Stress incontinence and overactive bladder affect the sexual experience of affected women. Depression and anxiety disorders are often associated with incontinence. Conservative and surgical incontinence therapies can improve patients’ sexual experience. The empathic medical conversation is central to the care of female patients. If the patient is suitably motivated, referral to a sexual medicine consultation is a very sensible measure.
Suffering from incontinence and sexuality problems is a double taboo that does not stop at any age. Up to 23% of women suffer from urinary incontinence, and the figures for sexual problems during life are 30% [1]. It is not easy for physicians to address these potential problem areas, and only about 17% of patients report them on their own. Depending on the form of incontinence, stress incontinence (and/or bladder prolapse) results in loss of urine during penetration, while overactive bladder (OAB) results in loss of urine during arousal or orgasm. Women with stress incontinence are generally significantly more satisfied with their sexuality (79.4% satisfied) than women with OAB (only 31.7% satisfied). Effective incontinence therapies positively change sexual desire, sexual experience and psychological well-being.
Sexuality and brain circuits
The extent to which urine odor – or just the fear of it – affects sex life is not clear. It is known that odors are closely related to feelings, evoke conscious and unconscious memories, and influence sexual behavior. Incontinence resp. The urine odor and the fear of urine loss influence these control circuits in the patient and the partner, respectively. of the partner unfavorable. The nose and associated brain circuits are particularly sensitive immediately before ovulation, on the one hand to various types of odors and on the other hand to the largely unconscious effects of pheromones, the signaling substances that humans and animals emit through the skin and sweat glands [2–4]. As early as 1897, Wilhelm Fliess, an acquaintance of Sigmund Freud, published a book entitled “Die Beziehungen zwischen Nase und weiblichen Geschlechtsorganen: Presented in their Biological Significance”.
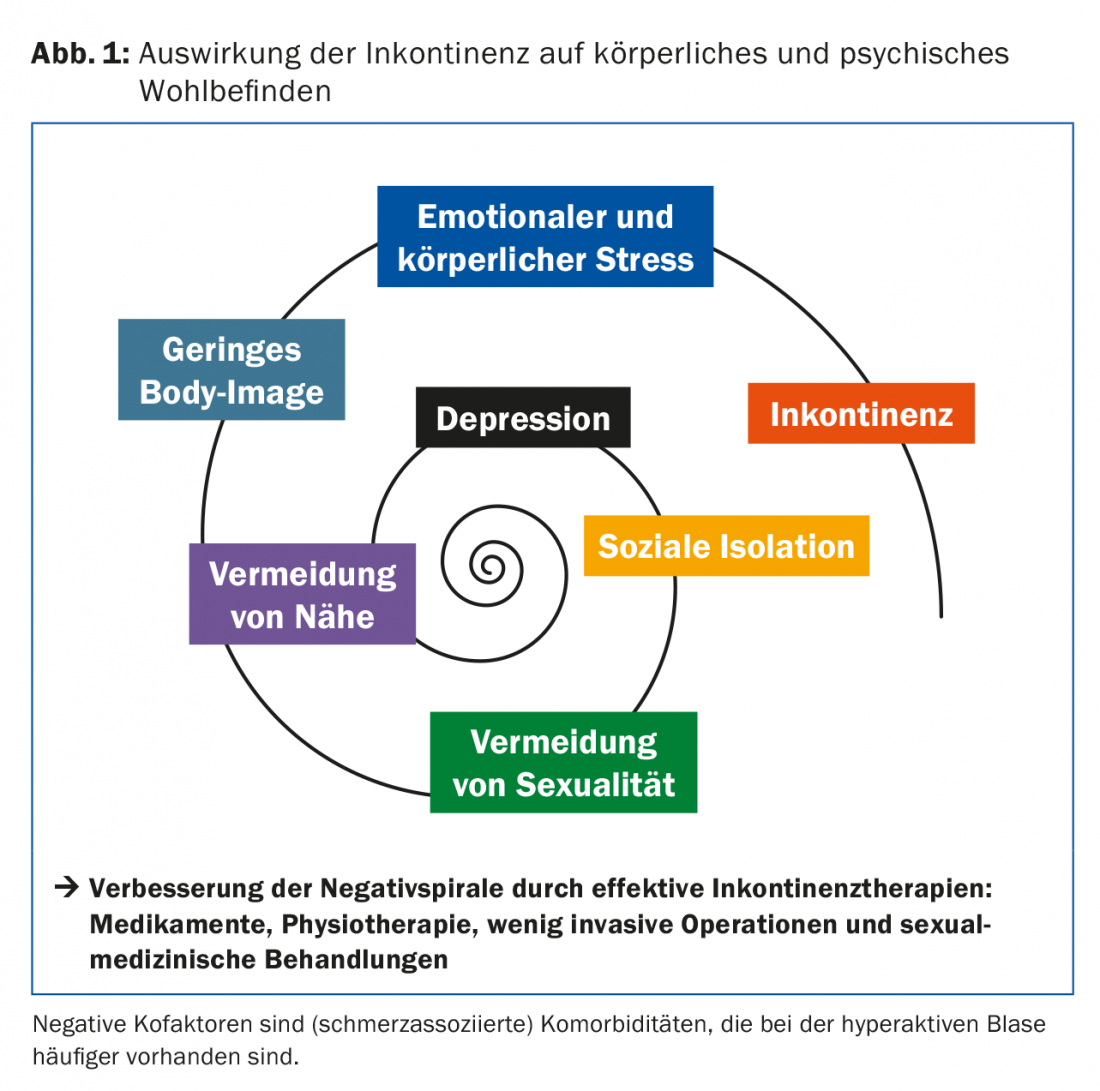
Out of shame of smelling unpleasant or even disgust with themselves, incontinent patients avoid situations that could lead to intimate contact. The fear of losing urine during the sexual act leads to tension and decreased satisfaction. However, this fear leads not only to avoidance of sexual contact, but in a broader sense also to disruption of the relationship and the basic psychosocial need for closeness. This negative spiral can ultimately affect very different areas of life (Fig. 1).
