Originally, humans were hairy all over their bodies until a few 100,000 years ago, when a pseudogene essential for keratin formation slowly lost its functionality for hair follicles in certain regions of the body. In the course of evolution, therefore, hardly any terminal hairs were formed on the body. Thus, man became a “naked ape”.
The differentiation of embryonic cells leads to the development of organs. Already in the embryonic stage, in the fifth week of gestation, the brain and heart are formed. Gradually, more structures emerge until, around the ninth week, the hair systems also emerge. An average of 5 million hair follicles (= pilosebaceous units) are formed throughout the skin. Excluded are palms, soles, lips, and semi-mucous membranes. The number is already fixed at this stage, no new hair follicles are formed during life. From the very beginning, each hair/sebaceous gland unit has an individual genetic program that tells it when in life a hair will grow or fall out at which part of the body in response to which stimulus (or in terms of the sebaceous glands, the regulation of sebum production). In the 15th week of gestation, the fetus is covered with fine lanugo hairs (downy hairs) on the entire skin, almost all of them fall out again by birth, some are still present at birth, e.g. in the area of the shoulders or on the head. According to this, hair growth is controlled by the genetic program: terminal hair is formed at certain times on the head, axillary and genital areas, eyelashes and brows are formed, and vellus hair (woolly hair) is formed in some places.
Too little hair (hypotrichosis, alopecia)
