Sport is also possible with a pacemaker. What should I pay attention to when programming the pacemaker? What are the possibilities offered by frequency-adaptive aggregates? And what aspects need to be considered before, during and after surgery?
Sport is the medicine of our century. Sport is understood in the broadest sense. So it also includes regular physical activities such as fast walking, cycling, walking or swimming, which should be done three to five times a week for at least 30 minutes to achieve better performance, health and well-being. Study results show that regular physical activity reduces all-cause mortality by about 35% [1,2].
This makes it clear: sports or targeted physical training should be practiced by both healthy individuals and those with the disease whenever possible. Patients who have had a pacemaker implanted also benefit in principle.
Limitation: underlying disease of the heart
What physical training or sports can be done depends less on the pacemaker and more on any heart disease. Pacemaker wearers without structural heart disease can participate in sports almost without restriction.
However, approximately 80% of patients who require a pacemaker are over the age of 70. Concomitant diseases such as arterial hypertension, coronary heart disease or heart failure are more common in this age group. The resulting performance must be determined individually by the cardiologist in charge. It provides the basis for selecting an appropriate sport and intensity. In principle, it is possible to exercise sensibly with almost any heart condition.
Pacemaker indication
A pacemaker is used to treat bradycardic arrhythmias. In 2016, almost 75,000 pacemakers were implanted as inpatients in Germany. In 44%, the indication was AV block 2. or 3rd degree, in 37% a symptomatic diseased sinus node was causative and in 15% of patients atrial fibrillation with bradycardic conduction was present [3]. According to the guideline of the European Society of Cardiology, in patients with AV block, there is – after exclusion of passive causes – a need for 2. or 3rd degree always a class I indication for implantation of a pacemaker. This is independent of the occurrence of symptoms. In contrast, patients with a diseased sinus node must have corresponding symptoms [4].
The principle of “physiological” stimulation is followed in the selection of pacemaker systems to be implanted. This means that the pacemaker is intended to take over the function of the defective stimulus-forming or stimulus-conducting system. For example, in patients with diseased sinus node, dual-chamber pacemakers are implanted that have an algorithm for AV node management. This ensures adequate atrial pacing while avoiding unnecessary ventricular pacing as long as AV conduction is intact. Patients with AV block also require a dual-chamber system, with the intrinsic P wave triggering ventricular pacing. Today, pacemakers with only one electrode are used almost exclusively in patients with permanent atrial fibrillation.
The systems consist of the actual unit with battery and electronics implanted infraclavicularly on the right or left side, and one or two electrodes placed in the heart. Wireless aggregates are now also used in isolated cases. Here, a miniaturized pacemaker of approximately 0.8 cm3 is anchored in the right ventricle. Currently, wireless pacemakers are only available as VVIR systems, i.e., suitable for patients with bradycardia-conducted atrial fibrillation.
For the question of sporting activity, the choice of pacemaker system does not play a role for the patient. However, wireless systems eliminate the risk of mechanical interference during certain sports.
