While many primary care physicians were skeptical of “remote treatment,” more and more physicians are now working in partnership with telemedicine providers.
Let’s start with a fictitious case study: The 63-year-old general practitioner, let’s call him Dr. med. Paul Lutz, has always preferred to spend his vacations in his vacation cottage in Maloja in the Upper Engadine. It has long been a dream of Lutz and his wife to move there completely. However, he still felt too young to give up his flourishing practice in Thalwil ZH and retire completely – he was also too attached to his work. Then he learned about the opportunity to telemedicine part-time regardless of where he lived. After long consideration and intensive discussions with his wife, who supported him as a trained MPA, he sold his practice and moved with her to the Engadine. For the past year, he has been caring for patients via telephone from his home office in Maloja five days a week every morning between 9 a.m. and noon.
Definition of terms
Telemedicine is a subset of eHealth. The interaction takes place between
- Patient and medical consultant (triage)
- Patient and doctor (teleconsultation)
- or among physicians (teleconsil)
in connection with medical diagnosis or treatment, where the parties involved are not in direct physical contact with each other.
Telemedicine enables location- and time-independent, electronically supported services that are close to citizens and their needs.
The terms telemedicine and telehealth are used interchangeably. Telehealth emphasizes individual maintenance and population-wide promotion of health (public health), which extends beyond disease-centered health services.
Globally, eHealth is now considered to be of the highest strategic importance in health policy prioritization.
Telemedicine pioneers in Basel and Bern
For Medgate, Switzerland’s largest telemedicine consulting center headquartered in Basel, the scenario with Paul Lutz is not a utopia: “We are working on tapping additional medical resources and are looking for doctors who work part-time from home. We already have various doctors, even in peripheral regions such as Ticino, who are affiliated with our network. They are also doctors with small children who want to work temporarily from the home office,” explains Medgate’s marketing manager, Cédric Berset.
Medgate, together with Bern-based Medi24, has been one of Switzerland’s pioneering telemedicine providers since 1999. With 70 doctors, the Basel-based company is now the leader in its sector throughout Switzerland. In addition to general practitioners, the in-house medical team also includes specialists in internal medicine, gynecology or dermatology. Patients with skin problems have been able to use image-assisted telediagnostics for five years: Photos are emailed to Medgate and examined by dermatologists. Patients are counseled and, if necessary, referred to a specialist’s office for a face-to-face consultation. Medgate plans to allow primary care physicians to send images of their patients’ skin lesions for reporting in the future.
In-house physicians are supported by 50 certified nurse practitioners and medical office assistants and 60 call center staff. Before a physician can work for the company, he or she is trained in the FMH-approved in-house training center for telemedicine service provision. Medgate has a special practice permit from the Basel Health Department, which also controls the training.
Telemedicine counselors triage patients to appropriate care providers for treatment. Thus, patients with acute or general health issues could also be referred by telephone to our fictitious Dr. Lutz in Maloja. He would instruct patients on sensible self-care, write prescriptions for medications for certain conditions, or refer patients to their primary care physician’s office as needed. Medgate claims to have performed 3.4 million teleconsultations since anno 2000, up to 4300 per day. Cost of a Medgate private membership: for one person CHF 100 per year, families pay CHF 150 .
A must for insurers
Many health insurers work with Medgate and Medi24. As a rule, telemedicine consultations are free of charge for customers of health insurers. Helsana, for example, writes on its website: “A competent and independent advisory team of medical professionals will be happy to help you and provide specific recommendations and expert information on medical issues. This service is free of charge for Helsana customers.” The health insurer gives examples of cases in which the telephone health advice service has been requested:
- “Could my child have meningitis?”
- “Tick bite while jogging: What Should I Do?”
- “Lumbago after moving”
- “Abdominal discomfort after vacation abroad”
- “Earache after a day of skiing in the Valais”.
“Today’s clientele expects a good health insurer to offer telemedicine consulting,” explains Patrick Elmiger, head of strategic projects at health insurer Concordia. Along with Swica, Concordia is the first health insurer to offer an in-house telemedicine consultation under the concordiaMed name. The counseling center was opened in July 2012. The services include an assessment of the medical situation, within which time a visit to the doctor is indicated, instructions for self-treatment if a visit to the doctor is not necessary, assistance with emergency measures at home and abroad as well as with problems and administrative questions on site during a stay abroad, information on generic drugs and vaccination information.
Do such insurance offerings compete with primary care physicians? “As far as we are informed, telemedicine providers are accepted by primary care physicians. We save the family doctors many unnecessary emergency consultations that would disrupt their organizational processes. Consultations are eliminated in which family physicians have no medical interest at all. We take over part of the night and weekend service. Our team of consultants is on duty 24 hours a day, 7 days a week, and there is always a doctor available for more detailed information. Our telemedicine service is also a contribution to solving the problem of the shortage of family doctors, especially in rural areas,” says Elmiger. He knows from his own experience that there are fewer and fewer family doctor’s offices in rural areas of Lucerne, for example.