In addition to other forms of hair loss such as circular hair loss, which usually has a psychosomatic background, fungal diseases of the scalp, autoimmunologically caused scarring scalp diseases that lead to pronounced hair loss, and diffuse hair loss, which can have many systemic causes (iron deficiency, stress, psychological stress, thyroid diseases, paraneoplastic, alimentary, post-inflammatory, post-partem), the most common form of disturbing persistent hair loss is hormonally induced androgenetic alopecia.
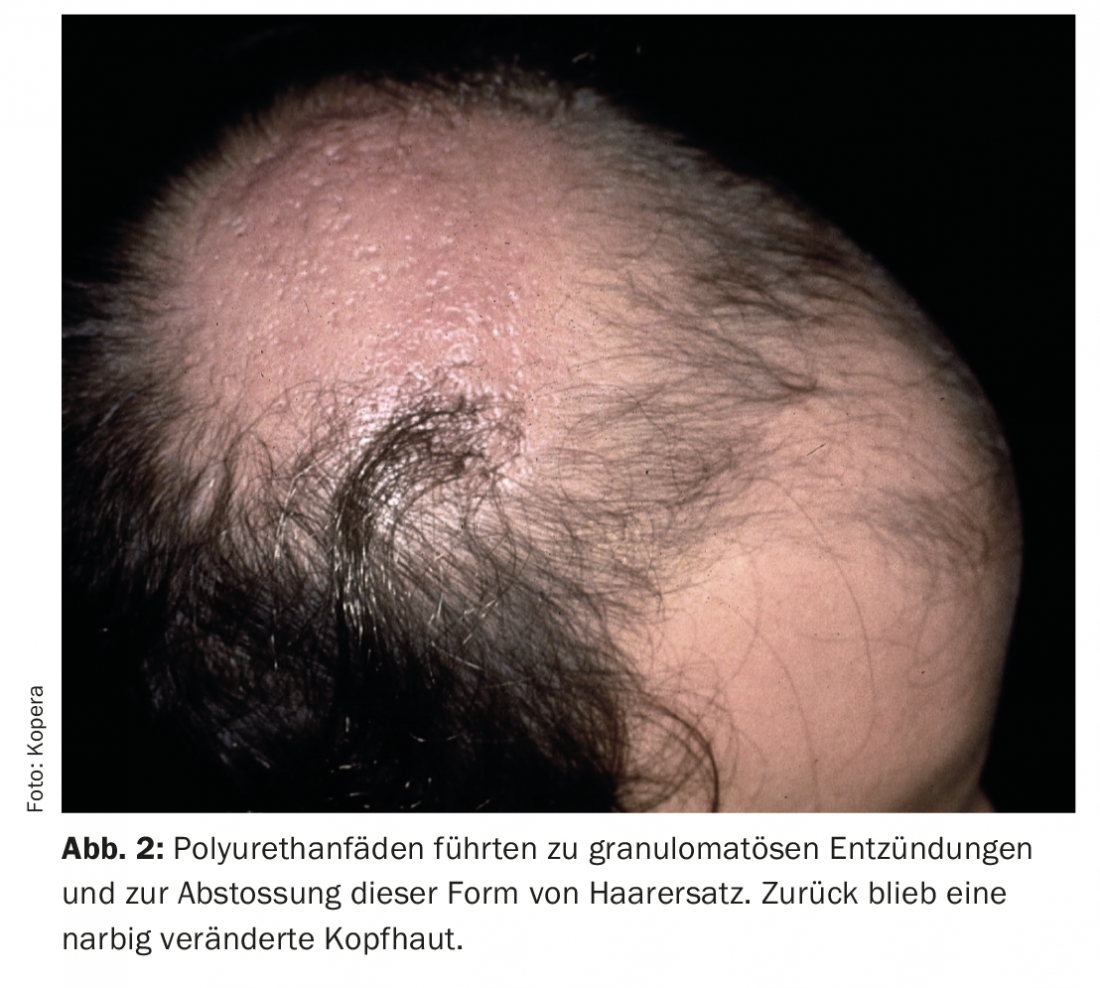
Due to the individually varying sensitivity of hair follicles to male hormones in the blood, certain hair growth patterns result in androgen-sensitive areas of the body. These have different phenotypes in males and in females. The male hormones in the serum are usually within the normal range. The cause is precisely the sensitivity of the hair follicles to androgens. The most effective form of androgens for hair roots is dihydrotestosterone, which in men slowly causes hair roots to atrophy, especially on the head, but in the opposite direction leads to increased hair growth on the body (Fig. 1) . In women, the cause of hormonally induced hair loss is other androgen metabolites such as androstenedione and dihydroepiandrosterone. The clinical picture of female-type androgenetic alopecia is somewhat different, with clearing occurring in the parietal region, although the anterior hairline is usually preserved.
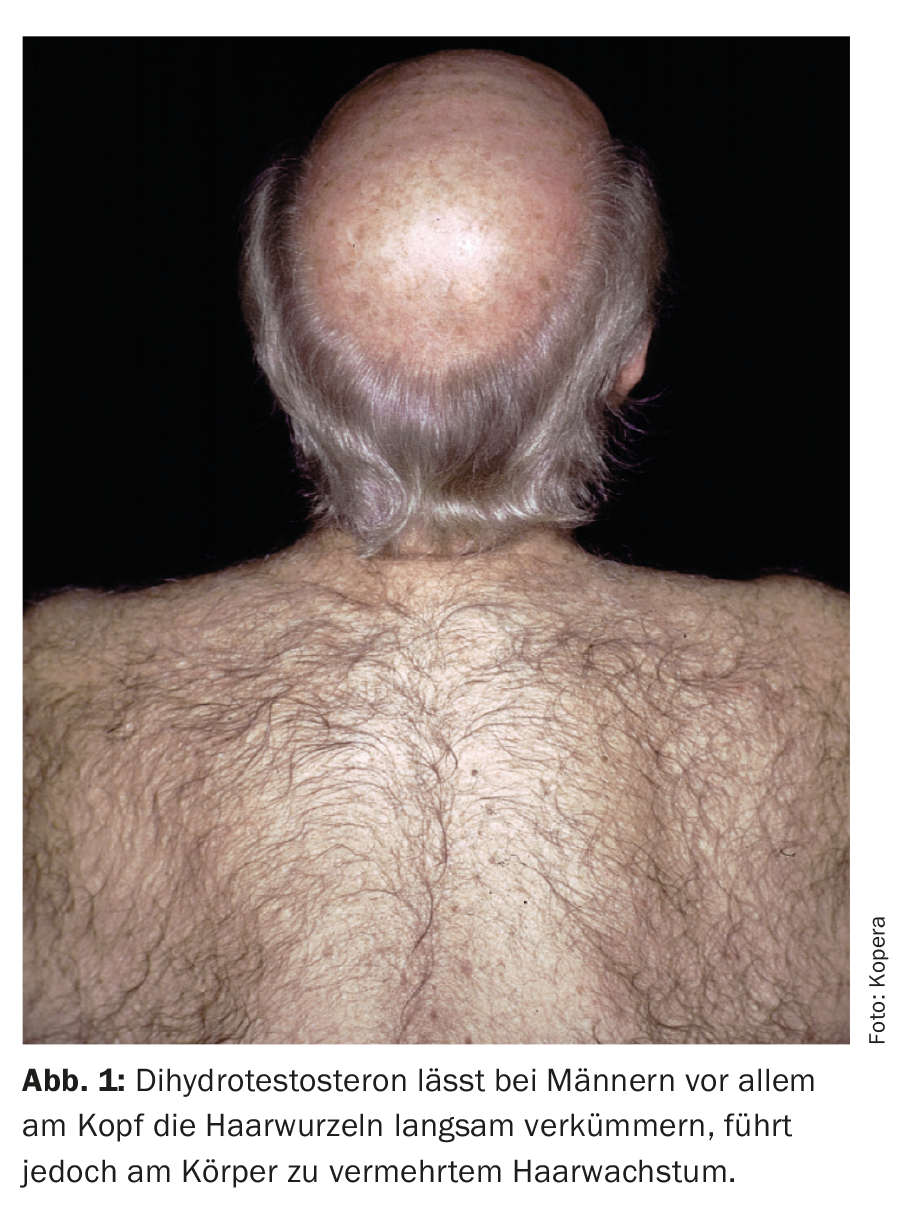
Options for non-drug treatment exist. One can dismiss hair loss as a phenomenon with little pathological value and not prescribe any therapy, but this is not the strategy of choice in cases of great suffering. 30 years ago, artificial hair came on the market, which was knotted in the scalp. However, these polyurethane threads were recognized as foreign bodies, leading to granulomatous inflammation and eventual rejection of this form of hair replacement. What remains is scarred scalp (Fig. 2). In the