At this year’s Swiss Forum for Mood and Anxiety Disorders of the Swiss Society for Anxiety and Depression (SGAD), Prof. Martin E. Keck, MD, Oetwil am See, presented for the first time the second part of the SGAD recommendations for the treatment of anxiety disorders. This second part is devoted to obsessive-compulsive disorders and post-traumatic stress disorder (PTSD) and was prepared by SGAD in collaboration with the Swiss Society for Obsessive-Compulsive Disorders (SGZ), the Swiss Society for Biological Psychiatry (SGBP), and the Swiss Society for Psychiatry and Psychotherapy (SGPP).
The SGAD treatment recommendations were based on the guidelines of the World Federation of Societies of Biological Psychiatry (WFSBP) [1], which were adapted to local conditions and practices. The evidence criteria used are also consistent with those of the WFSBP. Prof. Martin Keck, MD, emphasized that the application of treatment recommendations must always take into account the patient’s own clinical experience, or as Dr. David Sackett, the founder of EBM, put it, “Practicing evidence-based medicine (EBM) means integrating individual clinical experience with the best available external evidence from systematic research.”
Treatment principles
For both conditions, obsessive-compulsive disorder and post-traumatic stress disorder (PTSD), evidence-based psychotherapy is generally the first-line treatment. For moderate to severe impairment, additional drug therapy is often recommended. One must always be aware that the effect of the medication is usually delayed. Although many of the substances used are not approved for these indications, they can still be used off-label, which only requires brief documentation. It is important to have an individual therapy plan with multimodal treatment, which always includes psychoeducation.
Treatment should last at least six months to two years and continue for twelve to 24 months after remission. “Always keep in mind in the context of guidelines that they assume ideal-typical patients, i.e., those without comorbidities, whereas in everyday clinical practice we are usually dealing with very complex cases,” Prof. Keck added.

Obsessive Compulsive Disorder
Evidence-based psychotherapy – treatment of first choice for OCD – has slightly higher success rates than pharmacotherapy and, in particular, better stability. The high complexity of the disorder often requires multimodal approaches, with cognitive behavioral therapy (CBT) being the best studied and considered the gold standard. It is recommended to combine CT with systemic, psychodynamic and mindfulness-based elements. The individual building blocks of psychotherapy should be selected based on a careful behavioral analysis (causative, triggering, maintaining conditions). Special attention should be paid to intrapsychic and interpersonal functioning, as these are the most common reasons for treatment failure and discontinuation. The core component of CT must always be exposure to response management in sensu and in vivo. In terms of cognitive interventions, identification, review, and correction of intrusive obsessive thoughts and, most importantly, metacognitions (modification of underlying basic assumptions) are recommended.
In pharmacotherapy, selective serotonin reuptake inhibitors (SSRIs) are primarily recommended (Table 1). Clomipramine, which is considered the gold standard and standard comparator, has the only disadvantage that it has unpleasant side effects in individual cases. Response rates (caveat: not to be confused with remission rates!) are 60-80%. A delayed onset of action of four to six weeks and the onset of the maximum effect after twelve weeks can be expected. The duration of maintenance therapy is individual, usually a duration of twelve to 24 months is recommended. In individual cases, very high dosages are necessary (off-label use). “Keep in mind that after pharmacotherapy alone, relapse rates are very high, so you should always combine it with psychotherapy. The gold standard is the combination of KVT plus antidepressant,” Prof. Keck emphasized. In the absence of a response to SSRIs (according to the guideline, at least 3 months and high-dose), augmentation with a neuroleptic is successful in 30% of patients. As ultima ratio, deep brain stimulation or ECT (electroconvulsive therapy, evidence category B3) may be considered.
Obsessive Compulsive Disorder
Evidence-based psychotherapy – treatment of first choice for OCD – has slightly higher success rates than pharmacotherapy and, in particular, better stability. The high complexity of the disorder often requires multimodal approaches, with cognitive behavioral therapy (CBT) being the best studied and considered the gold standard. It is recommended to combine CT with systemic, psychodynamic and mindfulness-based elements. The individual building blocks of psychotherapy should be selected based on a careful behavioral analysis (causative, triggering, maintaining conditions). Special attention should be paid to intrapsychic and interpersonal functioning, as these are the most common reasons for treatment failure and discontinuation. The core component of CT must always be exposure to response management in sensu and in vivo. In terms of cognitive interventions, identification, review, and correction of intrusive obsessive thoughts and, most importantly, metacognitions (modification of underlying basic assumptions) are recommended.
