The most important risk factors for age-related macular degeneration (AMD) are age and smoking. Cardinal symptoms of AMD are a decrease in reading ability, metamorphopsia, and small scotomas. Complete blindness is rare because the patient’s visual field is preserved. The most important diagnostic measure in suspected cases is optical coherence tomography (OCT). In wet AMD, VEGF injection treatment can improve visual acuity by nearly 20% over two years in more than 80% of patients. Other important measures are a good supply of optical aids and comprehensive counseling (counseling centers for the visually impaired).
Demographic changes in industrialized countries are leading to a sharp increase in age-related diseases. In ophthalmology, this is especially true for cataract and age-related macular degeneration (AMD). Both diseases are on their way to become true widespread diseases: It is estimated that about 60,000 cataract surgeries are performed annually in Switzerland and about 200,000 people are affected by AMD. Accordingly, the primary care physician is also increasingly confronted with questions from these areas.
Risk factors for AMD
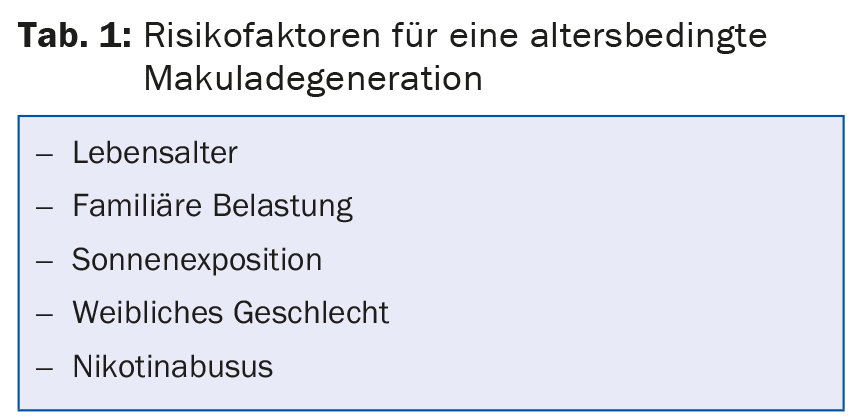
The most important risk factor for AMD is age. It is estimated that about 35% of 75- to 84-year-olds are affected by an early form and about 5% by a late form of AMD. Other risk factors are summarized in Table 1 . Strongest preventable risk factor with a relative risk >2 is nicotine abuse, but questionable is the advice to patients over 80 years of age to quit smoking to reduce the risk of AMD.
Clinical image
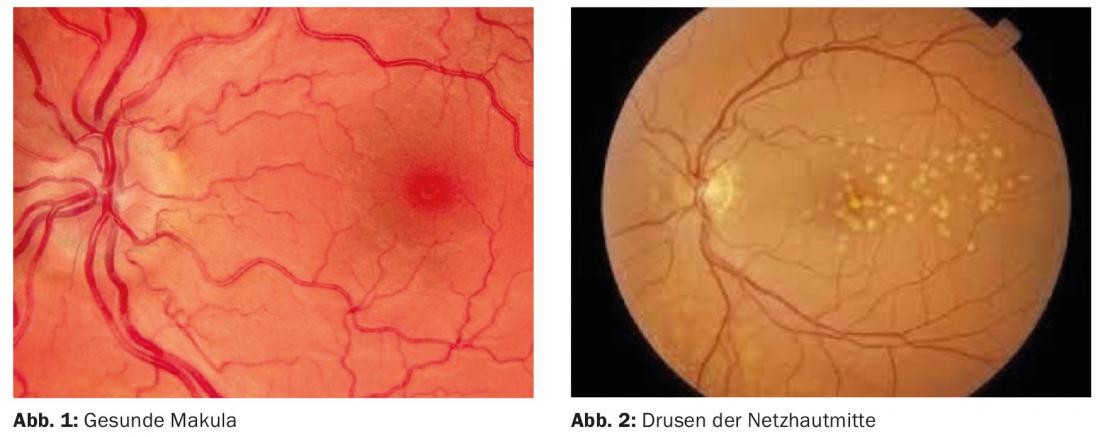
The macula, the region of the retina with the highest density of photoreceptors, is responsible for central visual acuity, i.e. the actual visual acuity, this in contrast to the visual field, the performance of which is provided by the peripheral retina and mainly serves orientation (Fig. 1).
