Psoriasis is a very heterogeneous clinical picture that requires differentiated care, not least because of its chronicity and the high degree of suffering. As a systemic disease, not only the skin, but also nails and joints can be involved. Effective diagnostics are therefore essential to guide patients with high inflammatory pressures to effective and targeted therapy.
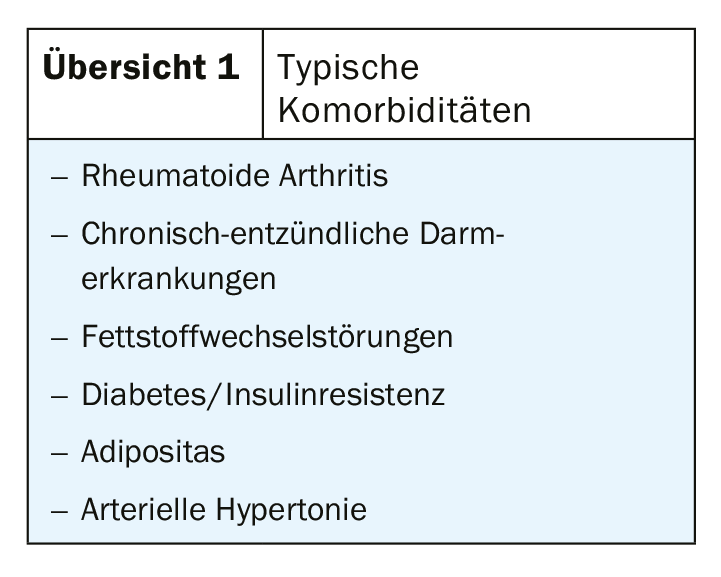
Psoriasis is one of the most common chronic diseases of the skin. In Switzerland, approximately 150,000 people are affected. However, the systemic disease not only affects the skin, but may also involve the nails and/or joints and entails other characteristic comorbidities (overview 1). The chronic inflammatory disease is caused by a disorder of the body’s immune system. Key roles are played by pro-inflammatory proteins, overactivity of Th1 lymphocytes, and various cytokines, such as tumor necrosis factor-alpha (TNF-alpha) and the pro-inflammatory interleukins-12 and -23, as well as interleukin-17. The skin reacts with an inflammatory response and the keratinocytes divide more rapidly. However, in addition to a genetic predisposition, a number of other factors are required to trigger the disease (overview 2).
Heterogeneous appearance
With 85-90%, psoriasis vulgaris or plaque psoriasis is the most common. Sharply demarcated, reddish, slightly raised plaques covered with silvery-white scales are typical. These occur because the skin of those affected does not renew itself every 28 days, but at a much faster rate of every three to five days. As a rule, the plaques can be localized mainly on the extensor sides of the elbows and knees, in the sacral region and or on the scalp. However, they can eventually affect any area of the body. Often, psoriasis runs a chronic to progressive course over many years or occurs in acute attacks. Especially infections, stress or certain medications can influence the manifestation.

In addition to psoriasis vulgaris, there are other forms of manifestation. Guttate psoriasis is a more acute form with small lesions. It can occur especially in children and adolescents after a streptococcal infection and develop into psoriasis vulgaris. In psoriasis intertriginosa/psoriasis inversa, the inflammatory foci additionally occur in the body folds. When the entire skin is affected, it is called psoriatic erythroderma. This rare form is often associated with complications that require hospitalization. In addition, there are still different pustular manifestations. They are all characterized by sterile pustules. These may appear on the palms of the hands or soles of the feet.
Nail psoriasis and psoriatic arthritis
With all forms of the disease, the nails can also be affected. Nearly every second psoriasis patient has nail involvement, which is difficult to treat. Stippled nails, onychodystrophy, oil spots, or subungual hyperkeratosis are typical. Not only are these nail changes associated with severe disease progression and often stigmatize patients, they are also a predictor of joint involvement. Up to 80% of patients with psoriatic arthritis (PSA) have nail involvement. A PSA is suffered by 20-30% of all psoriatic patients. Half of them show erosive joint changes, which can often be detected within ten months to two years after diagnosis. Not least for this reason, rapid and early diagnosis is indicated.
Skin lesions do not equal severity
Different parameters should be used to determine the severity. Even patients with only a few skin lesions can still be severely affected. Especially if the nails, face or genital region are affected. Therefore, in addition to assessing skin involvement by PASI or BSA, the localization of lesions and individual quality of life must also be evaluated. The BSA (Body Surface Area) indicates the percentage of the body surface area affected. One palm reflects one percent of the body surface. For the Psoriasis Area and Severity Index (PASI), the four body regions of head, arms, trunk and legs are considered. Three symptoms are assessed for each body region: the intensity of redness (erythema), the intensity of thickening of the skin (infiltration), and the intensity of scaling, each on a scale of 0 to 4. The estimation of the affected body surface is made on a scale of 0 (not affected) to 6 (completely affected).
Topical or systemic – which therapy is effective?
Basic therapy with drug-free ointment bases or topical preparations of urea and salicylic acid is essential for all forms of the disease. Thereafter, further treatment decision is made based on the severity.
Mild psoriasis is well advised with topical therapy. The gold standard is topical vitamin D3, topical steroids, or a combination of cortisone and vitamin D3.
Moderate to severe psoriasis is usually treated systemically. In the first instance, ciclosporin, fumaric acid esters, methotrexate and retinoids are available here in addition to phototherapy.
Therapy goal – appearance-free skin appearance
A biologic may be used for treatment when first-line therapy has not achieved adequate therapeutic success and in cases of intolerance or contraindications to conventional systemic therapeutics. In this case, for example, a TNF-alpha antagonist such as adalimumab, etanercept, certolizumab, and infliximab, an interleukin-17A inhibitor such as secukinuab, brodalumab, and ixekizumab, or the monoclonal antibody ustekinumab directed against interleukin-12 and -23 can be resorted to. With guselkumab, risankizumab and tildrakizumab, pure IL-23 blockers are available that stand out as the safest biologics with high efficacy and no loss of effect over time.
Which systemic therapeutic agent ends up being used should be individualized to the patient. For this purpose, concomitant diseases and concomitant medication must also be taken into account. Ultimately, the clinical criteria must be weighed against the drug profile and patient characteristics in order to initiate treatment that is effective for the individual.
Further reading:
- www.beobachter.ch/gesundheit/krankheit/schuppenflechte-psoriasis (last accessed on 15.01.2020)
- Augustin M, Reich K, Blome C et al. Nail Psoriasis in Germany: Epidemiology and Burden of Disease. Br J Dermatol 2010; 163: 580-585.
- Reich K, Krüger K, Mössner R, Augustin M: Epidemiology and clinical pattern of psoriatic arthritis in Germany: a prospective interdisciplinary epidemiological study of 1511 patients with plaque-type psoriasis. Br J Dermatol 2009; 160(5): 1040-1047.
- Radtke MA, Mrowietz U, Feuerhahn J, et al: Early detection of comorbidity in psoriasis: recommendations of the National Conference on Healthcare in Psoriasis. J Dtsch Dermatol Ges. 2015; 13(7): 674-689.
- Thaçi D, Augustin M, Krutmann J, Luger T: Importance of basic therapy in psoriasis. J Dtsch Dermatol Ges. 2015; 13(5): 415-418.
HAUSARZT PRAXIS 2020; 15(3): 43-44