Pacemaker function and programming during stress
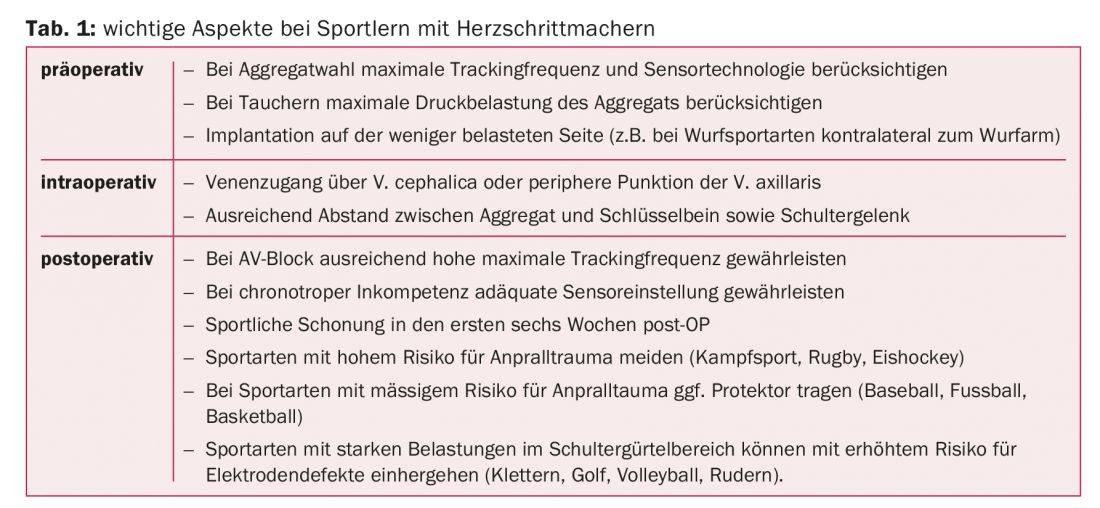
When physical exertion begins, there is an increase in heart rate within 10 to 45 seconds, as well as in the volume of blood pumped by the heart. Patients with AV conduction dysfunction usually demonstrate an adequate rate increase at the atrial level (chronotropic competence). The task of the pacemaker is to stimulate the ventricle following atrial excitation in the event of AV nodal conduction failure: the intrinsic P wave sensed by the atrial electrode triggers ventricular pacing (so-called VAT pacing). For sports activities, it is necessary that the pacemaker can also transmit high sinus frequencies to the ventricle, i.e. the maximum tracking frequency is programmed sufficiently high. Depending on the type of sport, age and any concomitant disease and medication, 130/min may be sufficient, but it may also be necessary to be able to achieve frequencies of 160-180/min. Young patients may require even higher frequencies. However, only certain pacemaker models allow a maximum tracking frequency above 180/min. This must be taken into account when selecting the aggregate.