Basically, two forms of AMD are distinguished, the dry and the wet form. In the dry form of AMD, on the one hand, metabolic products from the energy-intensive visual process accumulate in so-called drusen (Fig. 2), and on the other hand, the pigment epithelium and thus the embedded photoreceptors perish, the so-called areolar atrophy. These two pathomechanisms run concurrently and may merge.
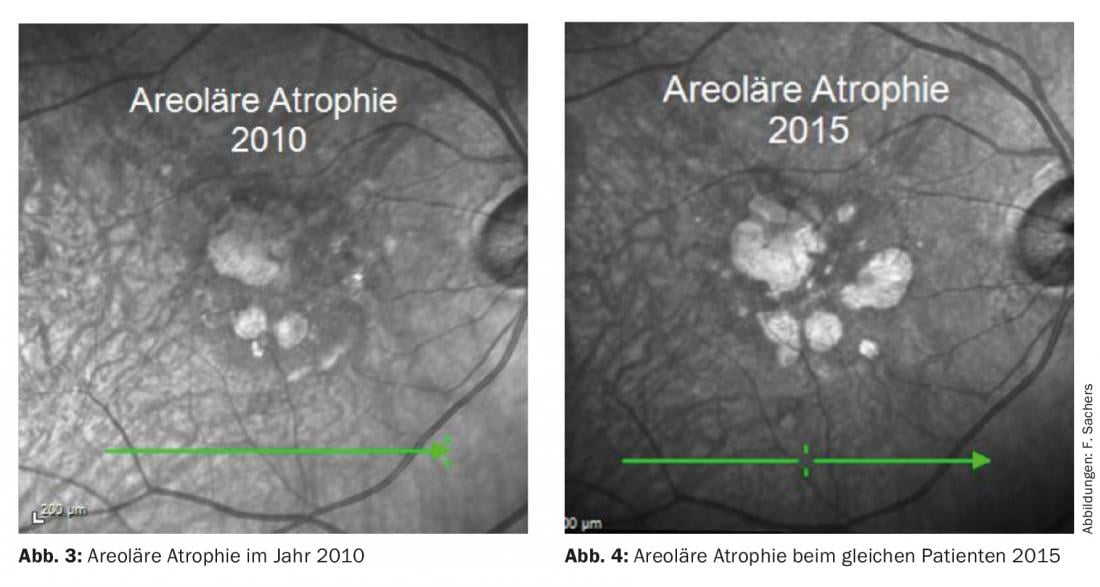
The progression of these processes is slow over years, initially mostly asymptomatic (Fig. 3 and 4). The majority of AMD patients (85%) have a dry form.
