Introduction: Tolosa-Hunt syndrome (THS) is a rare idiopathic inflammatory disorder that may involve the cavernous sinus, orbital apex, and superior orbital fissure. The leading symptom is painful unilateral ophthalmoplegia and oculomotor nerve palsy; this is due to extrinsic compression of neurovascular structures in the cavernous sinus. Diagnosis is based on clinical symptoms and typical MRI changes, as well as response to steroid therapy and exclusion of other inflammatory or neoplastic diseases of the cavernous sinus. Steroid therapy is the treatment of choice; symptom relief usually occurs within 72 hrs.
Case report: Referral of a 22-year-old female patient with headache and periorbital pain on the right side for 14 days, partly synchronous with the pulse. The patient also reported additional double vision for ten days. Neurological workup revealed right abducens palsy and hypesthesia of the right central face – onion skin-like sensory disturbances around the mouth and nose. Supplemental CSF aspiration showed elevated GP at 0.69 g/L, normal opening pressure, no signs of intrathecal immunoglobulin synthesis, no oligoclonal bands, and unremarkable lactate and glucose. Cytologically, few small mature lymphocytes were found. Lyme serology, HIV, and lues were negative. No evidence of sarcoidosis. To complete the diagnosis, an MRI of the skull was performed with the question of sinus vein thrombosis.
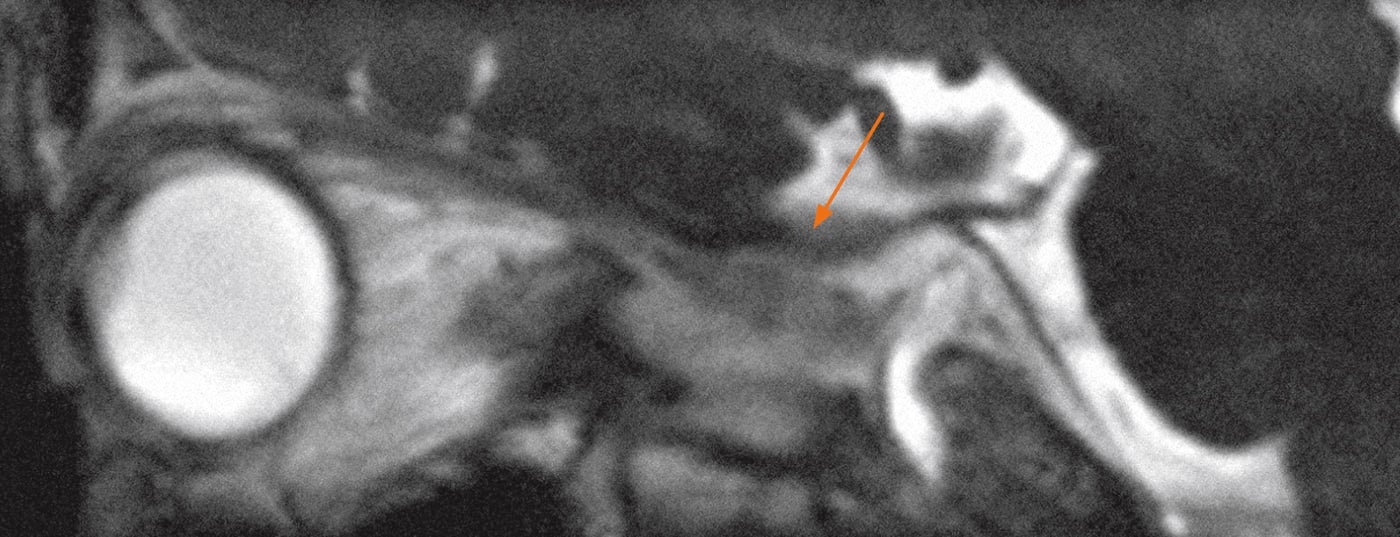
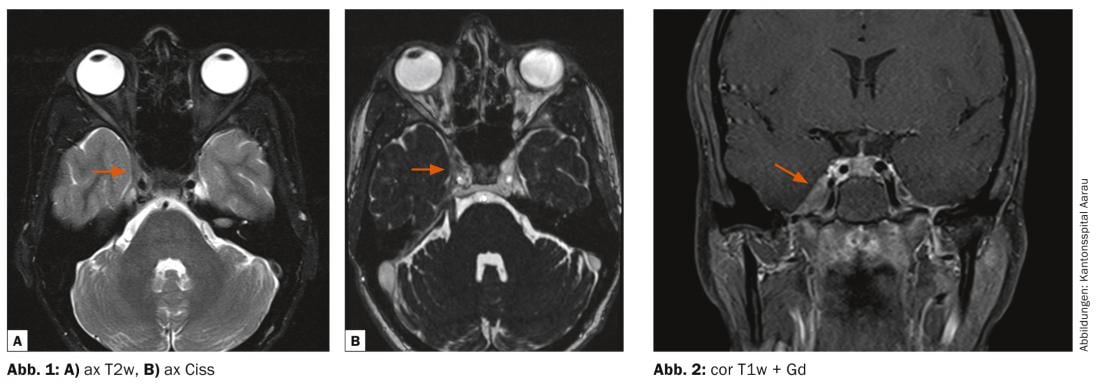
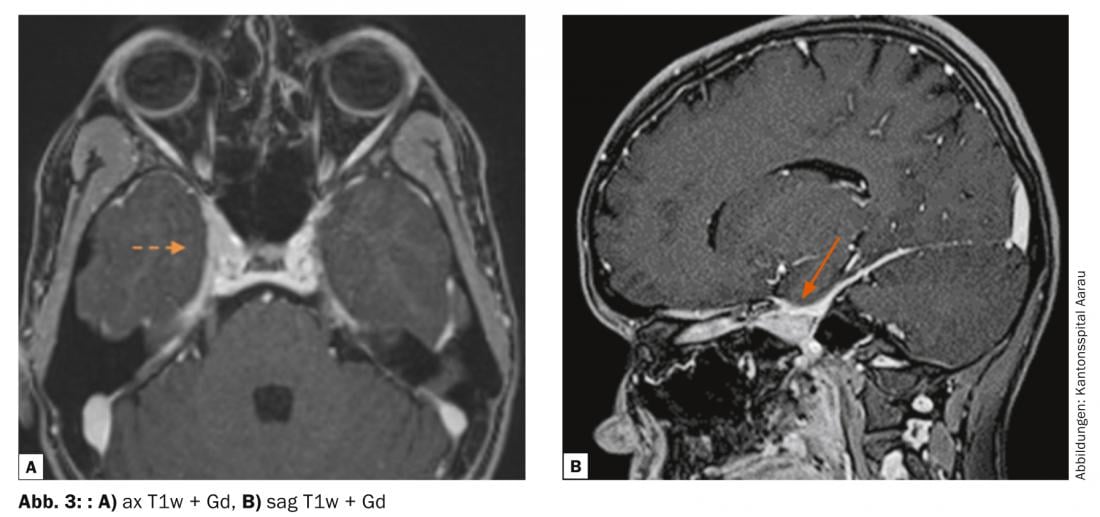
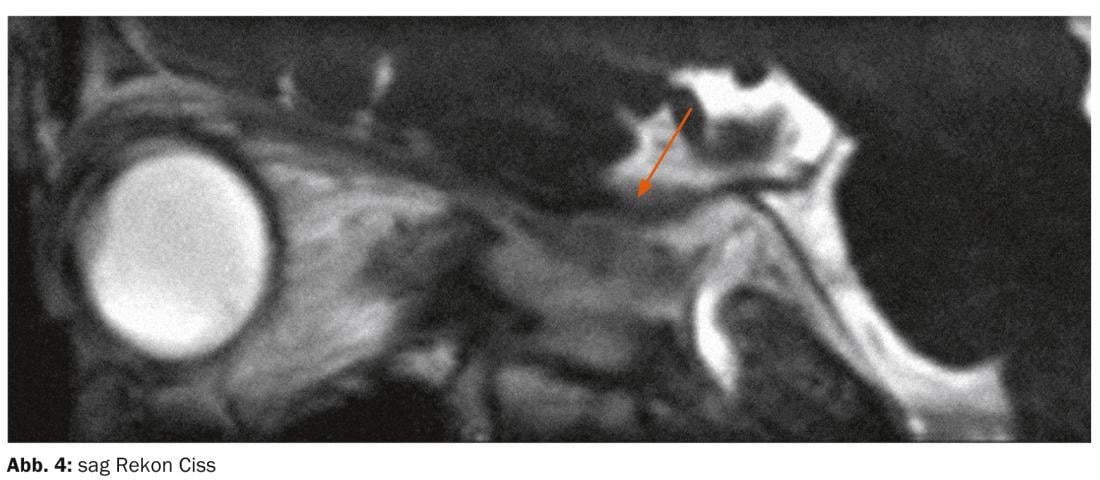
MRI diagnosis: In T2w and in the Ciss sequence at the level of the trigeminal nerve, evidence of a hypointense soft tissue plus in the right cavernous sinus; there was contact with the right internal carotid artery and the right superior orbital fissure (Fig. 1) . In lateral comparison, the lumen of the internal carotid artery was slightly narrower on the right side. Laterally, the soft tissue formation was smoothly bordered to the temporal lobe. This was peloted, but no brain edema was found in the adjacent brain parenchymal sections. The KM series showed distension of the cavum meckeli by a KM-absorbing soft tissue plus compared with the opposite side (Fig.2 and 3). Figure 4 shows the soft tissue plus in the cavum meckeli.
