Aneurysms are unstable at the beginning of their formation and rupture frequently. However, the majority of aneurysms stabilize without rupture. The decision to treat or observe depends on life expectancy and risk of treatment in addition to aneurysm factors.
Aneurysms are not congenital, they develop during life. With very few exceptions, however, it is not the aneurysm itself but the rupture with subsequent subarachnoid hemorrhage that becomes a life-threatening event for the patient. In principle, the association is true that treatment of nonruptured aneurysms can prevent bleeding from the aneurysm. However, on an individual basis, the risk of rupture must be weighed against the risk of treatment – and both risks vary widely depending on the situation, so the indication for treatment is always a case-by-case decision. The subject of this article is only incisional aneurysms without prior subarachnoid hemorrhage.
Prevalence of nonruptured aneurysms and incidence of rupture.
The incidence of nonruptured aneurysms in the population is 2-3% [1,2]. Higher numbers have also been published, but these are often from autoptic studies. Thus, the primary care physician or specialist is regularly confronted with this finding when prescribing an MRI for evaluation in patients with nonspecific complaints or headaches.
The incidence of rupture is approximately 5-10 persons per 100,000 population for Central Europe. It is higher in Japan and Finland for reasons that are unclear, but it seems to be converging in recent decades. Thus, it is clear that only a portion of aneurysms – about 15%, as we will show in the following paragraph – also rupture.
Rupture risk of non-ruptured aneurysms
Because most ruptured aneurysms are smaller than 7 mm, a rupture rate of 0.5-1% per year was assumed until 1999. Surprisingly, the most extensive study in 1077 patients (prospective arm), initially conducted retrospectively and then prospectively, showed a significantly lower risk than previously assumed [3]. In particular, the frequent small incidental aneurysms of a size of <7 mm had a rupture risk of only 0-0.1% per year. There is consensus among experts that the ISUIA data are probably too low because of selection bias (many patients in this group underwent surgery), short follow-up time (of the 535 