50% of hypertensives are not well controlled with prescribed medications, and about 40% of sufferers in Switzerland are not diagnosed at all. Thilo Burkard, MD, spoke at the Zurich Hypertension Day about tricks of the trade to reduce the risks of insufficiently controlled blood pressure for patients.
50% of hypertensives are not well controlled with prescribed medications. In addition to these patients, however, many more people are unknowingly exposed to the risks of insufficiently controlled blood pressure. A study was able to show that about 40% of hypertensive patients in Switzerland are not even diagnosed. [1]. So is one of the problems of inadequate blood pressure therapy the diagnosis, Dr. Burkard asked at the beginning of his talk.
Problem diagnosis
A large American study retrospectively compared the rate of diagnoses of hypertension in older patients with that in younger patients. Accordingly, 27% of >60-year-olds remained undiagnosed over a four-year period, compared with 38% of younger people (25-31 years). The probability of a correct hypertension diagnosis at a young age was about 30% higher if the attending physician was female [2].
To bring the problem more into focus, “awareness” and systematic diagnosis are needed. The 2011 English guidelines provide an example. If the “office blood pressure” is ≥140/90 mmHg once, a 24-h blood pressure measurement or home measurement is recommended there [3]. Figure 1 shows the detailed procedure.
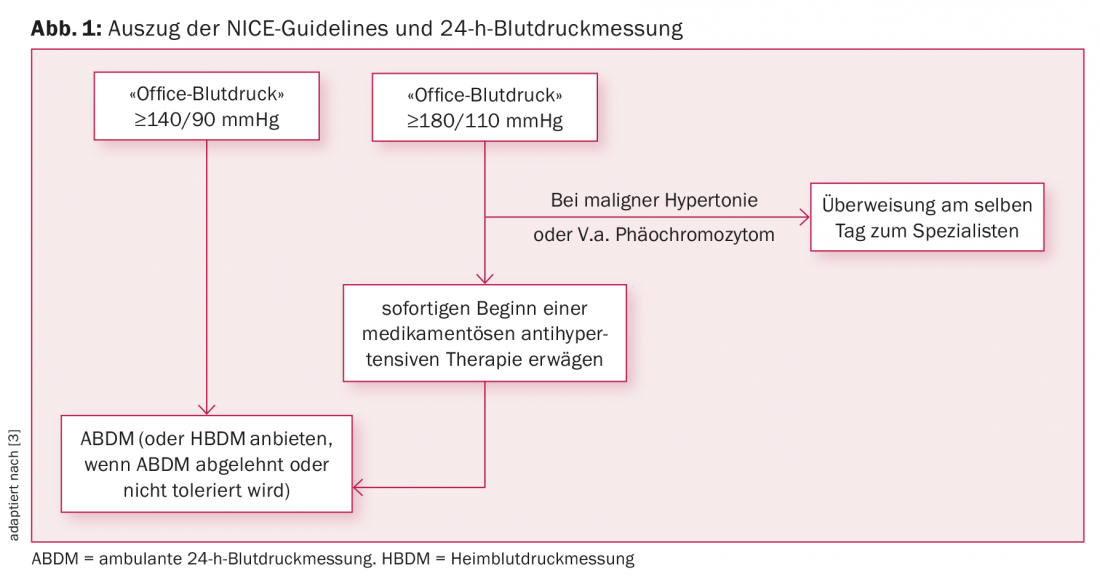
The Americans show a similar picture in their current guidelines. Class IA recommendation is to control elevated “office blood pressure” with home measurement [4]. 24-h blood pressure measurement tends to be neglected here due to often poor reimbursability.
