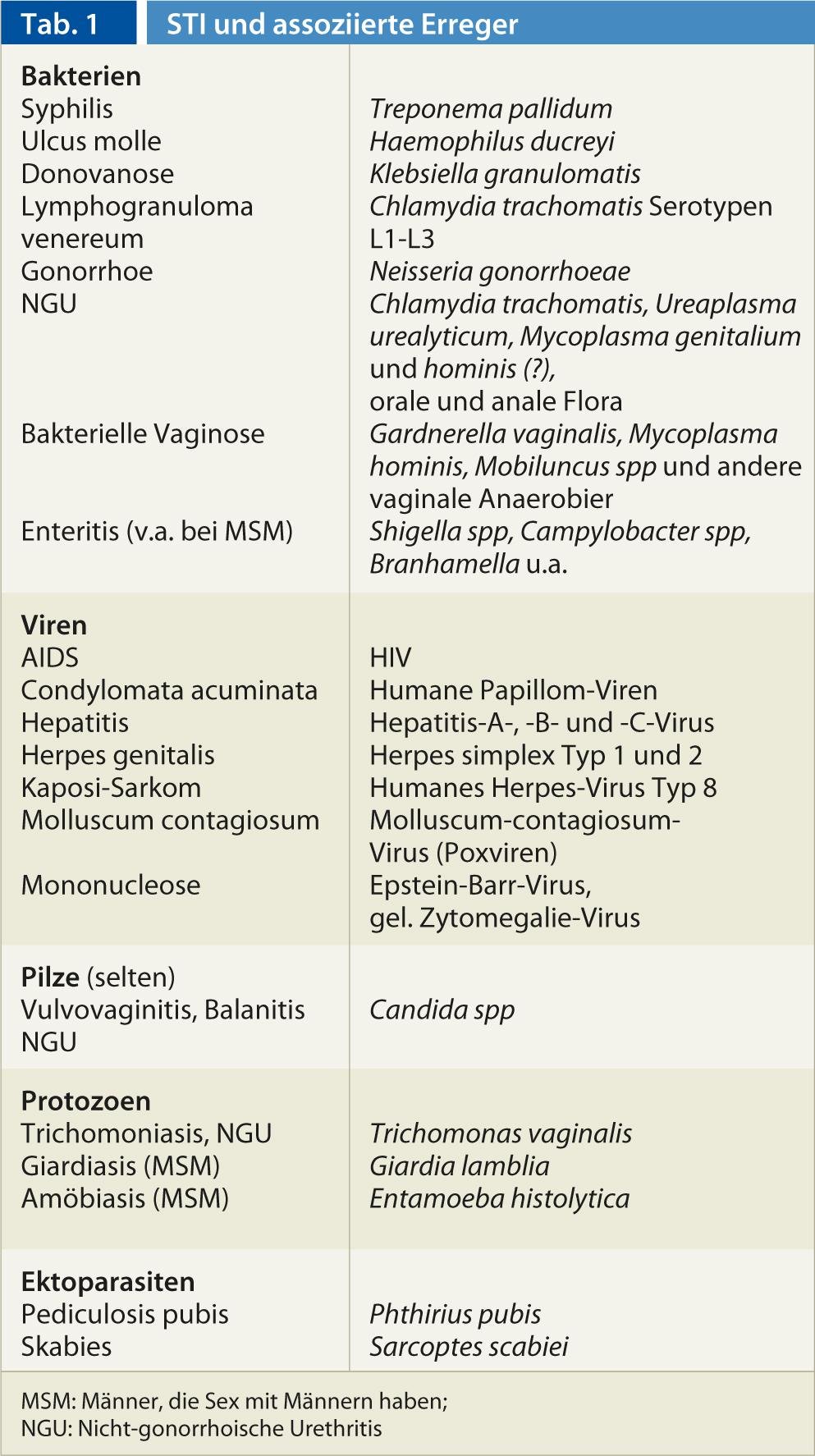

Fig. 1: Isolated superficial ulcer in recurrent genital herpes.
Encouraging developments in HPV infection
Promising publications from Australia have documented a massive reduction in the incidence of condylomata acuminata in young women vaccinated with quadrivalent HPV vaccine (against types 6, 11, 16, 18). Encouragingly, there was also a marked reduction in condylomas in men of the same age, but not in unvaccinated older persons or in homosexual men [11]. This trend was generally confirmed for Australia in the national surveillance network [12]. For the first time, a reduction in HPV-related genital changes could also be demonstrated in vaccinated men [13] and a decrease in the incidence of cytologic cervical changes in vaccinated women [14]. To what extent these encouraging data can be transferred to Switzerland, which has a much lower vaccination rate than Australia, only time will tell.