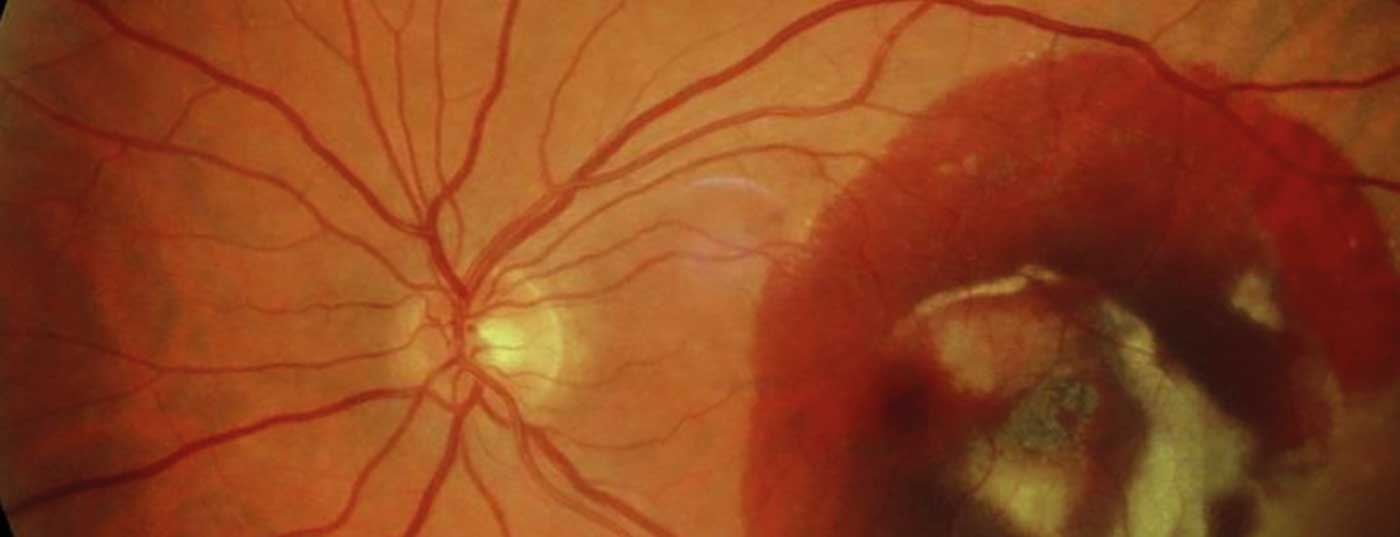
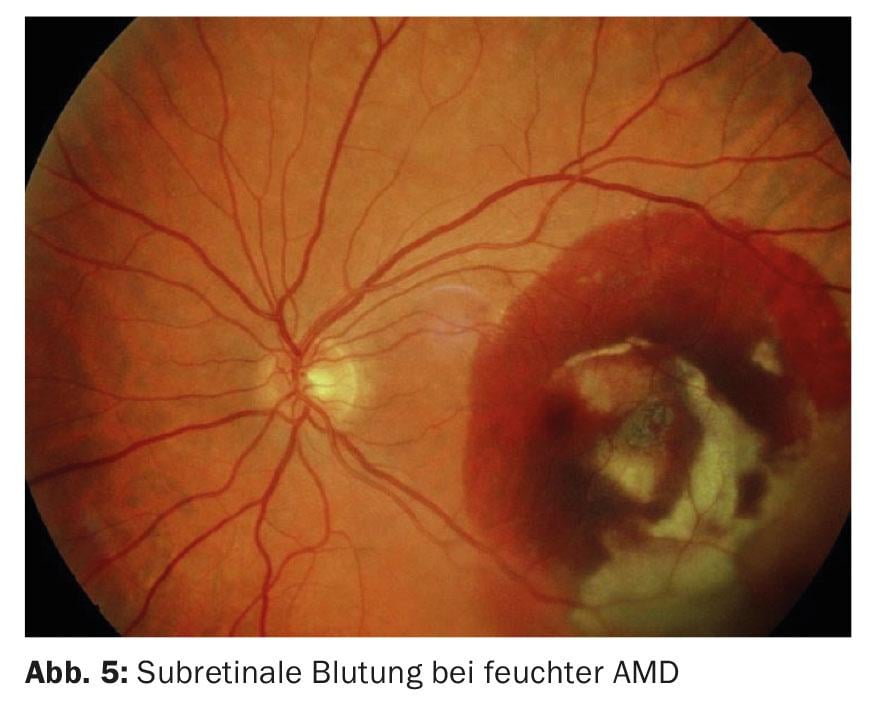
More acute and at the same time less frequent – but responsible for most severe forms of AMD – is wet AMD. This results in the formation of subretinal neovascularizations (SRN) from the choriocapillaris, which sprout inside or below the retina, lose serous fluid and blood, and ultimately lead to large so-called fibrovascular scars of the retinal center (Fig. 5). This almost inevitably results in loss of reading ability. Nearly half of all patients with wet AMD in one eye also develop AMD in the other eye within five years.
