In clinical practice, it has become apparent that the previously used subtype classification inadequately reflects the collective of patients with rosacea. This is because different symptoms often overlap and the transitions are fluid. This is better reflected in the phenotype-based approach with important implications for targeted treatment. In addition to the appropriate active substance, therapy adherence and patient expectations are also decisive factors. Visible treatment success often only appears after a few months.
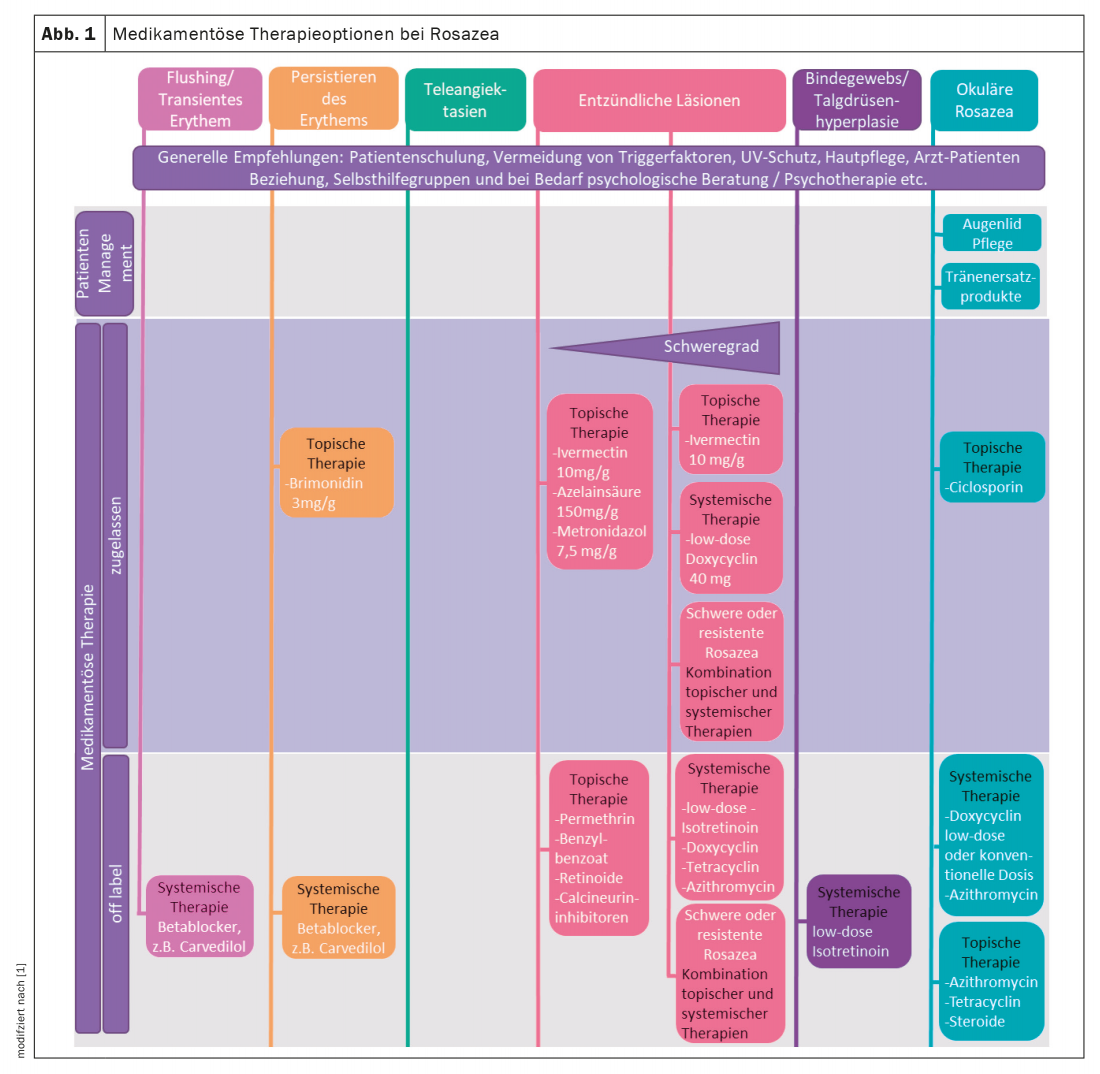
Characteristic symptoms of rosacea are transient or persistent erythema with telangiectasia; later in the course, papules and pustules often form and lymphedema may occur. In addition, plaques, skin dryness, phyme of the facial aces, and ocular involvement may occur. Rosacea patients also suffer from symptoms such as burning, tightening, stinging and a feeling of heat [1]. Since the subtype classification (erythema, papulopustular, phyma, ocular) commonly used until a few years ago does not sufficiently reflect the manifestations observed in practice, the ROSCO panel (ROSazea COsensus) has proposed a phenotype-based diagnosis instead [2–4]. It is true that there are patients who show only erythema or telangiectasia or exclusively papules or pustules. “But much more common is an overlap of these symptoms,” explained Prof. Martin Schaller, MD, University Dermatology Clinic, Tübingen (D) [5]. Several clinical signs often coexist. Against the background of these findings, national and international experts have defined a phenotype-based therapy algorithm, which at its core propagates a symptom-oriented treatment approach. This is described in detail, for example, in the updated version of the s2k guideline published in 2022 [1]. The spectrum of drug treatment options includes topical preparations and system therapies, with combination therapies also being possible, especially in severe cases (Fig. 1, box) . The speaker points out that it often takes a long time before a successful therapy becomes apparent. “Rosacea therapy is a marathon,” said Prof. Schaller, explaining, “You have to treat for months to lead patients to therapeutic success” [5]. It is important to educate patients about this in advance of therapy, he said.
Counteract papules, pustules and erythema with topicals
Metronidazole is among the most commonly used topical therapeutic agents for rosacea [1]. This antibiotic and antiparasitic substance has been shown to reduce inflammatory papules and pustules. The topical vasoconstrictor brimonidine (0.33% gel) is recommended for the treatment of persistent centrofacial erythema. Brimonidine is a highly selective alpha-2-adrenergic receptor agonist. In the facial skin of rosacea patients, its direct vasoconstrictive activity leads to a strong, passive constriction of the dilated dermal arterioles, resulting in a fading of the erythema. This effect begins as early as 20-30 minutes after topical application of a 0.33% brimonidine gel, reaches its maximum after 3-6 hours, and lasts for a total of 8-10 hours [1]. As the binding of brimonidine to the alpha-2 receptor subsides and the substance is degraded, vasodilation resumes and erythema returns. Efficacy and tolerability were confirmed in two randomized, controlled parallel clinical trials and one long-term study [6–8]. Brimonidine has an anti-inflammatory component of action in addition to the vasoconstrictive component [9].