patients mentioned above, only 260 were followed up for two years, only 112 for four years, and only 35 for six years), and retrospective group definition. Nevertheless, the significantly lower rupture risk compared to previous assumptions has also been confirmed in practice during the currently much more frequent “wait and scan” management. This should be distinguished from so-called additional aneurysms, which were known to be present in patients with SAB from another aneurysm, or any aneurysms larger than 7 mm.
The modern theory of aneurysm disease
The biggest contradiction is that we see patients in the emergency department with rupture and subarachnoid hemorrhage whose aneurysm in more than 50% of cases is less than 7 mm in size [4], but in incidentally discovered aneurysms of the same size category, only two of 535 patients show rupture over the course of one to four years.
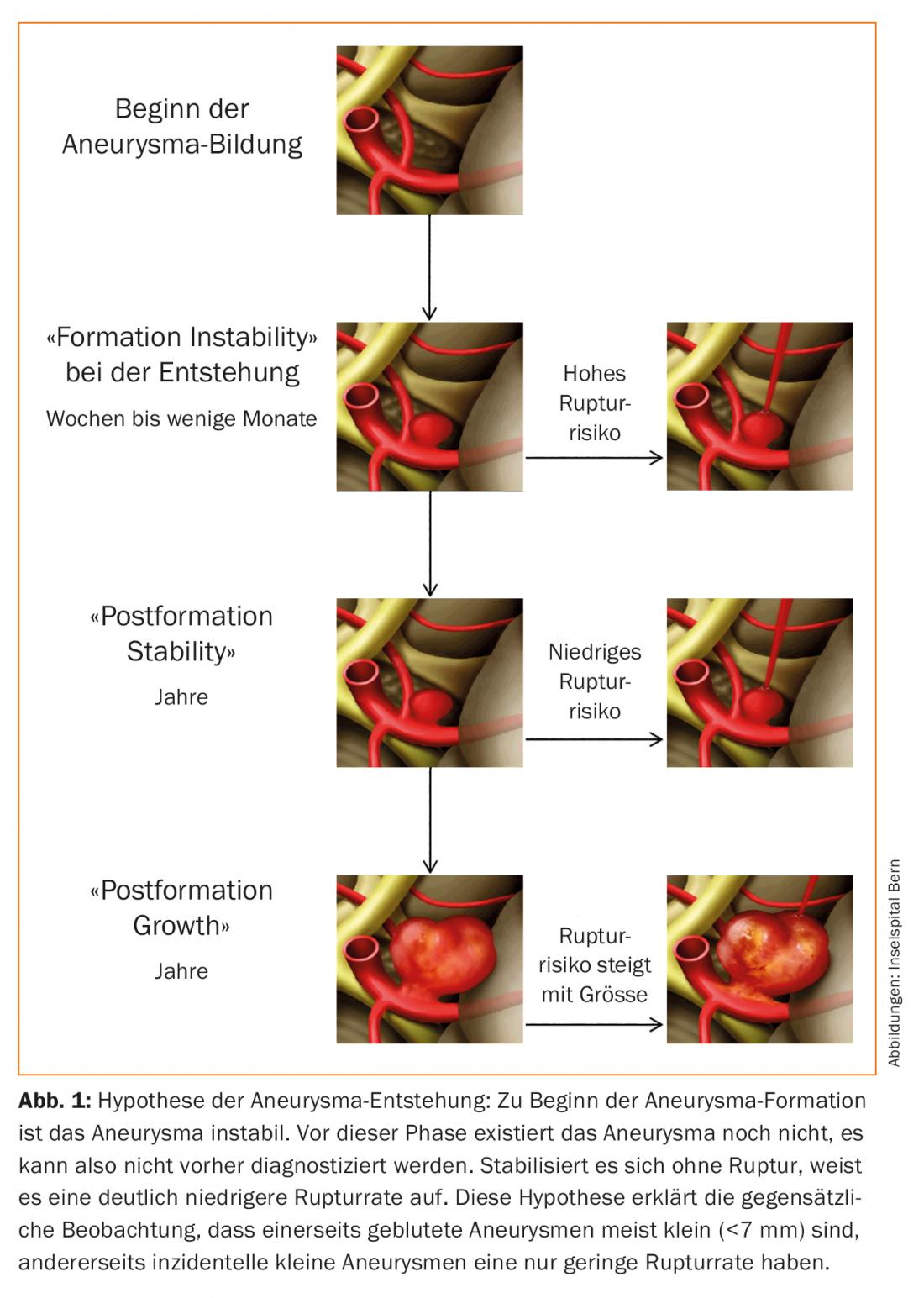
One theory that is gaining ground combines both observations. Aneurysms are likely to develop within a few weeks or months. During this time, the aneurysm is unstable and may rupture. This unstable phase is hardly observable by random imaging because it is very short. After that, it stabilizes and can remain stable in size for a long time or even permanently. A part of the aneurysms grows and thus again reaches a partly considerably higher risk of rupture due to increase in size and wall changes during growth. (Fig. 1). Based on available epidemiological data, it can be roughly estimated that of all aneurysms, approximately 15% rupture during the “birth” of the aneurysm and 15% rupture during its subsequent course – the latter usually associated with risk factors.
Factors for the risk of rupture
The most significant risks are:
- A growth or visible configuration change of the aneurysm (5-20-fold).
- Genetic in familial aneurysms (sixfold).
- Polycystic kidney disease (quintuple)
- Localization
- Arterial hypertension
- Smoking
- Heavy alcohol consumption with more than 300 g/d.
The latter factors are associated with an approximately two- to fourfold increase in risk [5].
A separate risk group with higher rupture rates, as mentioned earlier, are the additional aneurysms in which the patient has already been treated for hemorrhage from rupture of another aneurysm.
