With the adapted guidelines of the International Atherosclerosis Society (IAS), the Working Group Lipids and Atherosclerosis of the Swiss Society of Cardiology (AGLA) has found a compromise for risk assessment, prevention and treatment. The biggest challenge continues to be the high number of high-risk patients in whom LDL target levels are not achieved
The Lipids and Atherosclerosis Working Group of the Swiss Society of Cardiology (AGLA) considers both the International Atherosclerosis Society (IAS) Guidelines and the joint European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) Guidelines in its 2012 recommendations on atherosclerosis prevention. In both cases, the high-risk categories were modified slightly. Analogous to the ESC/EAS guidelines, the AGLA proposes risk stratification into four categories.
- The highest category is assigned to individuals with manifest CHD/atherosclerosis, diabetes mellitus type-2 or -1 with end-organ damage, and chronic renal insufficiency.
- Individuals with multiple risk factors are particularly at high risk.
- In addition, there are two other categories: intermediate and mild.
An important difference between the ESC/EAS and AGLA scores concerns risk assessment. While the ESC/EAS calculate the absolute risk of mortality within 10 years, the AGLA algorithm calculates the 10-year risk of occurrence of a fatal or nonfatal coronary event. The latter results in higher risk values.
In the absence of epidemiological data in Switzerland, the AGLA risk calculator is based on the IAS PROCAM algorithm for low-risk countries. These include Germany, among others. However, cardiovascular risk already varies within Switzerland and is significantly lower than in Germany. For this reason, the PROCAM score for Switzerland was calibrated with a factor of 0.7. Another difference concerns the LDL target values. For example, the AGLA recommends an LDL cholesterol of 1.8 mmol/l for high-risk patients. The remaining target values range from <2.6 mmol/l to <4.1 mmol/l depending on the risk category according to IAS/AGLA.
A new edition of the AGLA recommendations on atherosclerosis prevention is already planned for next year. The definition of a general LDL threshold is under discussion in primary prevention. This would replace the group-specific target values. Alternatively, the currently calculated 10-year risk could be replaced by the lifetime risk calculation. “In addition, the current classification of chronic kidney disease should be taken into account in the newly issued guidelines,” said Prof. Arnold von Eckardstein, MD, president of the AGLA, at the joint annual meeting of the Swiss Societies of Cardiology (SGK) and Cardiothoracic Vascular Surgery in Lugano. For the development of his own algorithms, he hopes to use data from the two large Swiss observational studies SAPALDIA and “Cohorte Lausannoise” (CoLaus).
Women and smokers inadequately treated
Scientific arguments for the use of the AGLA algorithm were provided by the CoLaus cohort [1]. Nanchen et al. (2009) calculated the 10-year risk of CHD in the observed 5683 men and women aged 35 to 75 years. Subsequently, the ESC, IAS (PROCAM), and US National Cholesterol Education Program Adult Treatment Panel III (Framingham) scores were used to determine how many subjects were indicated for primary prevention. This showed that more subjects were assigned to the high-risk category by using the ESC score(Fig. 1).
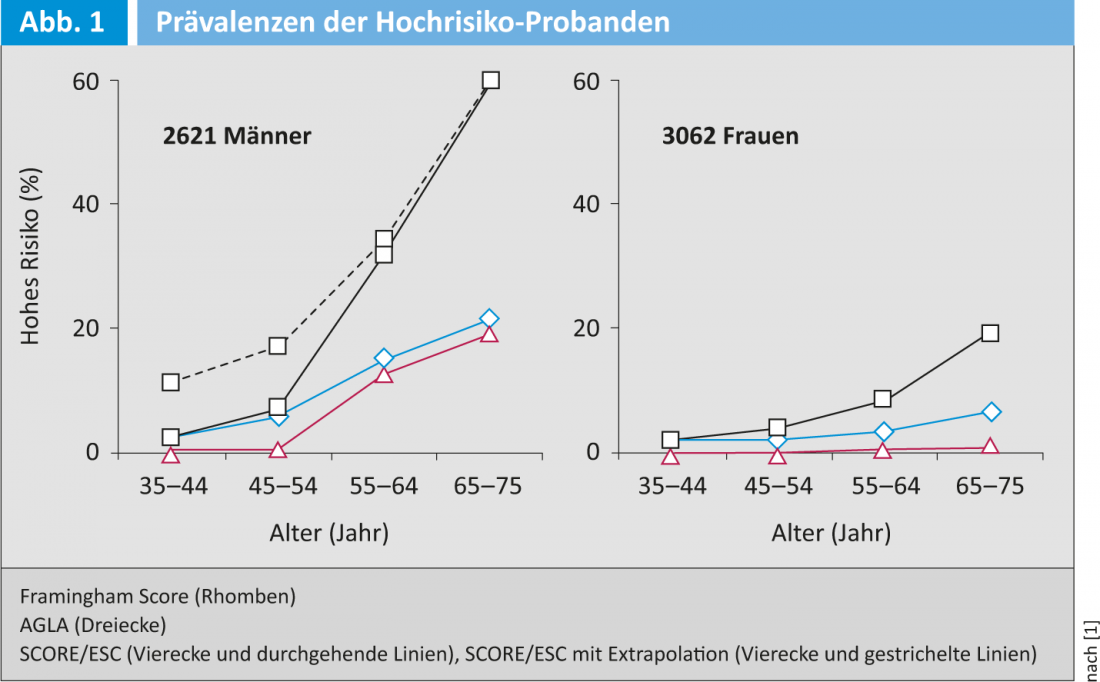
The remaining scores also identified younger patients with fewer risk factors.
