At the Update Refresher General Internal Medicine, Michael Andor, MD, Center for Spine Medicine PRODORSO, Zurich, provided information on the current therapy of rheumatoid arthritis (RA). The treatment of RA has changed significantly in recent years thanks to new agents. For patients, the new treatment options mean less discomfort, higher quality of life and also an improved prognosis. However, side effects and costs of modern preparations are not insignificant.
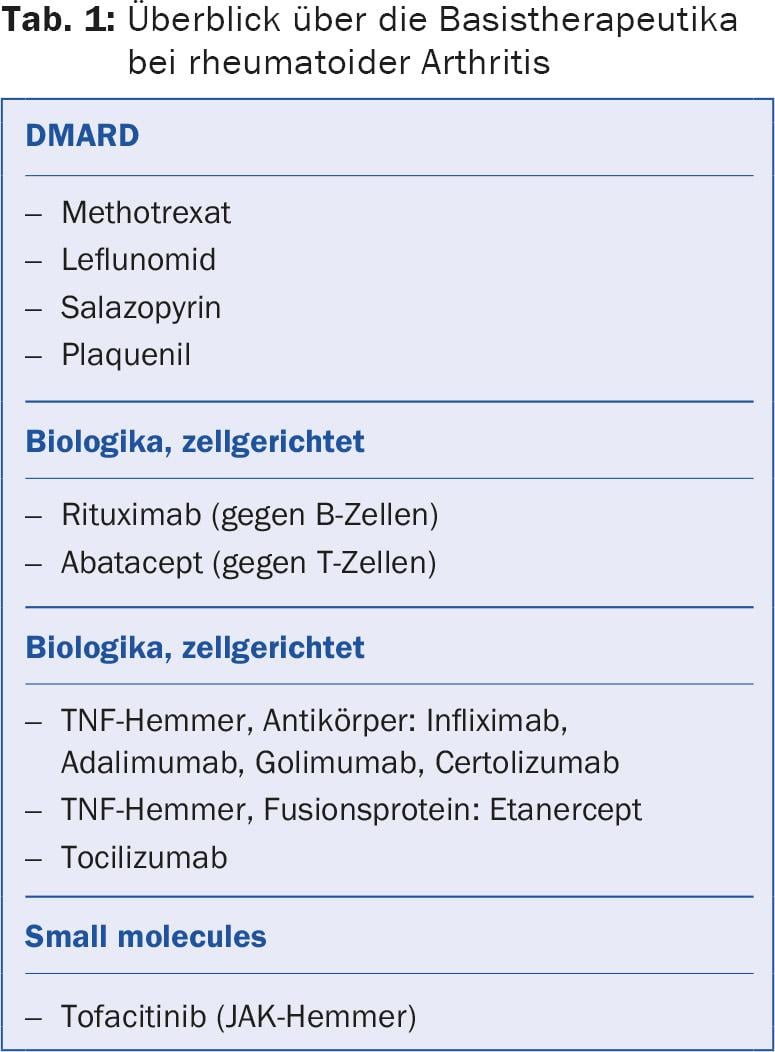
In RA, therapy is (almost) always initiated with methotrexate; alternatives are leflunomide and sulfasalazine. Patients on methotrexate treatment must come for regular blood checks. Side effects may also occur if the drug has been taken for years without any problems. The different biologics have different targets. If one doesn’t work (enough), it’s worth switching to another.
Patients usually respond very rapidly to the administration of TNF inhibitors, as evidenced by a rapid reduction in humoral inflammatory activity. The joint-destroying process is greatly slowed down. However, TNF inhibitors must be used with caution because they increase the risk of infection. For this reason, patients must be clarified for – possibly also inapparent – infections before starting therapy: Infectious anamnesis, tuberculosis screening, HIV and hepatitis screening, treatment of skin lesions, vaccinations according to the vaccination schedule, and dental cleanup.
Rituximab, Abatacept and Co.
The speaker presented the properties of some of the most important active ingredients:
Rituximab (MabThera®): The monoclonal antibody rituximab selectively destroys CD20-positive B cells. Even in patients who do not respond clinically to rituximab, radiographic progression of RA is significantly slowed. The drug is infused once a year at a dose of 1000 mg twice every two weeks (cost of two infusions about 10 000 Fr.). After six to twelve months, disease activity increases again due to B-cell regeneration, so infusions must be repeated.
Abatacept (Orencia®): Abatacept is a fusion molecule of CTLA-4 and an immunoglobulin and prevents T-cell activation. It is applied by monthly infusions (500-1000 mg), the effect is delayed, usually after six months. The combination with methotrexate improves the effect.
Tofacitinib (Xeljanz®): Tofacitinib is a small molecule that, unlike a protein, is not denatured. Tofacitinib is a reversible, competitive inhibitor of Janus kinase (JAK), which triggers immune and inflammatory responses. Tofacitinib is administered as a tablet at a dose of 2× 5 mg/d, which is more convenient for some patients than infusions. “However, many patients find swallowing pills daily more troublesome than getting a monthly or even less frequent shot,” the speaker mentioned.
Intensive therapy, frequent controls
The goal of any basic therapy in RA is to achieve early remission or remission of the disease. to achieve the lowest possible disease activity. The motto is “treat to target”: The success of treatment is not only defined clinically and by the subjective feeling of the patient, but also measured with exact scores, e.g. with the “Disease Activity Score 28” (DAS28). If no remission can be achieved by therapy, treatment is adjusted after three months at the latest – taking into account the patient’s individual situation and risk profile (contraindications). Rapid start of treatment, intensity and control intervals are more important than the choice of drug. “In principle, it doesn’t matter what you treat with, but treat quickly and treat well,” Dr. Andor said.
During treatment, the patient is monitored regularly and disease activity is assessed by objective parameters (laboratory values, ultrasound, X-ray) and the patient’s subjective feelings. Intensive treatment with monthly consultations and rapid adjustment of therapy can achieve better disease control in most patients.
In the acute disease flare-up, steroids can bridge the time until the biologics take effect after a few months. However, Dr. Andor recommended that, as a primary care physician, steroids should not be prescribed if possible, so that the rheumatologist can still see and evaluate the patient in the condition without steroid treatment.
Source: Update Refresher General Internal Medicine, November 5, 2015, Zurich
HAUSARZT PRAXIS 2016; 11(1): 48-49











