A review article with a special focus on the possible skin manifestations on hands and feet in classic collagenoses, such as lupus erythematosus, systemic scleroderma, dermatomyositis, and Sharp syndrome.
It is well known that the classic collagenoses lupus erythematosus, systemic scleroderma, dermatomyositis and Sharp syndrome (synonym: mixed collagenosis) can cause various cutaneous symptoms and organ damage. This review article focuses exclusively and specifically on the area of the hands and feet, respectively on the possible skin manifestations on hands and feet in collagenosis.
Raynaud’s phenomenon
Raynaud’s phenomenon (synonymously Raynaud’s disease, Raynaud’s syndrome) is common to almost all collagenoses, which is why it should be placed before the other descriptions as a superordinate skin phenomenon on hands and feet. This is typically understood as a characteristic three-color play of the hands triggered by cold or emotional stress: white, blue, red, which is why one also speaks of the so-called tricolor phenomenon . This is due to a sympathetic dysregulation of the autonomic nervous system, which causes excessive vasoconstriction of the arterioles via receptors, leading first to ischemia with numbness and pain in the affected areas (white) and then to cyanosis due to hypoxia (blue). Usually, these spasms resolve on their own, resulting in the final reactive hyperemia with redness and tingling (red). Only this characteristic color sequence is defined as Raynaud’s phenomenon and should be described in the medical history documentation. The primary Raynaud ‘s syndrome is to be distinguished from the secondary Raynaud’s syndrome. In primary Raynaud’s syndrome, which occurs much more frequently, there is no causal or concomitant underlying disease, in contrast to secondary Raynaud’s syndrome, which can already be distinguished by the clinical appearance with asymmetric involvement of individual fingers and the detection of antinuclear antibodies. Thus, when Raynaud’s phenomenon occurs in the collagenoses, it is by definition the secondary form.
Systemic scleroderma
Already relatively early in systemic scleroderma (sclerosis), characteristic skin changes appear on the hands and feet, which is why the suspected diagnosis of systemic scleroderma can often be made on this basis alone.

Clinically, a distinction is made between a stage oedematosum with doughy edematous swollen fingers (Fig. 1A and 1B) from the later developing stage sclerosum with waxy hardened, non-sliding finger skin (sclerodactyly) (Fig. 1C). In the final stage, a claw-like fixation and posture of the fingers (“dermatogenous flexion contractures”) finally occurs. (Fig. 1D). The fingers also become significantly thinner toward the fingertips, which is aptly described by the term “Madonna fingers” (Fig. 1E). At the distal end, trophic disturbances and necrosis (“rat bite necrosis”) may occur (Fig. 1F). The nails may also show trophic changes accordingly.
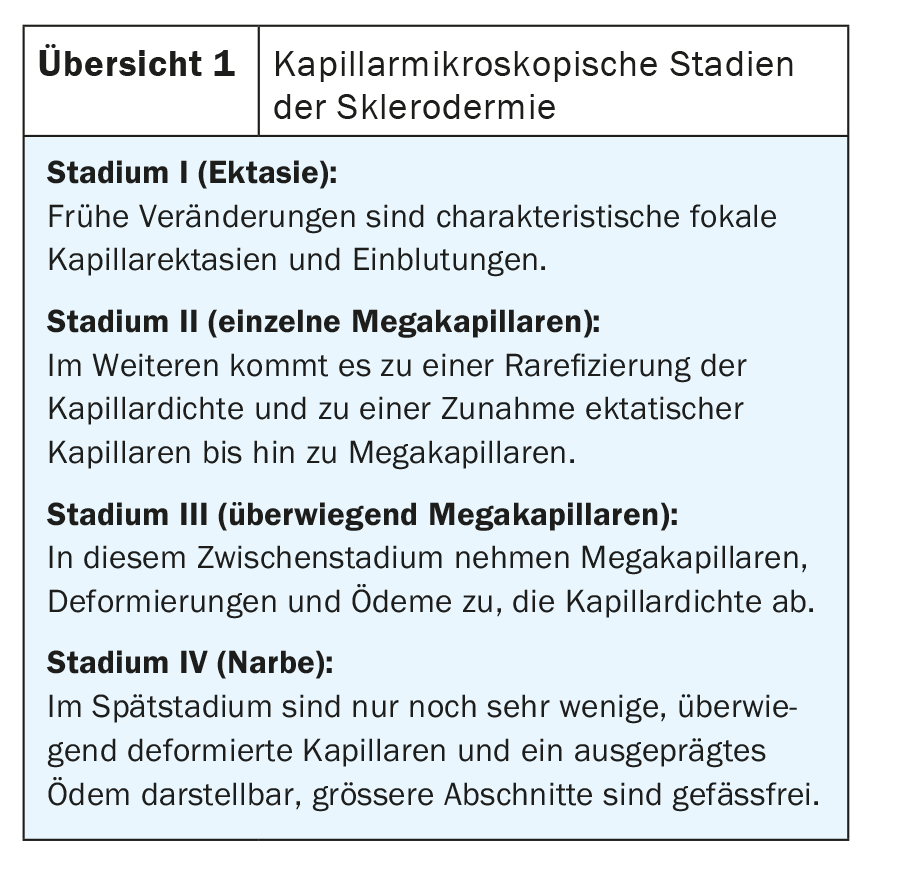
Capillary microscopically, all pathologies can be observed in scleroderma patients, sometimes even simultaneously, side by side. Typically, however, different stages can be distinguished from each other (overview 1).