Prevalence of urine leakage during sexual intercourse.
Figures on the frequency of urine leakage during sexual intercourse vary. There is a high association between urge complaints and various sexual problems. For example, in a Northern European survey, 15-17% of young women in the 22-34 age group reported suffering from bladder symptoms such as frequent urination or urgency (corresponding to OAB). 25% reported a symptom associated with decreased sexual experience, such as lack of desire or arousal, infrequent or no orgasm, or dyspareunia (pain during intercourse). These figures were significantly higher in urinary incontinent women: 59% reported no longer having regular sexual intercourse because of incontinence, 25% did not experience orgasm, and 23% complained of urine leakage during intercourse [5]. The percentage for anorgasmia is comparable to that in healthy women without urogynecologic problems (20-30%) [6]. It is also worth mentioning a 2012 electronic anonymized survey in a group of 480 urogynecologic patients that confirmed the relatively high proportion of coital incontinence: 60% of women answered in the affirmative to the question about urine leakage during intercourse [7].
The FSFI score (Female Sexual Function Index) in premenopausal women is inversely proportional to the number of incontinence pads used per day [8]: All parameters are significantly lower in women with incontinence vs. continent women, only in the assessment of pain resp. Dyspareunia, no difference was found. Incontinent women generally feel less sexually attractive, if only because of the need to wear pads to bed.
Interestingly, this behaves somewhat differently in postmenopausal women: They remain sexually active despite incontinence, comparable to the group of continent women. A possible reason could be found in a more consolidated body image of the older women [9]. In general, sexual activity decreases with age, but depending on surveys and the presence of a partner, 25-50% of 70-year-old women are sexually active. This must be considered when choosing surgical treatment for incontinence, if necessary. Older women describe a slowing of physical reactions and reduction in intensity with the aging process, but this is accompanied by higher emotionality.
Comorbidities
Incontinence is often associated with mental illness. Depression is 2.5 times more common in incontinent women, and most common in OAB. In general, women with OAB are more affected in psychometric parameters than women with stress incontinence, because in stress incontinence events are more predictable and loss of control is lower [10]. Anxiety disorders are also significantly more common in incontinent women than in the normal population (3.5-fold increase).
Research on the associations between incontinence and psychological or psychosomatic disorders may be complicated for two reasons: first, in retrospective surveys, 18-62% of women report no recollection of the event following abuse [11], and second, the sensorimotor cortex in the female genital area (homunculus) is significantly sparsely mapped after abuse, as MRI studies showed [12]. Women with a history of sexual abuse appear to have an increased incidence of urinary incontinence, specifically OAB. On the other hand, women with OAB often have a difficult relationship with sexuality and avoid sexual contact.
There is also a link between chronic lower abdominal pain and sexual dysfunction. Thus, in addition to OAB, urge complaints during coitus, bladder pain syndrome/interstitial cystitis, suprapubic pain, vulvodynia, and even lichen sclerosus are associated with sexual abuse. Common to all these diseases is the unexplained pathogenesis. Possible hypotheses include neuropathological and neuroimmunological mechanisms leading to the release of nociceptive substances such as substance P, histamine, calcitonin gene-related peptide, and glutamate.
Does sexual experience improve with incontinence therapy?