In order for the pacemaker to realize high tracking frequencies, the AV time (time between perception of atrial excitation and ventricular pacing, roughly comparable to PQ time in intrinsic conduction) and the refractory periods must be programmed accordingly. If this is not taken into account, a pseudo-Wenckebach behavior of the pacemaker or even a 2:1 block with sudden halving of the ventricular frequency under heavy load occurs at high sinus frequencies (Fig. 1-2).
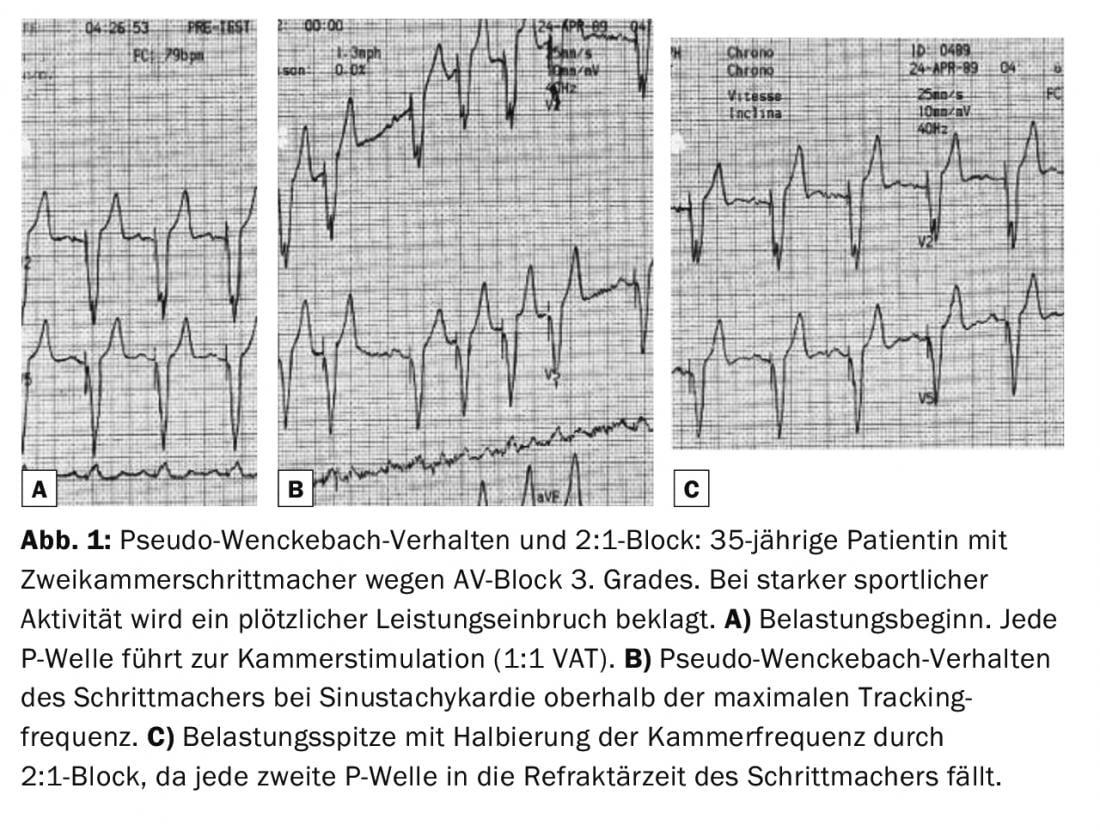
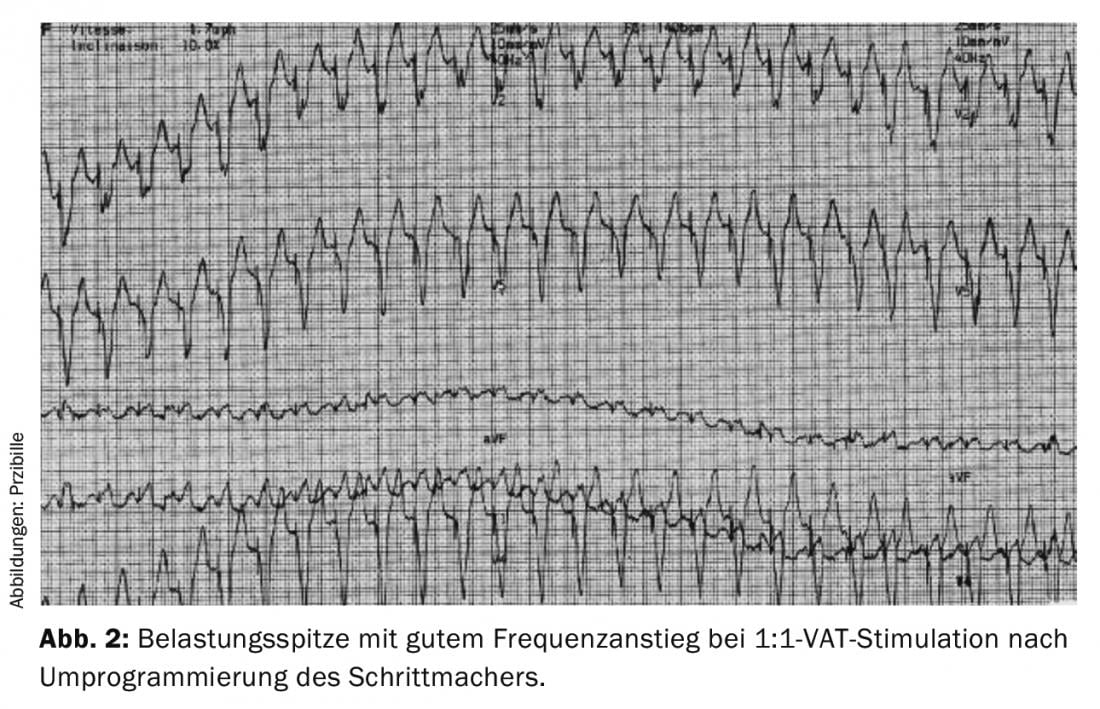
Many pacemaker systems operate in nominal programming with automatically adjusting refractory periods that shorten at higher frequencies. Rapid increases in frequency may overwhelm automatic adaptation and lead to loss of 1:1 VAT stimulation, resulting in palpitations or performance limitations. A fixed, short refractory period provides a remedy here.