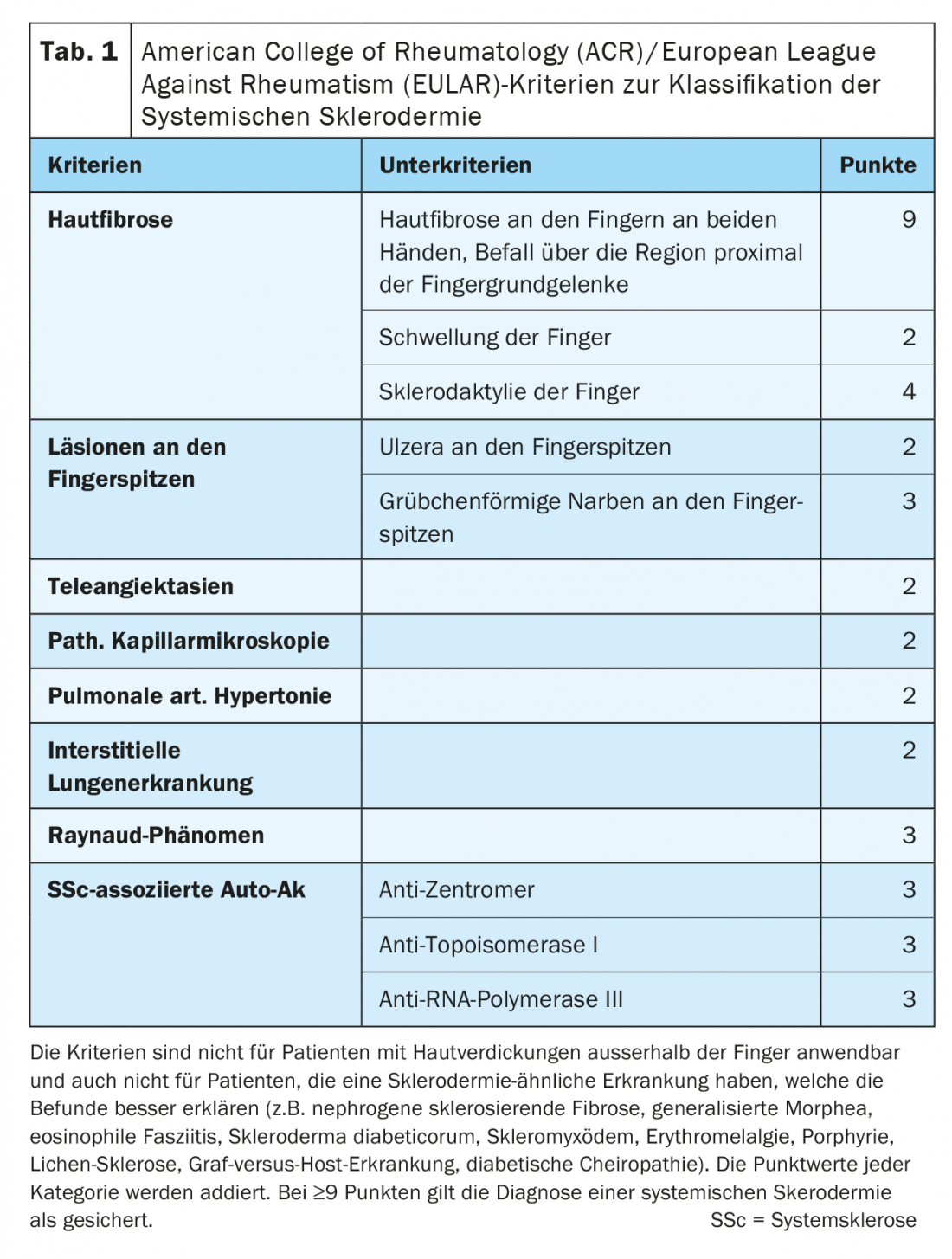
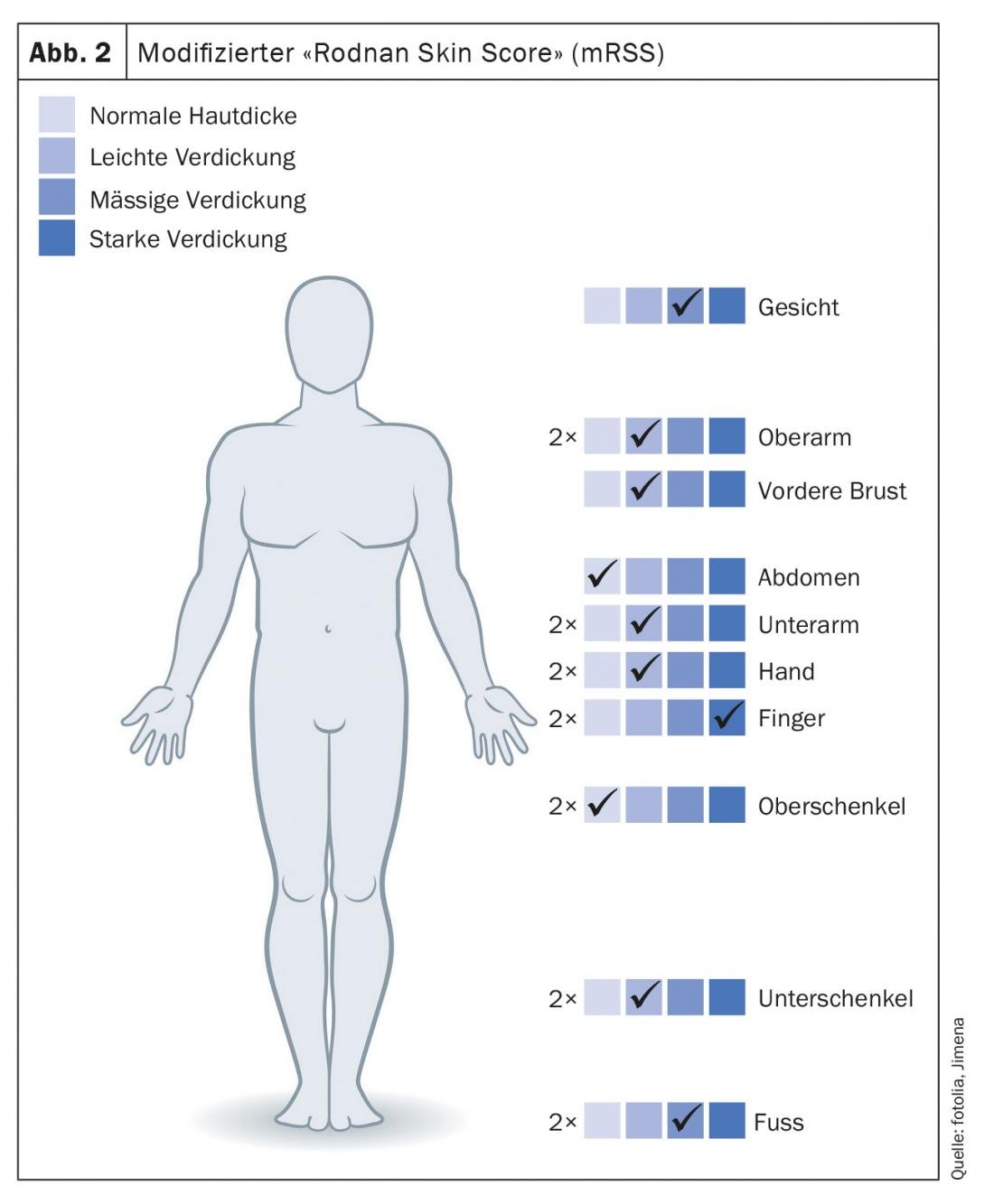
The skin changes on the hands and feet, which are so typical for systemic scleroderma, are also reflected accordingly in the “scores” and classifications for diagnosis and severity. Based on the criteria of the American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR), systemic scleroderma can be diagnosed almost solely on the basis of skin changes on the hands. (Table 1). The modified 1995 “Rodnan Skin Score” (mRSS) is still considered the best validated correlation parameter for estimating organ involvement, especially lung involvement. In 17 regions, with hands and feet represented a total of six times, skin sclerosis is assessed with a score of 0-3 ( Fig. 2).