In addition to anogenital changes, the possibility of oral infection must also be considered. Recently, a prevalence of oral HPV infection of 6.9% of healthy individuals aged 14-69 years in the United States has been demonstrated(Fig. 2).

Fig. 2: Condylomata acuminata of the lip
Further encouraging is the almost complete disappearance of pediculosis pubis from clinical practice. However, this merely reflects the current trend in genital depilation.
Worrying developments
According to WHO estimates, 106 million people worldwide are affected by gonococcal infection each year. Since 1996, the incidence of gonorrhea in Switzerland has been increasing practically linearly every year. So far, this could be accepted without consequences, since the infection could be healed without problems with the correct choice and form of administration of the antibiotic. In recent years, however, there has been an alarming development of resistance, which justifiably leads to current fears of a future no longer treatable gonorrhea [5]. Only the third generation of cephalosporins should be used here, although a rapidly increasing proportion of strains with elevated minimal inhibitory concentrations has also been observed in the perorally administered forms, although this has not yet been observed in Switzerland. Consequently, in August 2012, the Centers for Disease Control in Atlanta no longer recommended peroral cephalosporins such as cefiximin as the drug of choice [15]. In this situation, only ceftriaxone 1× 250-500 mg i.m. can be recommended. In addition, the American, British, German, and European Guidelines (IUSTI) provide for the concomitant administration of 1-2 g azithromycin per os (alternatively doxycycline 2×100 mg for 7 days) to counteract the development of resistance based on theoretical considerations [15, 16]. Unfortunately, dosage recommendations are not consistent and have been changed repeatedly in recent months.