Even for treated aneurysms, aneurysm recurrence may occur depending on the treatment method and therapeutic outcome. These patients may also be prone to de novo aneurysms in 0.5-2.5% of cases per year.
Forget, watch or treat?
Best management depends on many factors and is always a case-by-case decision involving the following factors:
- Rupture risk
- Treatment risk
- Life expectancy taking into account the quality of life
- Risk type and setting of the patient.
The risk of aneurysm rupture from an incidentally discovered finding varies from 0.1% to 10% per year in extreme cases and depends on size and the other risk factors already mentioned. For practical application, the PHASES score has been established, which is a sum score for estimating risk [6].
The risk of treatment also depends on many factors, but most clearly on the size of the aneurysm. Thus, the large or “giant” aneurysms that have the highest risk of rupture also have the highest risk of treatment. The complication risk of the procedure should ideally not be known from the literature, but from quality control via one’s own database.
When weighing “risk of rupture/risk of treatment,” one must not forget the influence of the immediate risk of complications from treatment versus the delayed risk of rupture with observation. The apparent equality of risks-for example, for a 4% risk of bleeding over the next 20 years at 0.2% per year risk of rupture and a 4% risk of severe complications with treatment-is incorrect because, unlike the treatment complication, the rupture rate with observation is statistically distributed over the 20 years. Equality is achieved only when the observation time is doubled.
Follow-up – “wait and scan” – is a common management for many patients. Small aneurysms of the anterior circulation without significant risk factors have a low risk of rupture, probably largely reduced to cases with size growth or shape change. Again, the PHASES score helps to estimate the probability of growth, which ranges from 1% to 5% per year [7]. If an aneurysm shows an increase in size, the risk of rupture increases massively and is 5-10% per year. Thus, a demonstrated growth or configuration change will usually provide an indication for treatment.
Summary
The recent epidemiological figures suggest a low risk of rupture for incidental small aneurysms (<7 mm) of the anterior cerebral circulation. However, additional risk factors and treatment complications of endovascular or microsurgical therapy are often just as critical in determining the best management in a specific patient. Often, no clear recommendation can be made during a consultation with the physician, and the patient’s risk type has a significant influence on the decision. Whether to observe or treat an incidentally discovered aneurysm remains a highly individualized neuromedical decision that should be made by an interdisciplinary and well-coordinated team that understands its own complications. Thus, we see and discuss about 850 cases annually in our interdisciplinary aneurysm board (aneurysma.board@insel.ch), which shows the extent of incidental findings.
Take-Home Messages
- With modern imaging and a prevalence of 2%, primary care physicians and specialists are frequently confronted with the incidental finding of an incisional aneurysm.
- Aneurysms are unstable at the beginning of their formation and rupture frequently. However, the majority of aneurysms stabilize without rupture.
- The risk of aneurysm rupture from an incidentally discovered finding varies from 0.1% to 10% per year in extreme cases and depends on size and other risk factors.
- Many aneurysms can be observed. In particular, small aneurysms (<7 mm) of the internal cerebral artery and the middle cerebral artery have a low risk of bleeding if no other risk factors exist.
- However, the decision to treat or observe depends on life expectancy, the risk of treatment, and the patient’s attitude to risk, in addition to many aneurysm factors, and should be discussed in an interdisciplinary aneurysm board.
Literature:
- Vernooij MW, et al: N Engl J Med 2007; 357: 1821-1828.
- Etminan N, et al: Nat Rev Neurol 2016; 12: 699-713.
- Wiebers DO, et al: Lancet 2003; 362: 103-110.
- Beck J, et al: Acta Neurochir 2003; 145: 861-865.
- Rinkel GJ: Lancet Neurol 2005; 4: 122-128.
- Greving JP, et al: Lancet Neurol 2014; 13: 59-66.
- Backes D, et al: Stroke 2015; 46: 1221-1226.
InFo NEUROLOGY & PSYCHIATRY 2017; 15(5): 4-6.