meantime, the method has become obsolete. The most effective method to “re-grow” hairless or heavily thinned areas of the scalp is autologous hair transplantation for the treatment of receding hairline or “male pattern baldness”. In this procedure, micro or single hair grafts are transplanted from androgen-insensitive areas in the occipital region to the vertex, parietal or high frontal region.
Non-drug hair growth boosters
Intracutaneous injection of platelet-rich plasma (PRP) has been advocated by some authors to stimulate hair growth, but has shown quite controversial results in clinical trials [1]. Low-energy laser systems are said to have biostimulatory effects. Therefore, low-level lasers are built into hair treatment helmets so that the stimulation of hair roots by the red light can be achieved. Here, too, a positive effect has not been clearly proven or has only been described in combination with minoxidil and/or finasteride [2].
Too much hair (hypertrichosis, hirsutism)
Congenital hypertrichosis lanuginosa is rare and is inherited in an x-linked dominant manner. Acquired hypertrichosis lanuginosa may be pearaneoplastic in origin. A special form of generalized hypertrichosis is that caused by a defect on chromosome 11, which causes hair roots to actively grow all over the body. This affected Petrus Gonsalvus, who was discovered on a Mediterranean island in the 16th century and was allowed to live a good life in the European courts. The x-linked dominant inheritance also affected his daughter. They are immortalized on large portraits in the picture gallery of the Kunst-historisches Museum Wien at Ambras Castle near Innsbruck. This led to the filming of “The True Story of Beauty and the Beast” in the documentaries of the series Universum History [3]. Local hypertrichosis may be mechanically induced [4].