Refractory hypertension – tips and tricks
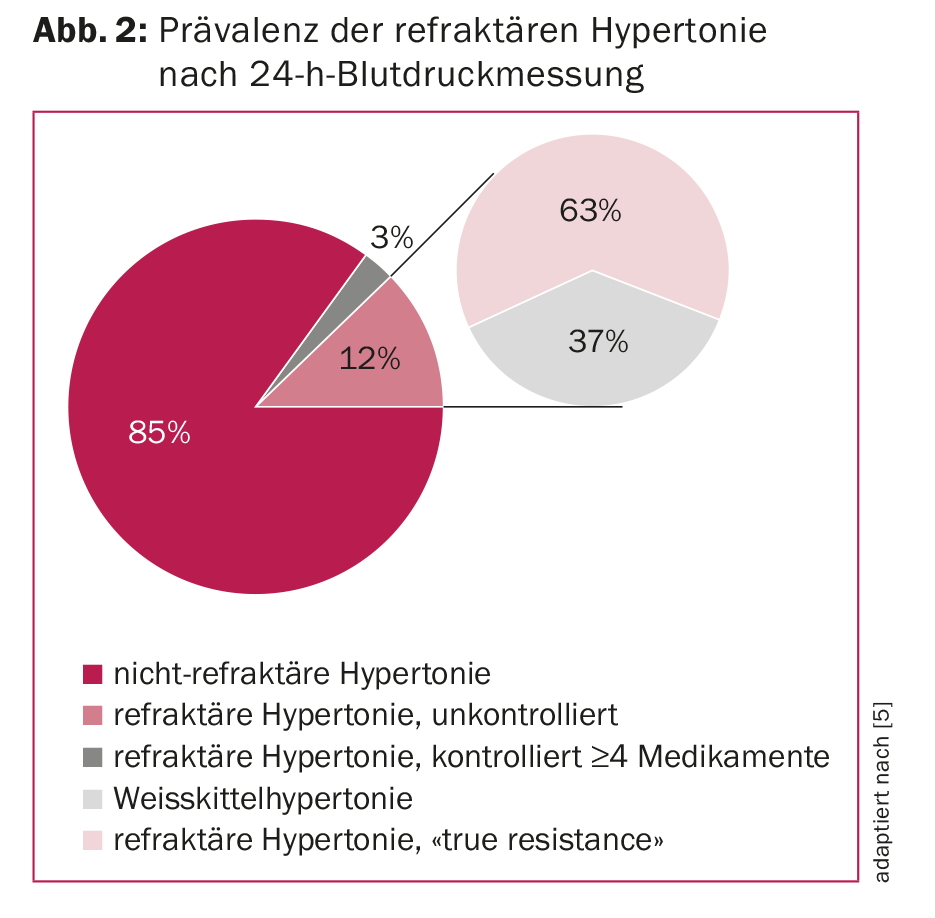
If the blood pressure is not satisfactorily controlled after successful diagnosis despite adequate therapy, the patient may have refractory hypertension. This is defined as an “office blood pressure” of ≥140/90 mmHg with existing treatment with ≥3 medications (one of which is a diuretic) [5]. For further diagnostic clarification, a 24-h blood pressure measurement is also recommended here as a first step, reports Dr. Burkard. Subsequently, it can be assessed, for example, whether true refractory hypertension is present or whether pseudoresistance exists, e.g., in the form of a white coat component. Figure 2 shows how large the proportion of pseudoresistant patients is.
One of the biggest problems in difficult-to-control hypertension is “non-adherence.” Before searching for other causes of refractory hypertension or implementing interventions, “nonadherence” should be ruled out. Only about half of all patients who are prescribed an antihypertensive take it correctly . The more medications prescribed, the worse the adherence. This can be caused by a language barrier, for example. One possible approach to solving this problem is cooperation with nearby pharmacies. Many offer their patients to dispense their medications in weekly dispensers, which helps to avoid medication errors and to reduce the number of tablets needed, in some cases considerably.
From the above, two simple rules for the setting of antihypertensive therapy can be formulated [nach Herb Kelleher]:
- “Keep it simple”
- “Don’t do anything that interferes with rule #1.”