Especially in patients with a diseased sinus node, the increase in heart rate under stress is disturbed (chronotropic incompetence). This may be a consequence of both impaired impulse formation in the sinus node and negative chronotropic medications (e.g., beta-blockers, antiarrhythmics). Patients with bradycardic atrial fibrillation also often have inadequate rate control during exercise. For these cases, the pacemakers are equipped with a sensor that allows a load-dependent increase of the heart rate (Fig. 3). In most units, the acceleration of the upper body is measured with an accelerometer and related to the extent of physical stress. Alternatively, respiratory time volume can be measured in terms of thoracic impedance changes. Both systems have different advantages and disadvantages. For example, the accelerometer responds more rapidly to changes in load; ergometer training, on the other hand, typically does not result in an increase in frequency due to the lack of acceleration of the upper body by the sensor control. In some pacemakers, both sensor technologies are combined to achieve the most physiological frequency matching possible. A third method of stress measurement is the determination of myocardial contraction dynamics. This is the only method that can also capture emotional stress.
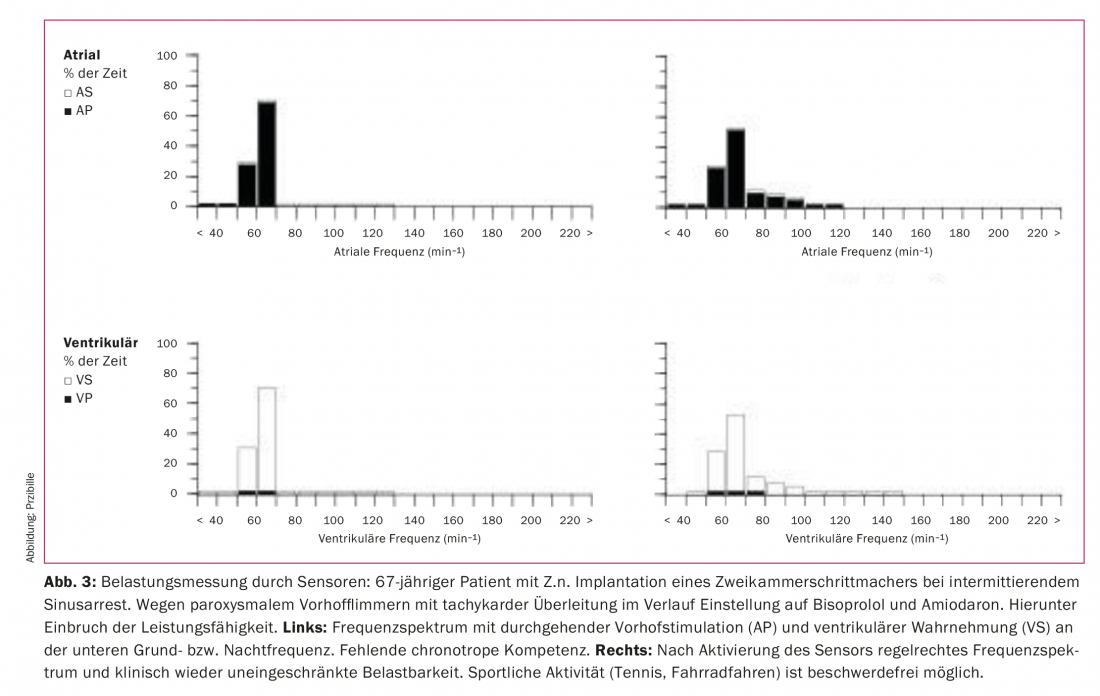
The majority of patients manage well with the standard setting or simple adjustments of the sensor function for everyday loads and sports activities. When programming the sensor, consider possible underlying cardiac disease (e.g., do not use frequencies that are too high in coronary artery disease that has not been completely revascularized). During intense sporting activity or when switching between sports that activate the sensor differently (e.g. cycling and swimming), fine adjustment of the sensor function may be required. Multiple reprogrammings may be required, and monitoring of heart rate and pacing by long-term ECG may be useful in some cases.