There is good evidence that sexual experience improves with conservative and/or surgical incontinence therapies. Pelvic floor physical therapy not only reduces stress incontinence, but also significantly improves all domains of FSFI, including sexual pleasure and orgasmic ability, with few side effects [13]. For the surgical options for the treatment of stress incontinence, many studies have shown that coital incontinence is significantly improved after insertion of an incontinence sling, especially if no other sexual dysfunction was present prior to surgery. However, it should be borne in mind that, depending on the incontinence loop or access route (retropubic or transobturator), de novo dyspareunia occurs in up to 10% of patients. If the history and clinic are consistent, band splitting should be discussed with the patient in these cases, which is most likely to resolve the de novo dyspareunia [14].
But not only physiotherapy and surgery improve the sexual experience. Especially for urge incontinence, there are drug therapies (local estrogens, anticholinergics, b3 agonists, and botulinum toxin) that favorably modify incontinence. Local estrogens, as a simple and effective therapy, improve not only urge symptoms and incontinence, but also other symptoms of menopause such as burning, dryness, nocturia and dysuria [15]. In premenopausal patients, there are no real evidence-based indications for the application of local estrogens.
Anticholinergics and electrical stimulation have also been shown to improve sexuality in women with OAB [16,17]. For more invasive therapeutic modalities such as neurostimulation for the treatment of OAB, data also show a benefit for sexuality [18]. For the intravesical injection of botulinum toxin, a beneficial effect on sexuality can currently only be suspected due to the lack of data [19].
For incontinence-related sexual problems, empathic medical discussion is central, in addition to effective treatment of incontinence. If the patient is motivated, referral to a sexual medicine consultation is the best “medicine.” Patients with OAB, in particular, may have a complex sexual disorder that is challenging to treat and requires the involvement of a sex therapist.
Literature:
- Beutel ME, et al: Prevalence of urinary incontinence in the German population. Der Urologe 2005; 44: 232-238.
- Savic IH, et al: Smelling of odorous sex hormone-like compounds causes sex-differentiated hypothalamic activations in humans. Neuron 2001; 31(4): 661-668.
- Dreher JC, et al: Menstrual cycle phase modulates reward-related neural function in women. Proc Natl Acad Sc USA 2007; 104: 2465-2470.
- Gangestad SW, Thornhill R: Menstrual cycle variation in women’s preferences for the scent of symmetrical men. Proc Biol Sci 1998; 265: 927-933.
- Bodden-Heidrich R, et al: Psychosomatic aspects of urinary incontinence. Arch Gynecol Obstet 1999; 262(3-4): 151-158.
- Ishak WW, et al: Disorders of orgasm in women: a literature review of etiology and current treatments. J Sex Med 2010; 7(10): 3254-3268.
- Jha S, Strelley K, Radley S: Incontinence during intercourse: myths unraveled. Int Urogynecol J 2012; 23(5): 633-637.
- Aslan G, et al: Sexual function in women with urinary incontinence. Int J Impot Res 2005: 17: 231-238.
- Tannenbaum C, Corcos J, Assalian P: The relationship between sexual activity and urinary incontinence in older women. J Am Geriatr Soc 2006; 54: 1220-1224.
- Abrams P, et al: OAB significantly affects quality of life. Am J Manag Care 2000; 6(11 Suppl): S580-590.
- Leeners B, et al: Effect of childhood sexual abuse on gynecologic care as an adult. Psychosomatics 2007; 48(5): 385-393.
- Heim CM, et al: Decreased cortical representation of genital somatosensory field after childhood sexual abuse. Am J Psychiatry 2013; 170: 616-623.
- Serati M, et al: Benefit of Pelvic Floor Muscle Therapy in Improving sexual Function in Women with Stress Urinary Incontinence. A pretest-posttest intervention study. J Sex Marital Therapy 2015; 41(3): 254-261.
- Kuhn A, et al: Sexual function after suburethral sling removal for dyspareunia. Surg Endosc 2009; 23(4): 765-768.
- Nappi RE, et al: The CLOSER (Clarifying Vaginal Atrophy’s Impact on Sex and Relationships) Survey: Implications of Vaginal Discomfort in Postmenopausal Women and in Male Partners. J Sex Med 2013; 10: 2232-2241.
- Hajebrahimi S, et al: Tolterodine Immediate Release Improves Sexual Function in Women with Overactive Bladder. J Sex Med 2008; 5(12): 2880-2885.
- Aydin S, et al: Effect of vaginal electrical stimulation on Female Sexual Functions: a randomized study. J Sex Med 2015; 12(2): 463-469.
- Signorello D, et al: Impact of Sacral Neuromodulation on Female Sexual Function and its Correlation with clinical Outcome and Quality of Life Indexes: a monocentric experience. J Sex Med 2011; 8(4): 1147-1155.
- Proietti S, et al: Overactive bladder and sexual function: a nightmare couple. BJU Int 2012; 110(7): 921-924.
HAUSARZT PRAXIS 2016; 11(2): 10-12