Hirsutism
Hirsutism refers to the unwanted hair growth in women caused by hyperandrogenic metabolism and occurs in 90% of cases in the context of PCO syndrome.
The extent of body hair varies between different cultures and ethnic groups. Therefore, it is important to distinguish between androgen-dependent hirsutism and increased vellus hair in women of Mediterranean or Indian descent. Hirsutism refers to more or less pronounced hair growth corresponding to the male phenotype in women and affects about 5% of all women.
From an internistic point of view, hirsutism can have multiple causes. In addition to rare ones such as ovarian and adrenal tumors, congenital adrenal hyperplasia, insulin resistance syndromes, and Cushing’s disease, polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of childbearing age, affecting approximately 5-10% of all women. At >70%, PCOS is the most common cause of hirsutism and should be considered even in women with normal cycles.
Hirsute women need not have elevated testosterone levels, but hyperandrogenemia may still be present. The very complex interplay between increased LH/FSH ratio and consequently increased GnRH secretion and insulin metabolism in women with PCOS takes direct and indirect influence on serum androgen levels and leads to actually measurable or relative hyperandrogenemia. In addition, insulin acts synergistically with LH on the theca cells and causes a further increase in androgen production. Furthermore, insulin inhibits the production of SHBG in the liver, which is responsible for the binding of testosterone, this leads to increased free testosterone, while total testosterone may be in the upper normal range or only slightly increased [5]. Hirsutism can have negative effects on the psychosocial well-being and behavior of affected women [6].
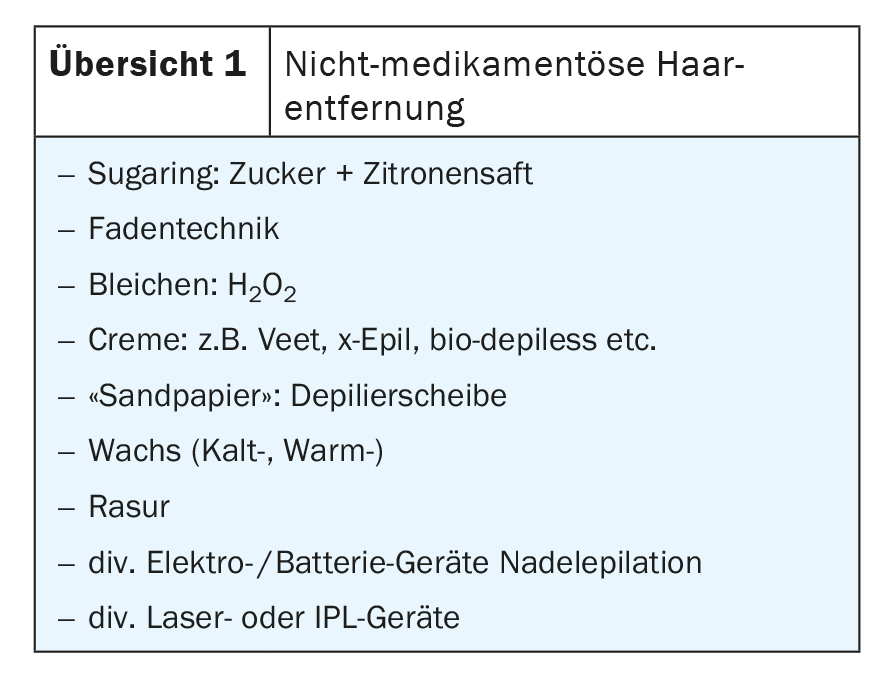
Treatment of hirsutism must be individualized and interdisciplinary to each case. In most cases, a combination of several treatment approaches leads to the desired result; antiandrogens and insulin sensitizers are used as medications. Non-medicinal options include all types of mechanical epilation (Overview 1) as well as light-assisted epilation with laser or IPL technology.