Systemic lupus erythematosus (SLE)
Skin lesions on the hands and feet are less specific in systemic lupus erythematosus than in systemic scleroderma. There are livedo racemosa, patchy red, sometimes keratotic plaques on the dorsal sides of the fingers or on the plantae (Fig. 3A), diffuse livid erythema on the palmae and plantae (Fig. 3B) and on the finger and toe end phalanges, telangiectasias periungual and on the fingertips, and small hemorrhages on the nail fold (Fig. 3C).
In capillary microscopy, SLE patients usually present a colorful picture with an accumulation of various pathological changes. Thus, caliber variations, “sludge”, branching and elongation are predominant.

Chilblain Lupus
Chilblain’s lupus is the rare, acquired variant of cutaneous lupus erythematosus with acral localized, cold-induced, pressure-dolent plaques reminiscent of pernions, which is why it is often overlooked and undiagnosed. It occurs almost exclusively in women, especially in the cold season and in cooler latitudes – before, with or after other manifestations of cutaneous or systemic lupus erythematosus.
In the early stages, there are extensive, deep red swellings, plaques and nodules reminiscent of chilblains.
Over the course of years, reddish-livid, indistinct, markedly indurated hyperkeratotic plaques then develop, either surface smooth or coarse lamellar scaling. Hyperesthesia, central atrophy, erosions or rhagades over the dorsal parts of the finger joints or even extensive ulcerations may occur (Fig. 4). A seasonal course is typical with a clear accentuation of the skin symptoms in the cold season and equally clear, but usually not complete remission in the summer months.

In 2006, a familial form of Chilblain lupus was described for the first time, based on a mutation of the TREX1 gene.
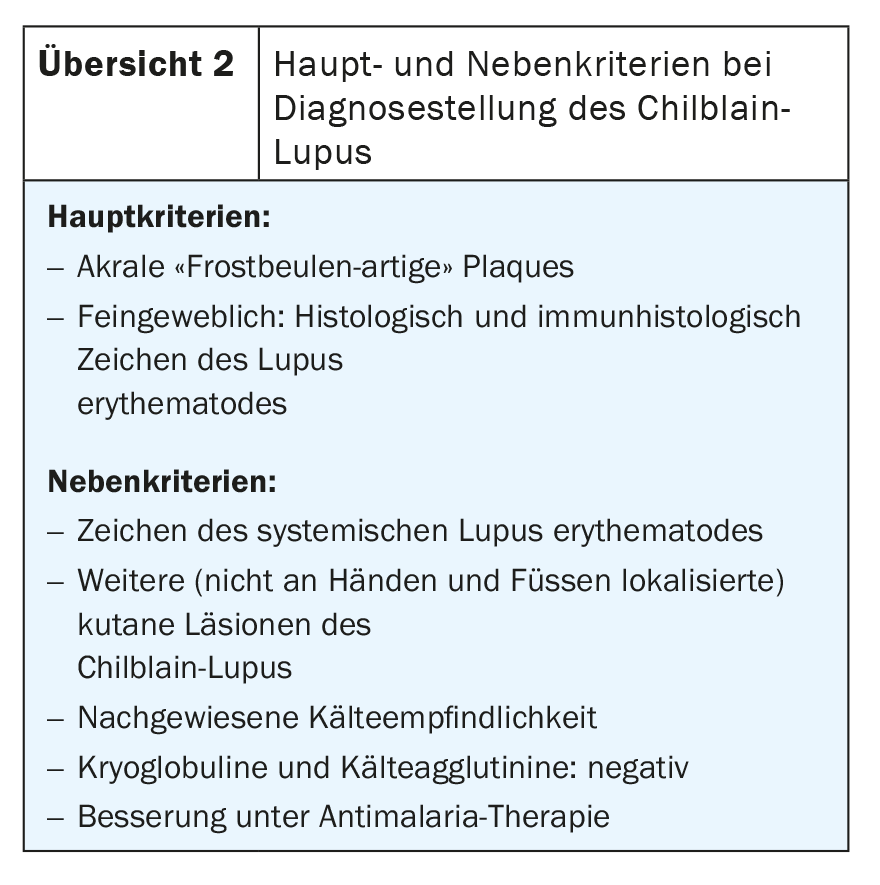
The laboratory usually shows hypergammaglobulinemia. ANA: frequently positive; antiphospholipid-Ak, anti SSA/Ro variably positive; ds-DNA: negative; accelerated BSR. Variable: Decrease of C3 and C4. The diagnosis is considered confirmed if two major criteria and one minor criterion from Overview 2 are met. Differential diagnosis should include true chilblains (pernions), sarcoidosis (lupus pernio), thrombosis, and less commonly, cryoglobulinemia, macroglobulinemia, or vasculites.
Dermatomyositis