Discussion: THS was first described by Eduardo Tolosa, a Spanish neurosurgeon, in 1954. At that time, he described a periarteritis of the cavernous internal carotid artery – a nonspecific chronic granulomatous inflammation with proliferation of fibroblasts as well as infiltration of the septa and the wall of the cavernous sinus with lymphocytes and plasma cells. These changes were confirmed by William Edward Hunt, an American neurologist and neurosurgeon, in 1961. In addition, Hunt described six characteristic features of the syndrome: persistent periorbital pain; deficits in the third, fourth, or sixth cranial nerves or the first branch of the fifth cranial nerve-rarely involving the optic nerve or sympathetic fibers around the cavernous portion of the internal carotid artery; symptom duration of two weeks; occasional spontaneous remissions; recurrent attacks of pain; and prompt response to steroids.
Since 1988, the International Headache Society (IHS) has included THS among the cranial neuralgias. MRI initially fell into the role of excluding other causes, such as meningiomas, metastases, lymphomas, aneurysms, and internal carotid artery infections, because clinical symptoms were not specific for THS. In the revised IHS classification of 2004, clinical aspects now also play a role.
THS is a disease caused by inflammatory tissue primarily localized in the cavernous sinus. In principle, there is the possibility of extension into the superior orbital fissure and the optic canal. In addition to the affection of cranial nerves, here especially the oculomotor, abducens and trochlear nerves as well as V1 and V2 of the trigeminal nerve, stenosis of the internal carotid artery occurs in rare cases. This is caused by inflammatory infiltration of the adventitia. THS is usually unilateral in location, but some authors report rare bilateral involvement in approximately 5% of cases. Because MR diagnostics are nonspecific with respect to the diagnosis of THS, some authors believe that regreening of pathologic findings on imaging after steroid therapy should be considered diagnostic of THS. Nevertheless, caution is advised in this regard as well, because other diseases such as lymphoma or vasculitis also respond to steroids. Basically, THS is therefore a diagnosis of exclusion. Since a biopsy is rarely performed in this region resp. is feasible, some authors recommend clinical and radiological follow-up over two years.
In the present case, the patient presented with the classic symptom of right periorbital pain and typical cranial nerve deficits. By means of MRI, a tentative diagnosis of THS was made. With subsequent steroid therapy, the headache was completely regressed by the following day. The abducens palsy and facial hypesthesia on the right side still existed and showed regression only in the further course.
Further reading:
- Yousem DM, et al: MR imaging of Tolosa-Hunt syndrome. AJR 1990; 154(1): 167-170.
- Kline LB, Hoyt WF: The Tolosa-Hunt syndrome. J Neurol Neurosurg Psychiatry 2001; 71: 577-582.
- Lee JH, et al: Cavernous sinus syndrome: Clinical features and differential diagnosis with MR imaging. AJR 2003; 181: 583-590.
- Tolosa E: Periarteritic lesions of the carotid siphon with the clinical features of a carotid infraclinoid aneurysm. J Neurol Neurosurg Psychiatry 1954; 17: 300-302.
- Korchi AM, et al: Imaging of the cavernosus sinus lesions. Diagnostic and Interventional Imaging 2014; 95: 849-859.
- Schuknecht B, et al: Tolosa-Hunt syndrome : MR imaging features in 15 patients with 20 episodes of painful ophthalmoplegia. European Journal of Radiology 2009; 69: 445-453.
- Sánchez Vallejo R, et al: MRI findings in Tolosa-Hunt syndrome (THS). British Medical Journal Case Report 2014 Nov 3; 2014. pii: bcr2014206629. doi: 10.1136/bcr-2014-206629.
InFo NEUROLOGY & PSYCHIATRY 2015; 13(2): 24-27.