The application of various high-energy laser systems (ruby, NdYAG, alexandrite and various diode lasers) [7–11] and broad-spectral IPL systems (intense pulsed ligh) currently offers the most effective alternative for sustainable reduction of hair growth.
Light from the visible red to the near infrared wavelength range (694 nm to 1064 nm) (for IPL from yellow to infrared) is optimally absorbed by pigmented structures, in this case by the hair follicle, and leads to damage of the target structure by converting the light energy into thermal energy. The pulse duration corresponds approximately to the thermal relaxation time [12] of the pigment, so that although the pigmented hair follicle is damaged, the unpigmented tissue in the surrounding area is spared. This effect and the cooling of the skin surface ensure the low side effect treatment without signs of burning or blistering. Only transient redness is expected for a few hours after treatment. The absorption behavior of the pigments explains the fact that unpigmented hair does not respond or responds only very slightly to this method.
Countless clinical studies with a wide variety of experimental setups have been published in recent years to filter out which wavelength or which specifications lead to the best result, i.e. the best possible reduction in hair growth. So far, it has been shown that the currently popular devices offered for hair removal can all be used for safe and effective hair reduction, except for small differences in application, such as beam diameter, cooling system or tolerance without cooling: Several treatments at intervals of 4 to 6 weeks lead to sustainable hair reduction of 50-84% after an average observation period of 6-12 months. New laser epilation may lead to further hair reduction, transient hypopigmentation may occur in patients with dark skin type, and in these cases it is generally advised to use lower energy density and longer pulse duration.
Take-Home Messages
- In case of hair loss, the search for possible causes and, if necessary, their treatment is inevitable.
- The most effective method to “re-grow” hairless or heavily thinned areas of the scalp is autologous hair transplantation for the treatment of receding hairline or “male pattern baldness”.
- Unwanted hair growth is one of the most common disturbing changes in external appearance, especially in women.
- In case of hirsutism, always arrange for endocrinological and gynecological clarification of a PCO syndrome.
- Currently, the most proven method with satisfactory hair reduction is the regularly repeated treatment with laser/IPL systems by dermatologists, in cosmetic institutes or with handy devices for independent use.
Literature:
- Gressenberger, et al: PRP for AGA: Randomized Placebo controlled Pilot Study. Acta Derm Venereol 2020; 100: adv00247.
- Darwin E, et al: Low-level laser therapy for the treatment of androgenic alopecia: a review. Lasers Med Sci 2018; 33: 425-434.
- https://youtu.be/moX643sIl2o
- Uslu A, Sürücü A, Korkmaz MA, Uygur F: Acquired Localized Hypertrichosis Following Pressure Garment and/or Silicone Therapy in Burn Patients. Ann Plast Surg 2019 Feb; 82(2): 158-161.
- Kopera D, Wehr E, Obermayer-Pietsch B: Endocrinology of hirsutism. Int J Trichology 2010; 2: 30-35.
- Barth JH, Catalan J, Cherry CA, Day A: Psychological morbidity in women referred for treatment of hirsutism. J Psychosom Res 1993; 37: 615-619.
- Campos VB, Dierickx C, Farinelli WA, Lin TD: Hair removal with an 800-nm pulsed diode laser. J Am Acad Dermatol 2000; 43: 442-447.
- Dierickx CC, Grossman MC, Farinelli WA, Anderson RR: Damage to hair follicles by normal-mode ruby laser. Arch Dermatol 1998; 134: 837-842.
- Finkel B, Eliezri YD, Waldman A, Slatkine M: Pulsed alexandrite laser technology for non-invasive hair removal. J Clin Laser Med Surg 1997; 15: 225-229.
- Kopera D: Hair Reduction: 48 Months of Experience with 800-nm Diode Laser. J Cosmet Las Ther 2003; 1-4.
- Kopera D: Systemic, topical, physical: modern options for hair removal. Kosmet Med 2004; 25: 14-17.
- Anderson RR, Parish JA.: Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science 1983; 220: 524-527.
DERMATOLOGY PRACTICE 2021; 31(4): 5-7