For pharmacotherapy, selective serotonin reuptake inhibitors (SSRIs) are primarily recommended (Table 1). Clomipramine, which is considered the gold standard and standard comparator, has the only disadvantage of having unpleasant side effects in isolated cases. Response rates (caveat: not to be confused with remission rates!) are 60-80%. A delayed onset of action of four to six weeks and the onset of the maximum effect after twelve weeks can be expected. The duration of maintenance therapy is individual, usually a duration of twelve to 24 months is recommended. In individual cases, very high dosages are necessary (off-label use). “Keep in mind that after pharmacotherapy alone, relapse rates are very high, so you should always combine it with psychotherapy. The gold standard is the combination of KVT plus antidepressant,” Prof. Keck emphasized. In the absence of a response to SSRIs (according to the guideline, at least 3 months and high-dose), augmentation with a neuroleptic is successful in 30% of patients. As ultima ratio, deep brain stimulation or ECT (electroconvulsive therapy, evidence category B3) may be considered.
Post-traumatic stress disorder
Evidence-based psychotherapy is also considered the first-line treatment for post-traumatic stress disorder. Trauma-focused interventions using cognitive behavioral therapy with exposure-response management have been most successful. In this regard, Prolonged Exposure Therapy (psychoeducation, imaginal and in vivo exposure), Cognitive Processing Therapy (confrontation limited to the worst moments [hot spots]) and Imaginery Rescripting and Antialptraumtraining (e.g., alternative dream) have been shown to be equivalent. Well proven in effectiveness and therefore recommended is EMDR (Eye-Movement Desensitization and Reprocessing).