The goal should be therapy with as few tablets as possible that work for the particular patient. It is important to look at the patient being treated and his or her individual response to the pharmaceuticals being used. Preference should be given to treatment with combination preparations in the sense of a simple drug regime. Early combination of drugs may show additive effects and also keep the side effect spectrum lower, as no single drug needs to be fully dosed. Similarly, preparations that have the longest possible half-life and can be given once daily are preferable.
What is the practical approach?
A simple but often effective approach is a combination of three main drug groups that can be combined with each other. Looking at adherence, it makes sense to combine ACE inhibitors or AT2 blockers with a calcium antagonist in the first step. In the second step, a thiazide or “thiazide-like” can be added. If another drug is subsequently required, spironolactone may also be considered after hyperaldosteronism has been ruled out. If this is done in ignorance of hyperaldosteronism, the diagnosis is made much more difficult, explains the speaker.
If the blood pressure is still not in the optimal range despite adequate therapy and it seems questionable whether the patient’s adherence is responsible for this, this can be checked quite easily with a 24-h blood pressure measurement after observed medication intake. The patient comes to the practice in the morning, receives the 24-hour blood pressure monitor and takes his medication in the practice, which is then recorded in the protocol. Subsequently, it becomes apparent whether adherence was the cause of uncontrolled blood pressure.
Consistent titration with accompanying close clinical follow-up has also been shown to be helpful in maintaining patient adherence. After each dose adjustment, the patient should be revisited to determine the effects of the adjustment on both objectively measured blood pressure and subjective well-being and to take action if necessary.
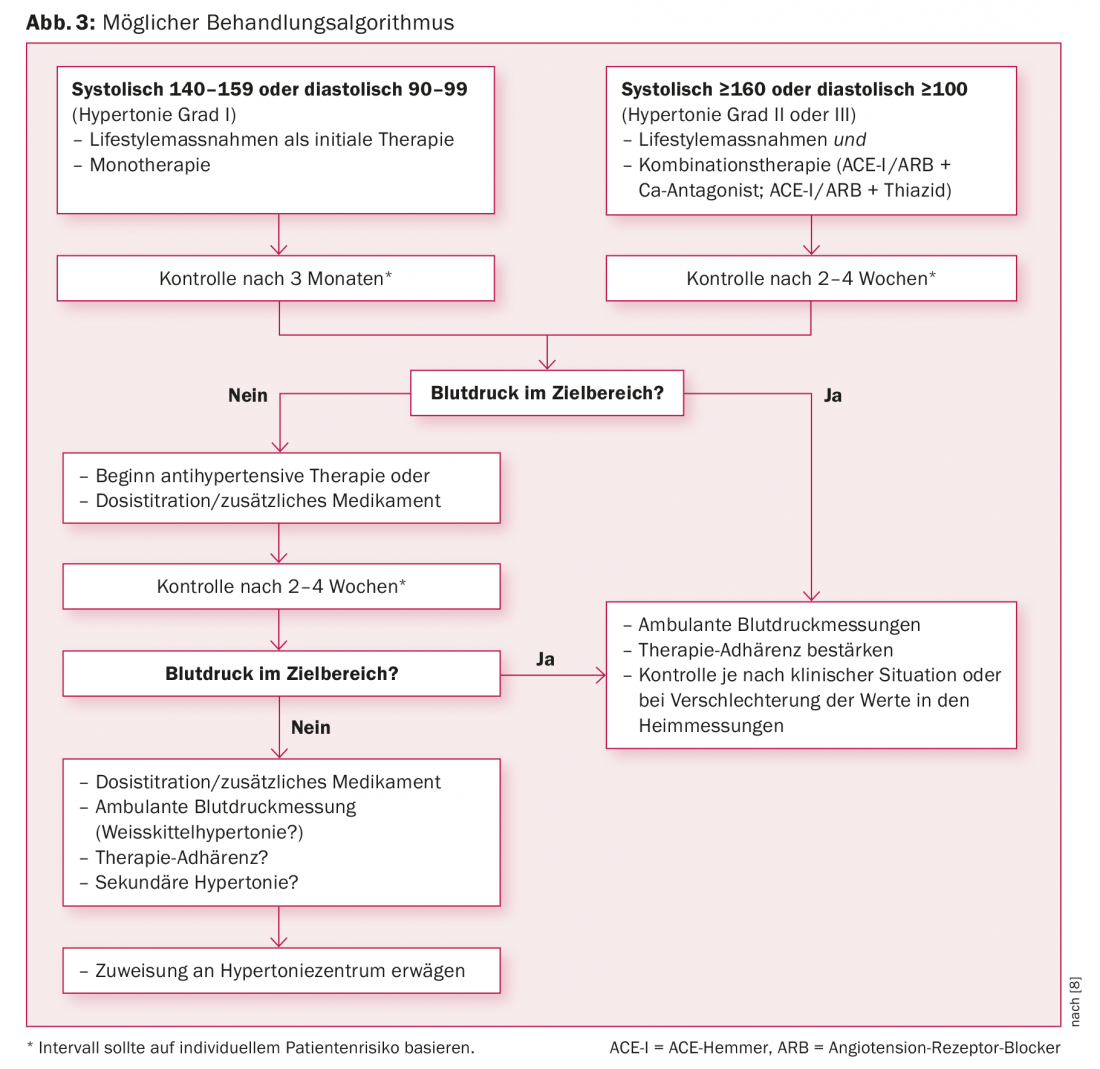
An overview of a possible treatment algorithm from the American Heart Association, American College of Cardiology, and Centers for Disease Control and Prevention can be found in Figure 3.
Blood pressure control – accessibility