“The strategy favored by the IAS/AGLA leads to a higher NNT and generates correspondingly higher costs,” Prof. von Eckardstein said. Since most events occur in the intermediate-risk group and the cost of statins decreases, this is a defensible strategy, he said.
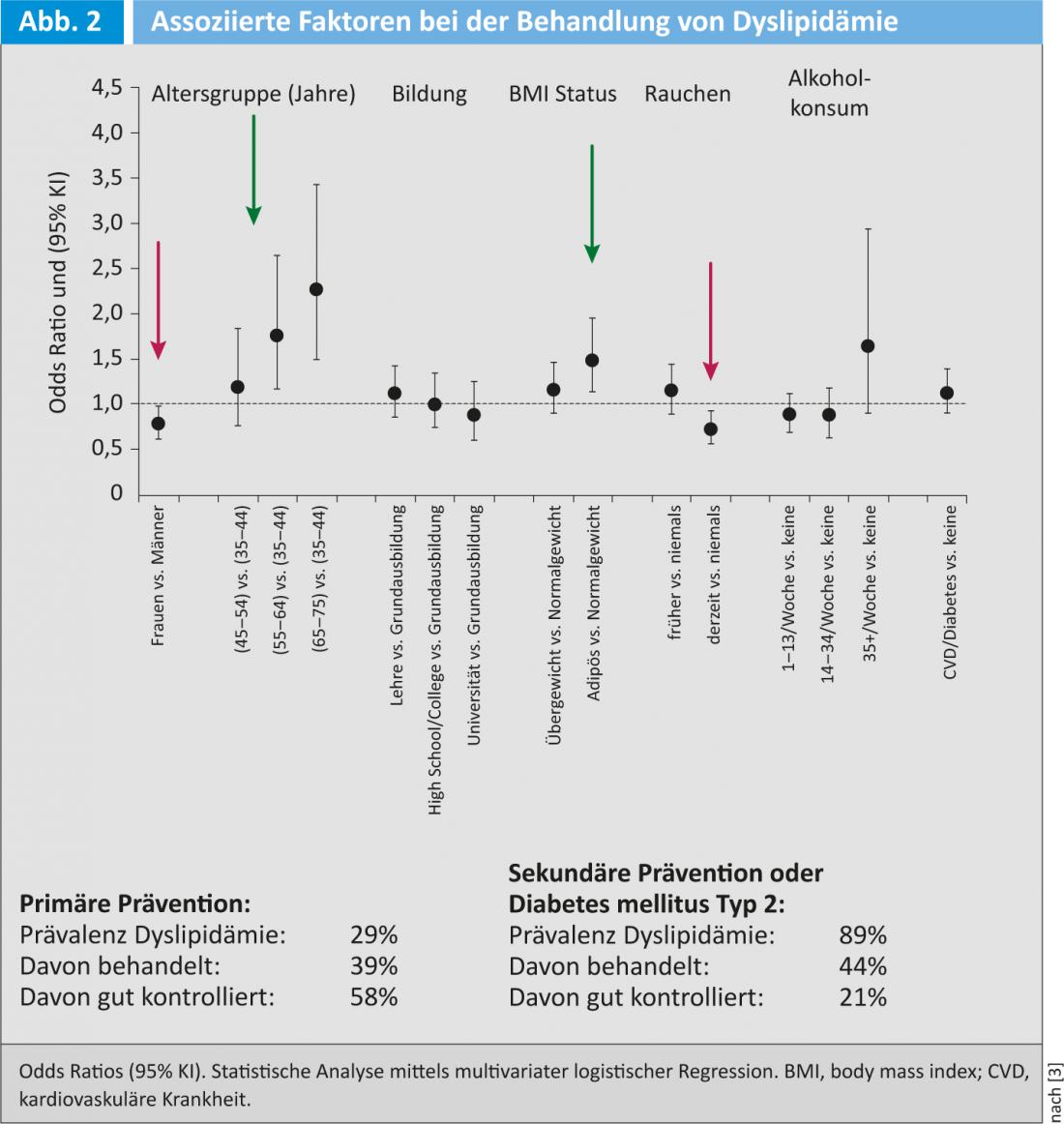
As the evaluation of hits on the AGLA website show, the adapted IAS/AGLA risk calculator is used significantly more often than the EAS/ESC risk calculator, which is also available on the website. Nevertheless, implementation in practice leaves much to be desired. In a study by Jaussi et al. (2010) showed a large discrepancy between clinical risk assessment and systematic risk calculation [2]. Even when physicians were specially trained, they trusted their clinical judgment rather than the calculated 10-year risk of cardiovascular disease. With the result that an estimated one-fifth of low-risk patients and about one-third of high-risk patients were not adequately treated. Even in the CoLaus cohort, more than 60% of high-risk patients did not reach the LDL target of 2.6 mmol/l [3]. “The best prospects for adequate LDL treatment are older people and those with a high BMI,” Prof. von Eckardstein said. Characteristics associated with undertreatment were female sex and smoking (Fig. 2).
Literature list at the publisher
Source: Joint Annual Meeting of the Swiss Society of Cardiology (SGK) and the Swiss Society for Cardiac and Thoracic Vascular Surgery (SGHC), June 12-14, 2013, Lugano.