About 40-50% of callers can be directed to self-treatment, according to Elmiger. The rest are advised to see a doctor within a precisely defined time. According to Elmiger, patient satisfaction is very high: “Every insured person who has called is given a questionnaire. Over 90% say they are satisfied to very satisfied with the telephone consultation.”
Chronic Care Management
The young industry is also gaining a foothold in the field of telemedical care for the chronically ill, even if the topic is fundamentally controversial(see interview). “Telemedical Chronic Care Management (CCM) is a standardized and individualized telemedically supported care for chronically ill patients. The necessary measuring devices and intervention arms are individually compiled for the patient and provided within the framework of the cost approval granted by the health insurer,” explains Berset.
The primary care physician providing care would be involved in the telemedicine treatment process. He could be trained in the basic skills of telebiometry, which would allow him to be reimbursed for telemedicine services. At Medgate, this is currently possible with the telemedical care of patients from the CSS insurance collective, with whom this process is already established. Other health insurers are expected to follow suit.
The basis of the CCM is the telelaboratory. This is the technical equipment for telemonitoring as well as alarm management and consists of the following components:
- Measuring devices: blood pressure/pulse, blood glucose, weight, heart failure questionnaire(e.g. Fig. 1)
- Base station (gateway): does not require an Internet connection at the patient’s home
- Central: Password-protected, web-based online patient file with master data and measured values; their receipt, evaluation and visualization.
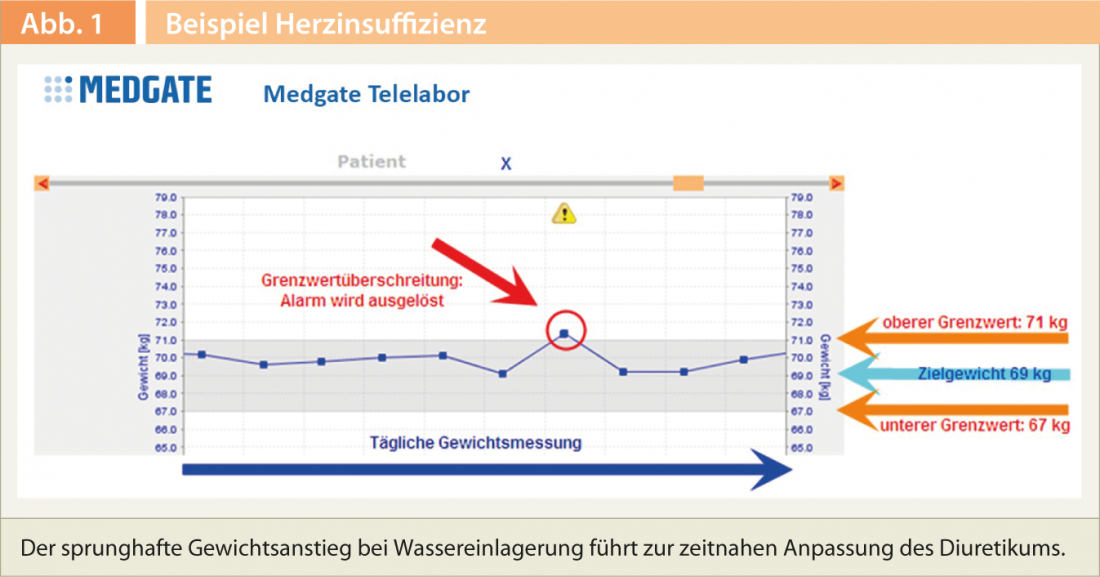
Telebiometry is the permanent measurement, monitoring and evaluation of the recorded measured values and is the basis for continuous therapy adjustment.
The alarm management ensures a prompt response to derailment of the measurement parameters when standardized and individualized limit values are exceeded. The basic examination – in the form of an actual consultation in the general practitioner’s or specialist’s practice – includes the clinical, instrumental and laboratory examinations for the diagnosis and therapy of the clinical picture, in which the required findings are collected (see, for example, Fig. 1) . Patient education is basic medical training for the patient on the clinical picture. It can be done on site, or by telephone.
“Telemedicine services are very useful in the care of patients with chronic diseases. This area is growing enormously – due to increasing life expectancy. Here, the integrated approach is of utmost importance, which includes the smooth cooperation between the general practitioner, the patient and the telemedicine center,” explains Medgate.
Much still in its infancy
An aging population, more chronically ill patients, rising costs: among other things, these factors will help telemedicine achieve a further breakthrough. Telemedicine providers are optimistic. The possibilities are far from exhausted – on the contrary: many things are still in their infancy, and the potential is great. “We have a long list of medical offerings possible in the future, from which we will realize the most important ones according to our strategy,” says Patrick Elmiger. Cédric Berset also explains, “We are in the process of further intensifying collaboration between the telemedicine center and primary care physicians in the spirit of integrated care.”