According to an internal study by Kaiser Permanente, an American network that provides both medical care and insurance for its patients, blood pressure control is achievable in 90%. This figure is based on systematic efforts by Kaiser Permanente to improve care for its patients. The treatment plan consisted of establishing a hypertension registry to identify all hypertensives and correct measurements, compiling a simple treatment algorithm with regular adjustment, introducing “single-pill combinations,” and performing consistent titration. These measures increased intra-center blood pressure control from approximately 40% in 2000 to 90% in 2013 [6]. In addition to improved therapeutic success in hypertension, a 24% lower rate of myocardial infarction was shown within the network over a similar time period [7].
Source: 13th Zurich Hypertension Day, January 18, 2018.
Literature:
- Danon-Hersch N, et al: Prevalence, awareness, treatment and control of high blood pressure in a Swiss city general population: the CoLaus study. Eur J Cardiovasc Prev Rehabil 2009; 16(1): 66-72.
- Johnson HM, et al: Undiagnosed hypertension among young adults with regular primary care use. J Hypertens 2014; 32(1): 65-74.
- NICE: Hypertension in adults: diagnosis and management. Clinical guideline [CG127] Published date: August 2011 Last updated: November 2016 (www.nice.org.uk/guidance/cg127)
- Whelton PK, et al: 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017 Nov 13. pii: HYP.00000000000066. doi: 10.1161/HYP.0000000000000066. [Epub ahead of print]
- de la Sierra A, et al: Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertens 2011; 57(5): 898-902.
- Jaffe MG, Young JD: The Kaiser Permanente Northern California Story: Improving Hypertension Control From 44% to 90% in 13 Years (2000 to 2013). J Clin Hypertens (Greenwich) 2016; 18(4): 260-261.
- Yeh RW, et al: Population Trends in the Incidence and Outcomes of Acute Myocardial Infarction. N Engl J Med 2010; 362: 2155-2165.
- Go AS, et al: An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. J Am Coll Cardiol 2014; 63(12): 1230-1238.
Further reading:
- Ogedegbe G, Schoenthaler A: A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich) 2006; 8(3): 174-180.
- Calhoun DA, et al: Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertens 2008; 51(6): 1403-1419.
CARDIOVASC 2018; 17(2): 31-34