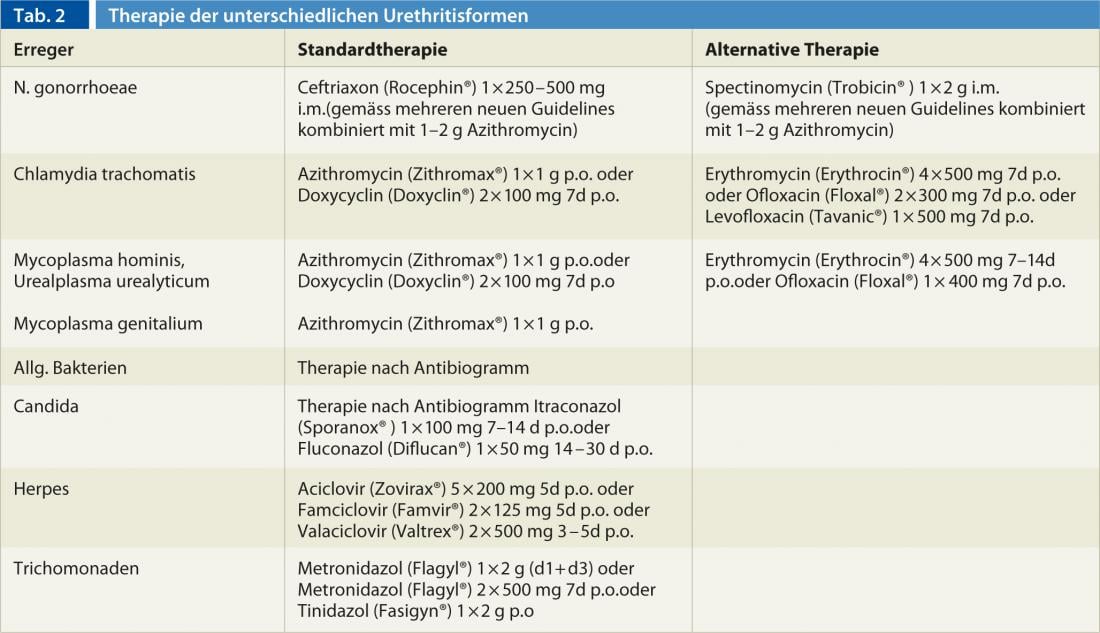
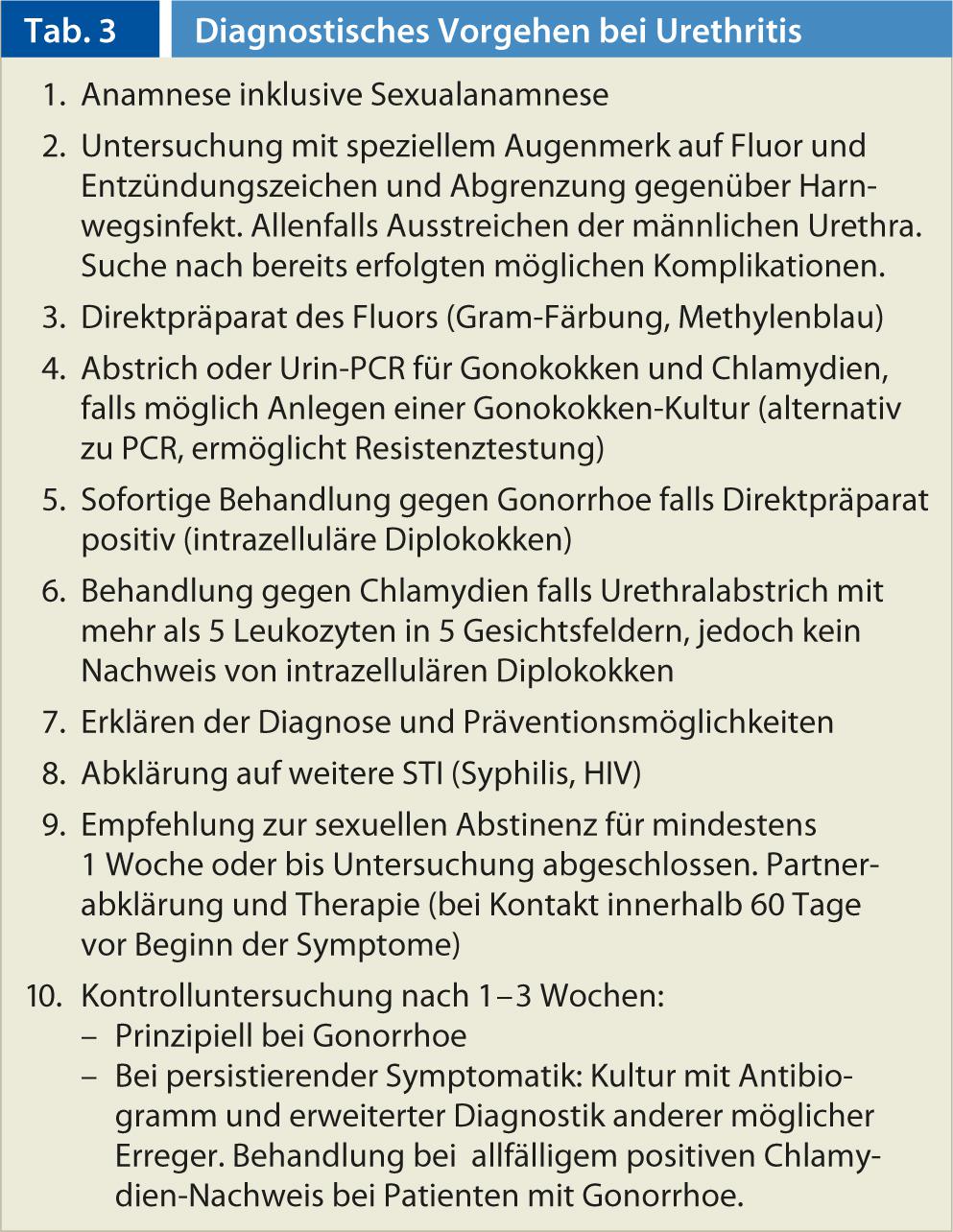
In urethritis, the increasing proportion of cases caused by Mycoplasma genitalium should additionally be mentioned, which results in diagnostic and therapeutic difficulties [17]. On the one hand, the diagnosis cannot be made culturally as with other mycoplasmas, but exclusively by PCR; on the other hand, the insufficient response to doxycycline should be mentioned, which is why treatment with azithromycin is preferable for this pathogen [18]. The therapy of urethritis according to the causative pathogen is listed in Table 2. The biological behavior and infection rates are comparable to those of Chlamydia trachomatis. The importance of this pathogen also for infections in the female genital tract is receiving increasing attention in the literature [19]. Table 3 lists a possible approach for patients with urethritis.
According to a comparison by the Robert Koch Institute, Switzerland occupies an inglorious top position in Europe with regard to the incidence of syphilis [20]. While neighboring countries such as Germany and Italy show significantly lower annualized incidence rates with a comparable reporting system, the increase in numbers in Switzerland, which has now lasted for ten years, continued unabated in 2013 according to the reports to the FOPH [8, 10]. Since syphilis has also reappeared during pregnancy, the possible transmission to the newborn – lues connata – must again be expected in our country [21]. Particularly in the case of indurated ulcers with accompanying lymph node swelling, primary syphilis should be considered not only in genital localization but also, in particular, on the lips and enorally(Fig. 4).

Fig. 4: Non-ulcerating syphilitic primary effect.