Patients with dermatomyositis may develop characteristic skin symptoms on the hands and feet. The dorsal sides of the fingers often show reddish, porcelain-white papules (“Gottron papules”) (Fig. 5). Periungual erythema with telangiectasia and splinter hemorrhages as well as hyperkeratosis of the eponychium are frequently found, the retraction of which is felt to be painful and is referred to as “Keining’s sign” (Fig. 6) . In addition, the nails may present as lackluster and ridged. Capillary microscopy shows predominantly capillary ectasia and hemorrhage, with no rarefaction of the vessels. The relative hyperemia and slowed blood flow provide the microscopic correlate to the visible livid discoloration of the skin.



Mixed Connective Tissue Disease (Sharp Syndrome)
Depending on the severity and leading symptoms, Sharp’s syndrome presents with sometimes specific, sometimes non-specific skin changes on the hands and feet. Sclerodactyly is predominantly found in more systemic scleroderma prone patients. Periungual erythema with telangiectasias as well as livid erythema (Fig. 7) are more characteristic of lupus or dermatomyositis overlap.
Further reading:
- Krieg T: Scleroderma. Dermatology and Venereology, 5th ed, 676-689. Springer Verlag 2005.
- Meurer M: Lupus erythematosus. Dermatology and Venereology, 5th ed, 690-705. Springer Verlag 2005.
- Messer G: Dermatomyositis and other autoimmune diseases. Dermatology and Venereology, 5th ed, 706-715. Springer Verlag 2005.
- Hunzelmann N, Krieg T: Scleroderma: dermatology, venereology and allergology, 6th edition, 849-865. Springer Verlag 2012.
- Sticherling M, Kuhn A: Lupus erythematosus dermatology, venereology and allergology, 6th edition, 866-882. Springer Verlag 2012.
- Eming R: Dermatomyositis and other autoimmune diseases. Dermatology, Venereology and Allergology, 6th ed, 883-896. Springer Verlag 2012.
- Hunzelmann N: Systemic scleroderma. Der Hautarzt 2013; 64: 299-312.
- Persa OD, et al: Systemic scleroderma. Der Hautarzt 2015; 66: 599-603.
- Volc-Platzer B: Dermatomyositis – update. Der Hautarzt 2015; 66: 604-610.
- Günther C, Beisserter S: Lupus erythematosus. Der Hautarzt 2015; 66: 611-616.
- Altmeyer’s Online Encyclopedia. (www.enzyklopaedie-dermatologie.de)
- Sander S, et al: Pocket Atlas of Capillary Microscopy, 3rd edition, 2008.
DERMATOLOGIE PRAXIS 2022; 32(4): 10-13