Beta-blockers: effective against additional flushing
Carvedilol is a nonselective β-receptor blocker with α1-antagonistic activity that may be considered for systemic therapy of persistent erythema and flushing symptoms in rosacea. The effect is based on several factors. Blockade of β-adrenergic receptors in smooth muscle of cutaneous blood vessels results in vasoconstriction. Anxiety and tachycardia, which can trigger an exacerbation of flushing symptoms, are also attenuated. Carvedilol also has antioxidant and anti-inflammatory properties. The standard dose is 2× 25 mg daily [5]. For persistent erythema, 6.25 mg twice daily gradually, then up to 12.5 mg three times. “In many patients, you see a significant improvement after 2-3 weeks,” said Prof. Schaller [5].
| Topical or systemic treatment or both? According to the guideline, topical therapy is sufficient in many cases for the treatment of transient or persistent erythema as well as papules and pustules of mild to moderate severity [1]. However, the severe, highly inflammatory forms of rosacea are also treated topically in combination with systemic therapies. For topical rosacea treatment, evidence is available for drugs containing metronidazole (gel, cream), brimonidine gel, and ivermectin cream based on randomized, vehicle-controlled, double-blind trials or head-to-head studies [11]. Other topicals are used off-label for rosacea, including azelaic acid in Switzerland. The choice of the particular agent and its concentration is made individually according to the phenotypic features of rosacea present in each case, as well as the acute nature of the disease and the patient’s skin type [1]. In severe, highly inflammatory forms, topical therapy is combined with systemic treatment [1]. |
With isotretinoin, be sure to use a low dosage
In several studies, the vitamin A acid derivative isotretinoin was shown to improve rosacea [1]. It is important to use a low dosage. In contrast to the usual dosage of 0.5-1.0 mg/kg body weight (bw) per day, a lower dose such as 10-20 mg daily can be successfully treated with a much lower side effect profile. Prof. Schaller has had very good experience with 10 mg isotretinoin daily; depending on the course, the dosage interval could be extended to every second or third day [5]. Patients with extrafacial rosacea or with a granulomatous component also respond very well to this treatment. In ocular rosacea, low-dose isotretinoin therapy of 10 mg daily is not contraindicated but often results in improvement of ocular symptoms. In patients with Morbihan’s disease, the combination of low-dose isotretinoin (10 mg/d) with an antihistamine (e.g., desloratadine 5 mg/d) has been shown to be effective – but patients should be informed that this is a prolonged therapy. However, experience shows that symptoms improve significantly after 1-2 years of treatment. Why isotretinoin is an off-label therapy despite good evidence is explained by the fact that isotretinoin-induced dermatitis occurred in pivotal studies at a high dose and this was interpreted as a worsening of rosacea, the speaker explained [5].