Symptoms
Cardinal symptoms of AMD are a decrease in reading ability, metamorphopsia – straight lines or letters that are perceived as crooked – and small image deficits (scotomas). Initially, these are hardly noticed, but lead to a significant deterioration in reading ability as well as an increased need for light. Ultimately, AMD ends in total reading disability or central visual acuity below 0.05 in advanced forms. Complete blindness due to AMD is very rare, because the peripheral visual field is usually preserved, so that the patient’s ability to orientate independently is almost always guaranteed.
Diagnostic possibilities
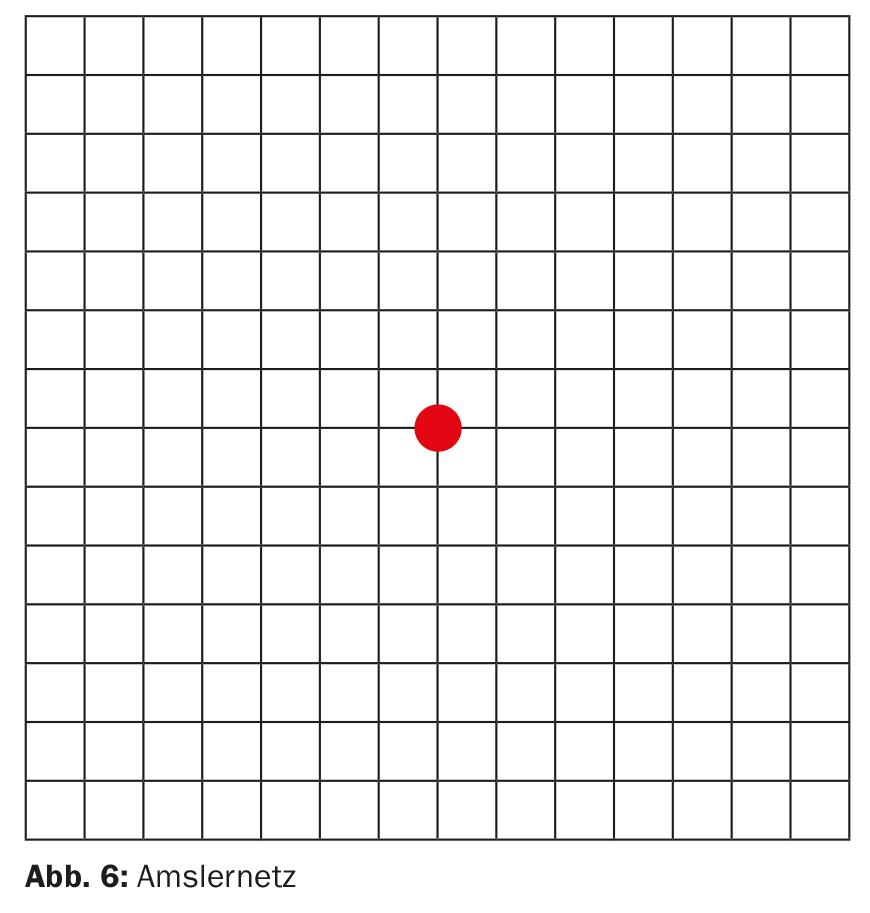
As a screening examination in the asymptomatic patient, the side-separated examination of the central 10° of the visual field with the Amsler net for metamorphopsia is well suited, also in internal medicine practice. (Fig.6). In addition to the obligatory measurement of best-corrected near and distance visual acuity, further diagnostic procedures include clinical examination of the retina with dilated pupil and, in suspected cases, optical coherence tomography (OCT) and/or fluorescence angiography.