In addition to the proverbial chameleon-like pictures in the context of secondary syphilis, the primary stage can also cause different manifestations [22–24]. Multiple primary, nodular, rhagadiform, and phagedaniform forms as well as herpetiform ulcerations have been described [23]. In the global absence of resistance development in Treponema pallidum, benzathine penicillin should be used for therapy whenever possible.
Consequences
To better identify patients at risk, sexual history must also be addressed in daily practice. According to a recent patient survey from Lausanne [25], over 90% would like a sexual history, but this has been done in less than half of patient encounters to date. Particularly in the case of syphilis, screening should be performed in cases of unclear exanthema, in patients with other sexually transmitted infections or after risk contacts, in cases of frequently changing partners, and during every pregnancy. In daily practice, we should not only consider classical signs, but also unusual or minor symptoms (Fig. 3 and 4) think more about the presence of possible STDs and inform patients individually about possible risks and treat them according to the current guidelines [26–28].
Every workup of patients with a suspected STI includes examination of the anal region, since STIs can manifest perianally, endoanal, but also rectally with appropriate exposure (Fig. 5) [29]. In order to prevent further infections as early as possible, intensified partner notification and therapy are of utmost importance in addition to rapid and adequate diagnosis and therapy.

Fig. 3: Syphilitic primary effect of the lip
CONCLUSION FOR PRACTICE
- In Switzerland, STIs continue to be on the rise.
- With timely and consistent quadrivalent HPV vaccination, condylomas and genital dysplasia can be prevented.
- As a result of the threatening increase in the development of resistance
- for Neisseria gonorrhoeae should be treated with ceftriaxone 1×250-500 mg i.m. in combination with azithromycin 1×1-2 g p.o. whenever possible.
- In the case of unclear exanthema, after risk contacts, with frequently changing partners and during pregnancy, a lues clarification should be carried out in addition to a screening for HIV.
- Sexual history should also be obtained in primary care.
Prof. Dr. med. Stephan Lautenschlager
Literature:
- Deguchi T, et al: Sex Transm Dis 2004; 31: 192-195.
- Shahmanesh M, et al: Int J STD AIDS 2009; 20: 458-464.
- Berntsson M, et al: Int J STD AIDS 2010; 21: 191-194.
- O’Mahony C: Int J STD AIDS 2006; 17: 203-204.
- Bolan GA, et al: N Engl J Med 2012; 366: 485-487.
- Meyer Sauteur PM, et al: Swiss Med Wkly 2012; 141: w13325.
- Ward H, Ronn M: Curr Opin HIV AIDS 2010; 5: 305-310.
- Lautenschlager S: Dermatology 2005; 210: 134-142.
- Abraham S, et al: Dermatology 2006; 212: 41-46.
- Federal Office of Public Health. Infectious disease messages. www.bag.admin.ch/k_m_meldesystem
- Read TR, et al: Sex Transm Infect 2011; 87: 544-547.
- Donovan B, et al: Lancet Infect Dis 2011; 11: 39-44.
- Giuliano AR, et al: N Engl J Med 2011; 364: 401-411.
- Brotherton JM, et al: Lancet 2011; 377: 2085-2092.
- Centers for Disease Control and Prevention (CDC): MMWR Morb Mortal Wkly Rep 2012; 61: 590-594.
- Bignell C, Fitzgerald M: Int J STD AIDS 2011; 22: 541-547.
- Weinstein SA, Stiles BG: Sex Health 2011; 8: 143-158.
- Manhart LE, et al: Clin Infect Dis 2011; 53 Suppl 3: S129-S142.
- Patel MA, Nyirjesy P: Epid Bull 2009; 49: 503-512.
- Robert Koch Institute: Syphilis in Germany in 2008. Epid Bull 2009; 49: 503-512.
- Meyer Sauteur PM, et al: Swiss Med Wkly 2012; 141: w13325.
- Lautenschlager S, et al: Dermatology 2006; 212: 200-202.
- Dourmishev LA, Dourmishev AL: Clin Dermatol 2005; 23: 555-564.
- Lautenschlager S: Am J Clin Dermatol 2006; 7: 291-304.
- Meystre-Agustoni G, et al: Swiss Med Wkly 2011; 141: w13178.
- WHO: Guidelines for the management of sexually transmitted diseases. www.who.int/hiv/pub/sti/en/STIGuidelines2003.pdf
- CDC: MMWR 2010; 59; RR-12.
- International Union against STI. European Treatment Guidelines. www.iusti.org/regions/Europe/euroguidelines.htm
- Lautenschlager S: Sexually transmitted infections: Anorectal manifestations. Therapeutic Review 2013; in press.
HAUSARZT PRAXIS 2013; 8(8), 33-37











