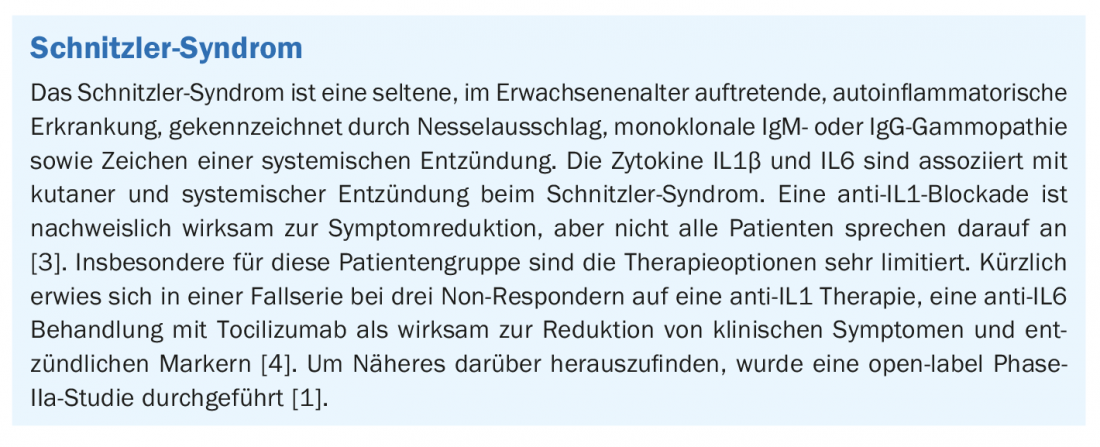
Schnitzler syndrome is a rare autoinflammatory disorder. Core symptoms include chronic, recurrent hives. In particular, for patients who do not respond to anti-IL1 therapy, there is a need for new treatment options. An open label proof-of-concept study was conducted to evaluate the effects of treatment with the anti-IL6 antibody tocilizumab.
The results of the research team, with the participation of dermatologists from Charité Universitätsmedizin Berlin, were presented at this year’s virtual annual meeting of the Arbeitsgemeinschaft dermatologische Forschung (ADF) [1]. The single-arm open-label single-center phase II study [2] included a 20-week treatment phase (part A), followed by an optional 32-week extension phase for patients with complete or partial response to therapy (part B). Study participants received weekly subcutaneous injections of 162 mg tocilizumab. The primary endpoint was defined as the change in Physician Global Assessment (PGA) score from baseline to week 20. The PGA is a composite score that includes the following five main clinical symptoms of Schnitzler syndrome: Hives, Fatigue, Fever, Myalgia, and Arthralgia/Bone Pain. Each subscore was scored on a scale from 0 (no disease activity) to 4 (maximum disease activity), and a sum score was calculated (range: 0-20). Secondary endpoints included self-reported disease activity (measurement tool: Schnitzler Activity Score)*, changes in inflammatory markers (C-reactive protein [CRP], serum amyloid A [SAA], erythrocyte sedimentation rate [ESR], S100A8/9), and self-reported quality of life (Dermatology Life Quality Index, DLQI**). The safety and tolerability of tocilizumab treatment were also assessed.
* Schnitzler Activity Score contains five subscales corresponding to the five main symptoms of Schnitzler syndrome
** DLQI: 36-item short form
Evidence for effectiveness
8 patients were included in the study. Data analyses show a decrease in mean PGA scores at week 20 (3.3 [SD 3,6]) compared with baseline (12.1 [2,5]; p<0.001). Regarding Schnitzler Activity Score*, tocilizumab treatment resulted in lower expressions of total scores at week 20 (days 134 to 140; 1.3 [SD*** 1 .0]) compared with the screening phase (days -7 to -1; 3.0 [1,4]). Mean concentrations of inflammatory markers normalized at week 20 (CRP 0.6 mg/l [SD*** 1 .0]; ESR 12.6 mm/h [13,1]; SAA 4.1 mg/l [3,5]) compared with baseline (CRP 31.7 mg/l [54,1]; ESR 37.6 mm/h [29,3]; SAA 176 mg/l [260,2]). Regarding DLQI and SF-36 scores, there were no relevant differences from baseline to week 20. Exploratory assessments of IgMκ and IgGκ concentrations also showed no relevant changes. Mean levels of IL6 concentrations increased from 7.1 pg/ml [SD*** 2 .7] at baseline to 0.9 pg/ml [35 .4] at week 20 (p=0.0162). The concentrations of IL18 and IL1 receptor antagonists did not change to a relevant extent.
*** [SD]=standard deviation
Three of the four patients with elevated scores for hives, fatigue, myalgia, and arthralgia/bone pain had higher PGA scores at the end of part B of the study compared with the end of part A. In contrast, the concentrations of inflammatory markers remained low during part B of the study, as shown by a look at the data collected at week 52 (mean values [SD***]): CRP: 0.4 mg/l [0,3]; ESR: 4.5 mm/h [1,9]; SAA 6.4 mg/l [7,8]. With regard to cytokine levels and quality of life, there were no changes during the extension phase. A total of 57 mild or moderate adverse events were reported, most of which were infections.
In summary, tocilizumab treatment initially reduced clinical symptoms and inflammatory markers, although efficacy waned over time in most patients. The authors suggest tocilizumab should be considered in patients with inadequate response to other targeted therapies (e.g., anti-IL1) [1].
Congress: Arbeitsgemeinschaft Dermatologische Forschung (ADF) 2021
Literature:
- Bonnekoh H, et al: P041, Clinical research, ADF Dermatology Awards V, ADF Annual Meeting 3/6/2021.
- NCT03046381, https://clinicaltrials.gov/ct2/show/NCT03046381, (last accessed Mar. 30, 2021).
- Bonnekoh H, Krause K: The Schnitzler syndrome… Akt Rheumatol 2017; 42: 53-58.
- Krause K, et al: J Allergy Clin Immunol 2020; DOI: 10.1016/j.jaci.2019.12.909.
- Krause K, et al: Allergy Clin Immunol. United States 2012: 129(3): 848-850.
DERMATOLOGIE PRAXIS 2021; 31(2): 33 (published 12/4/21, ahead of print).