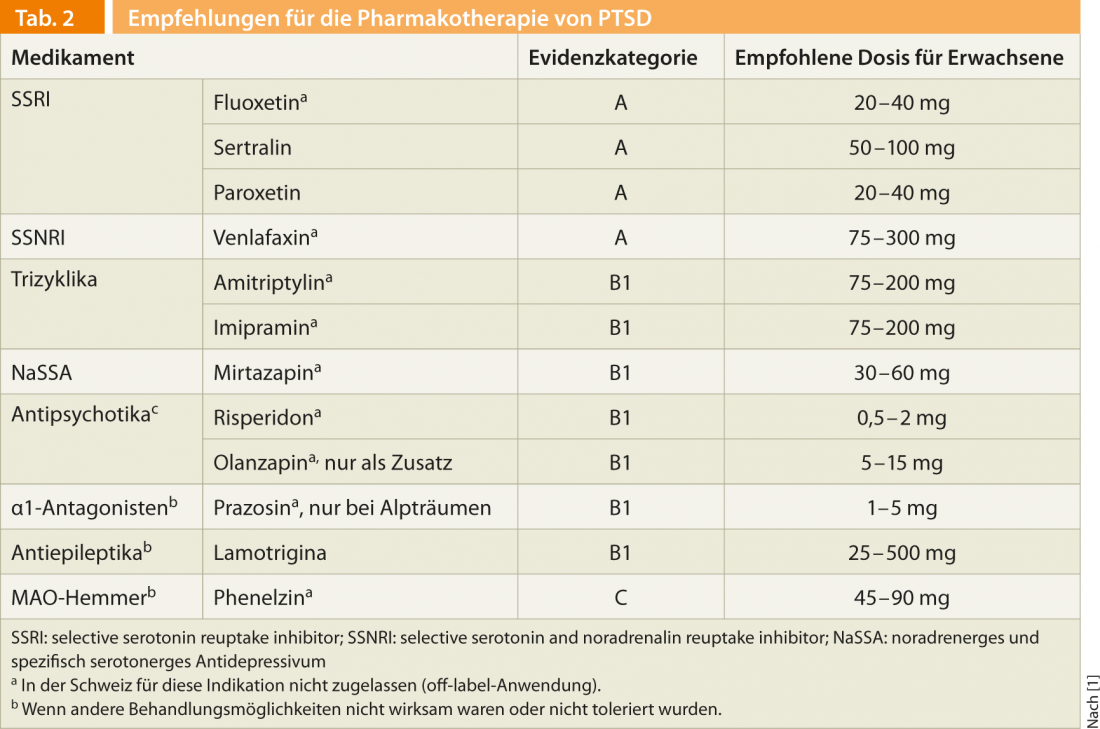
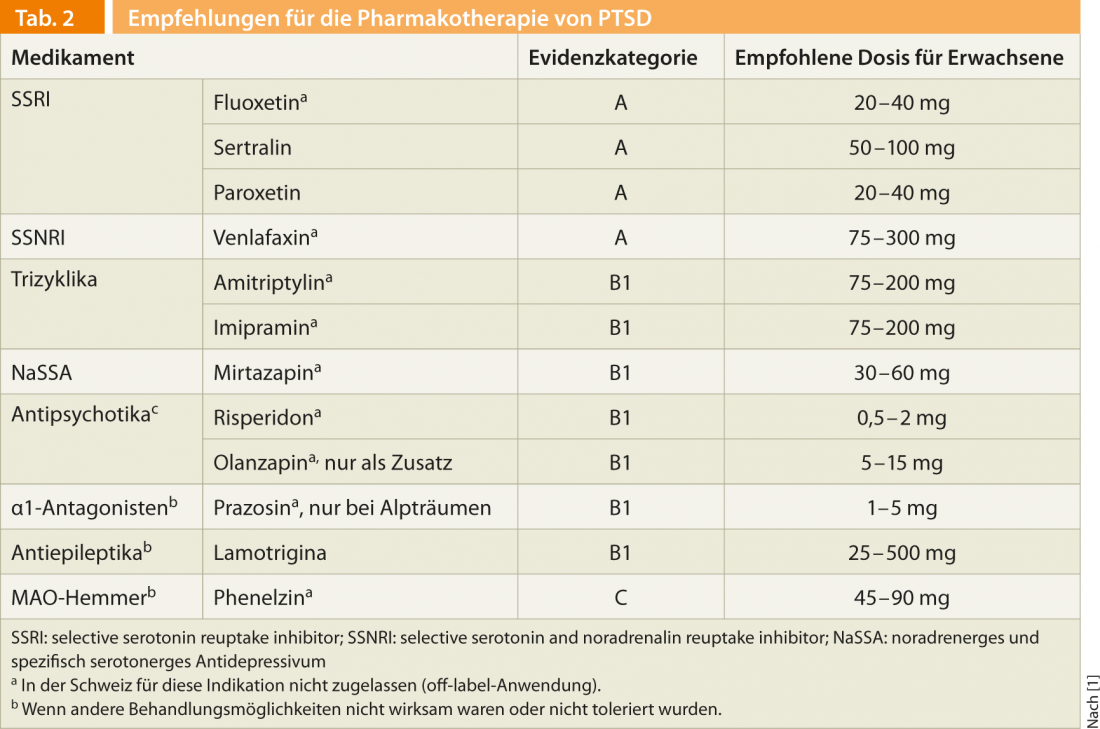
Pharmacotherapy is indicated only when psychotherapy alone is not sufficient or, as is very often the case, comorbidities such as depression, anxiety disorders, dissociative or somatoform disorders, addictive disorders, etc. are present. If the patient responds to pharmacotherapy, it should be continued for at least twelve months. The recommended substances are summarized in Table 2.
Since PTSD are triggered by a circumscribed event, the question arises whether they could not be prevented by effective secondary prophylaxis. It is important to note here that only about 10-50% of those affected by a traumatic event ever develop PTSD. The consensus today is that debriefing after the event not only doesn’t help, but can actually hurt, and is therefore obsolete. Moreover, the evidence regarding prophylactic measures is very unclear. “Central to secondary prevention is certainly stabilization, although the approach can vary greatly from individual to individual. A good social environment is certainly one of the best prognostic factors,” Prof. Keck explained. In certain cases, the short-term (a few days to a maximum of 3-4 weeks) administration of benzodiazepines may be useful in the initial period after trauma for symptomatic treatment of anxiety and sleep disorders to bridge the effect of antidepressants. However, these have no prophylactic effect.
Literature list at the publisher
Source:4th Swiss Forum for Mood and Anxiety Disorders (SFMAD), Zurich, April 18, 2013.