Mechanical limitations
In the first period after implantation, the affected side must be spared. Heavy loading may disrupt the formation of the connective tissue aggregate pocket and lead to pain, and the risk of electrode dislocation may be increased. After about six weeks, most sports can be practiced without restrictions. If jerky movements or strong stresses in the area of the pacemaker unit are to be expected, wait a little longer (e.g. volleyball, handball, goalkeeper in soccer).
In principle, damage to the system cannot be ruled out in ball sports where hard blows to the unit may occur (football, baseball); however, this is very rare in everyday life. Yes depending on the sport intensity, wearing a pad over the unit can be useful. Martial arts should be avoided because of the potential for repetitive force on the aggregate or electrodes [5,6]. If the patient wishes to participate in one-sided sports such as tennis, badminton, throwing sports or shooting (recoil), this should be discussed prior to surgery so that the pacemaker is implanted on the side that is not under stress.
Whether repeated mechanical stress in the shoulder girdle area increases the risk of an electrode defect cannot be answered in a generalized way. Systematic studies are not available; only case reports are found in the literature. On the one hand, the risk of electrode damage (“subclavian crush”) depends on the implantation technique: Insertion of the electrodes via the cephalic vein or a peripheral puncture in the area of the axillary vein may reduce the risk. On the other hand, individual anatomic tightness between the first rib and the clavicle may increase the risk of an electrode defect in this area. Due to only rare technical problems and the large interindividual variability, sports such as rowing, volleyball or golfing are also allowed for pacemaker wearers, at least for recreational purposes. However, patients should be informed of the increased stress on the electrodes. If necessary, shorter control intervals are useful. In individual cases, it may be necessary to advise against a certain sporting activity (type of sport or intensity of exercise, presence of an intrinsic rhythm in the case of pacemaker failure, electrode defects in the history).
Due to the pressure load, diving is a special challenge for pacemaker aggregates. Snorkeling is unproblematic, as all units can easily withstand water pressure down to a depth of two meters. In addition, the individual specifications of the manufacturers must be requested. Therefore, careful aggregate selection is necessary in divers prior to implantation.
Conclusion
Exercise has an important health-promoting or -maintaining function and can be practiced for almost all cardiac conditions. Even after implantation of a pacemaker, sport is possible in most cases. In order to minimize restrictions on sporting activity due to the pacemaker, some patient-specific or sport-specific factors must be taken into account. This already starts with the planning of the surgery (Tab. 1).
Take-Home Messages
- Pacemaker wearers without structural heart disease can participate in sports almost without restriction. However, sports with a high risk of impact should be avoided as a matter of principle.
- To enable high tracking frequencies, the AV and refractory time must be programmed to match the load.
- Patients with chronotropic incompetence or bradycardic atrial fibrillation benefit from sensors that adjust pacing frequency to current demand. Depending on the sensor, upper body movement, respiratory time volume or myocardial contraction dynamics are measured, for example.
- Sports should be avoided for the first six weeks post-op.
Literature:
- Schnohr P, et al: Dose of jogging and long-term mortality: the Copenhagen City Heart Study. J Am Coll Cardiol 2015; 65(5): 411-419.
- Lee DC, et al: Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol 2014; 64(5): 472-481.
- Institute for Quality Assurance and Transparency in Health Care (IQTIG), ed.
- Acquisition year 2016. Pacemaker implantation. Quality Indicators. Status 2017.
- Brignole M, et al.: 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: The Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 2013; 34(29): 2281-2329.
- Heidbüchel H, et al: Recommendations for participation in leisure-time physical activity and competitive sports in patients with arrhythmias and potentially arrhythmogenic conditions. Part I: Supraventricular arrhythmias and pacemakers. Eur J Cardiovasc Prev Rehabil 2006; 13(4): 475-484.
- Zipes DP, et al: Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 9: Arrhythmias and conduction defects. Circulation 2015; 132 (ahead of print).
CARDIOVASC 2018; 17(4): 17-20
HAUSARZT PRAXIS 2019; 14(8): 5-8