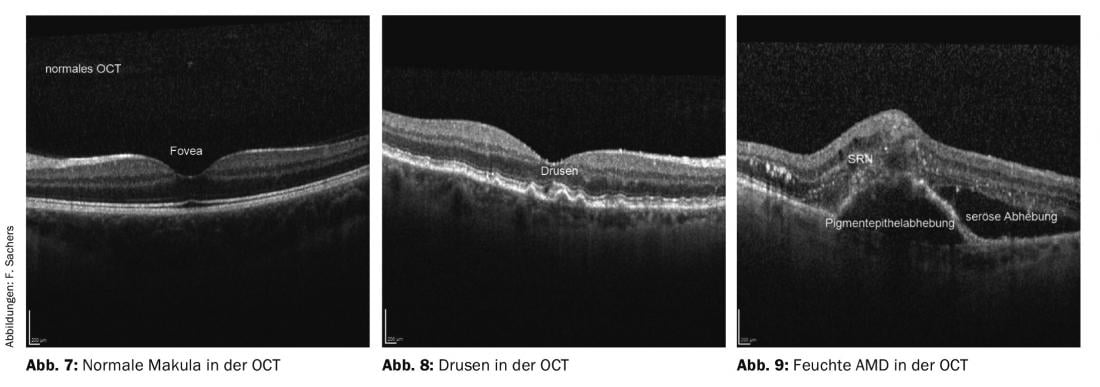
OCT has revolutionized retinological diagnostics. With noninvasive laser scanning technology, it is possible to create optical cross-sectional images of the retina that allow very precise diagnosis of various macular diseases (Figs. 7, 8 and 9) . Fluorescein angiography, which was previously necessary to confirm the diagnosis of wet AMD, needs to be used significantly less frequently. To establish the indication for a necessary intravitreal injection treatment, an OCT is mandatory.
Therapy of dry AMD
Therapeutic options for the dry form of AMD are extremely limited and are currently reduced to monitoring to rule out conversion to the wet form. The benefit of dietary supplementation with lutein, zeaxanthin, omega-3 fatty acids, and vitamins C and E to slow progression is extremely limited. Very important is the optimal supply of magnifying vision aids.
Therapy of wet AMD
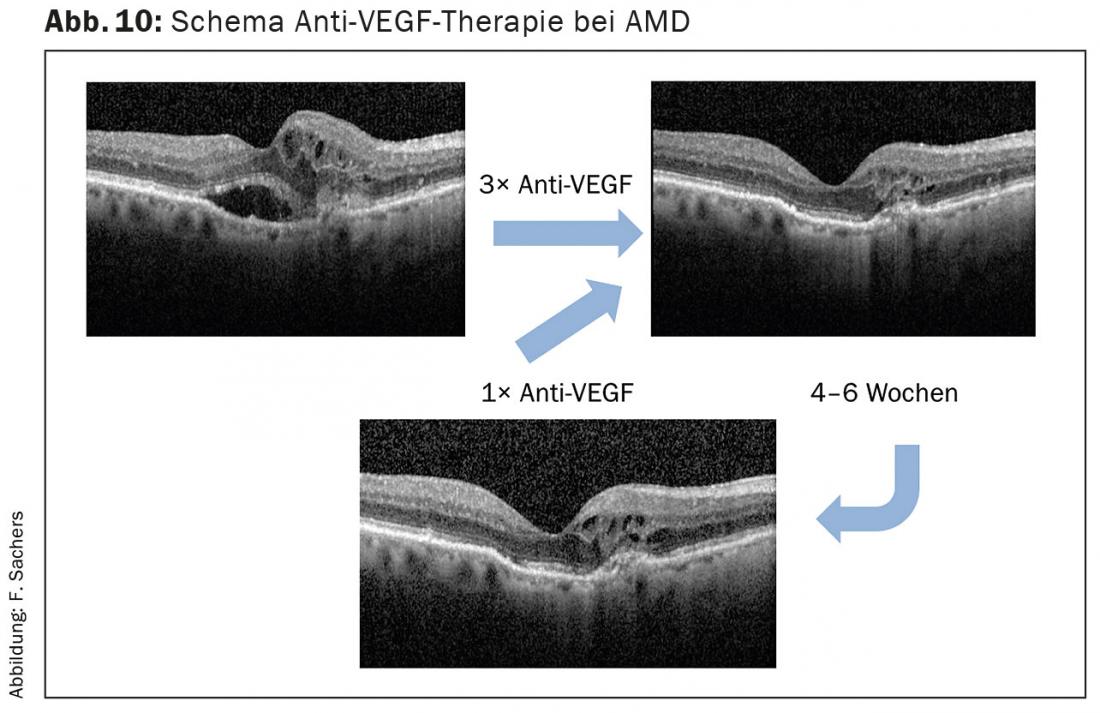
The introduction of intravitreal injection treatment with “Anti-Vascular Endothelial Growth Factor” (VEGF) agents revolutionized the treatment of wet AMD in 2005. The substances currently used are ranibizumab, bevacizumab and aflibercept. The therapeutic principle is based on the temporary blockade of the VEGF receptor at the subretinal neovascularization membrane, which thereby regresses. As a result, there is resorption of existing fluid exudation and hemorrhage, associated with visual stabilization or improvement. However, this effect is limited in time and must be maintained by regular injections.