Azithromycin may be considered on a secondary basis
The level of evidence on azithromycin in rosacea is rated low in a Cochrane review, but especially in cases of intolerance to tetracyclines or contraindications, azithromycin is one of the macrolides that can be switched to [1,10]. Prof. Schaller has also had good experience in patients with rosacea fulminans, a very debilitating form of rosacea [5]. Azithromycin is a macrolide with a potent anti-inflammatory effect and a long half-life of 2-4 days. After oral administration, it is rapidly absorbed into the circulation, stored in the intracellular space, and slowly released from there. Prof. Schaller recommends a dosage of 500 mg 3×/week for four weeks, followed by 2×/week and 1×/week, respectively, for four additional weeks [5]. If necessary, maintenance therapy of once-weekly azithromycin administration can also be performed.
Also target relief of invisible symptoms
Not only visible clinical manifestations of rosacea, but also the invisible symptoms can lead to a high level of suffering. “Patients often also have stinging, burning, dryness, and itching,” said Prof. Schaller [5]. In a study of 25 rosacea patients, treatment with ivermectin cream was shown to significantly alleviate these subjectively perceived symptoms. At baseline, 50% of patients had moderate or severe stinging and burning; at week 16, 80% were free of appearance. Similar results were seen for dryness and itching.
Congress: Inflammation Update Lübeck
Literature:
- S2k guideline: “Rosacea”, 2022, AWMF register number 013-065.
- Wilkin J, et al: Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol 2002; 46: 584-587.
- Tan J, et al: Updating the diagnosis, classification and assessment of rosacea: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol 2017; 176(2): 431-438.
- Schaller M, et al: Recommendations for rosacea diagnosis, classification and management: update from the global ROSacea COnsensus 2019 panel. Br J Dermatol 2020; 182(5): 1269-1276.
- “Diagnostic criteria, classification and therapy algorithm of rosacea”, Prof. Dr. med. Martin Schaller, Inflammation Update Lübeck, 05.03.2022.
- Fowler J, et al: Once-daily topical brimonidine tartrate gel 0.5% is a novel treatment for moderate to severe facial erythema of rosacea: results of two multicentre, randomized and vehicle-controlled studies. Br J Dermatol 2012; 166(3): 633-641.
- Fowler J, Jr, et al: Efficacy and safety of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of two randomized, double-blind, and vehicle-controlled pivotal studies. J Drugs Dermatol 2013; 12(6): 650-656.
- Moore A, et al: Long-term safety and efficacy of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of a 1-year open-label study. J Drugs Dermatol 2014; 13(1): 56-61.
- Piwnica D, et al: Vasoconstriction and anti-inflammatory properties of the selective α-adrenergic receptor agonist brimonidine. J Dermatol Sci 2014; 75(1): 49-54.
- van Zuuren EJ, et al: Interventions for rosacea. Cochrane Database Syst Rev 2015; 2015(4): Cd003262.
- Gollnick H, et al: Systemic isotretinoin in the treatment of rosacea – doxycycline- and placebo-controlled, randomized clinical study. JDDG 2010; 8(7): 505-515.
- Schaller M, et al: Rosacea management: Update on general measures and topical treatment options. JDDG 2016; 14 Suppl 6: 17-27.
DERMATOLOGIE PRAXIS 2022; 32(4): 46-48