The timing of re-injection is either based on signs of activity of AMD diagnosed by OCT or follows the “treat and extend” regimen at defined time intervals (Fig. 10). With consistent injection treatment, more than 80% of patients are able to maintain a visual acuity improvement of nearly 20% over two years – a massive improvement in prognosis over the spontaneous course.
To avoid bacterial endophthalmitis as the most severe complication, the injection is performed under highly sterile conditions in the operating room. The infection rate under these circumstances is a deep 0.3‰.
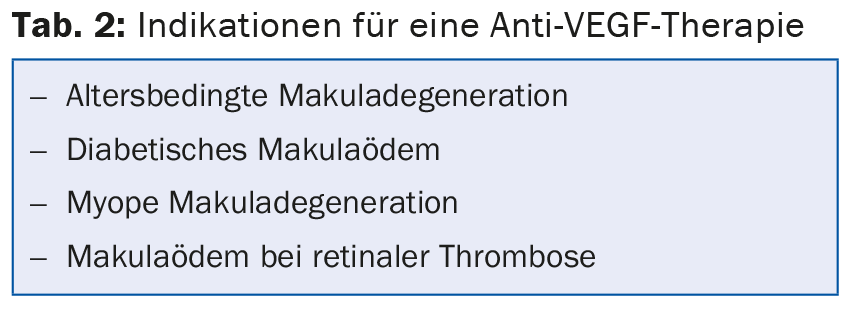
In Switzerland, approximately 65,000-70,000 intravitreal injections are now performed for various macular diseases (Tab. 2) . This means a workload for all involved that should not be underestimated, as well as a massive financial burden on the health care system.
Optical aids
Technological progress benefits visually impaired people in particular. On the one hand, a large proportion of older people have had contact with computers in their professional lives, and thus fears of contact have largely disappeared. On the other hand, image magnification and speech recognition programs are already available almost everywhere. Accordingly, a very important tip for those affected is to consult a low vision counseling service or a specialized low vision optometrist. If the central visual acuity drops below 0.2, there is an entitlement to a helplessness allowance in Switzerland, a support for everyday life that is often forgotten in the consultation.
Alternative treatment options
Dr. med. Google returns nearly 200,000 results within 0.3 seconds for the search term “treatment AMD”. The range of treatments offered is extremely wide, as is often the case with emotionally threatening diseases (blindness). A true track record is always missing and the financial outlay correlates inversely with the expected outcome. Here, the person seeking help is usually bamboozled – albeit with very well-made websites and glossy brochures.
In summary, great progress has been made in recent years, especially in the treatment of wet AMD. Early detection of appropriate patients is significant for treatment success. Therefore, raising the awareness of primary care internal medicine physicians, who play the central role in the medical care of the elderly, is very important here.
HAUSARZT PRAXIS 2015; 10(12): 25-28