Many patients who suffer from urinary incontinence only mention these complaints to their family doctor in passing – or not at all – out of shame. There are certainly ways to treat or at least improve incontinence. An overview of examinations and therapy options for elderly patients was given at the KHM by Dr. med. Cristina Mitrache, Chief Physician Reha Chrischona, Bettingen.
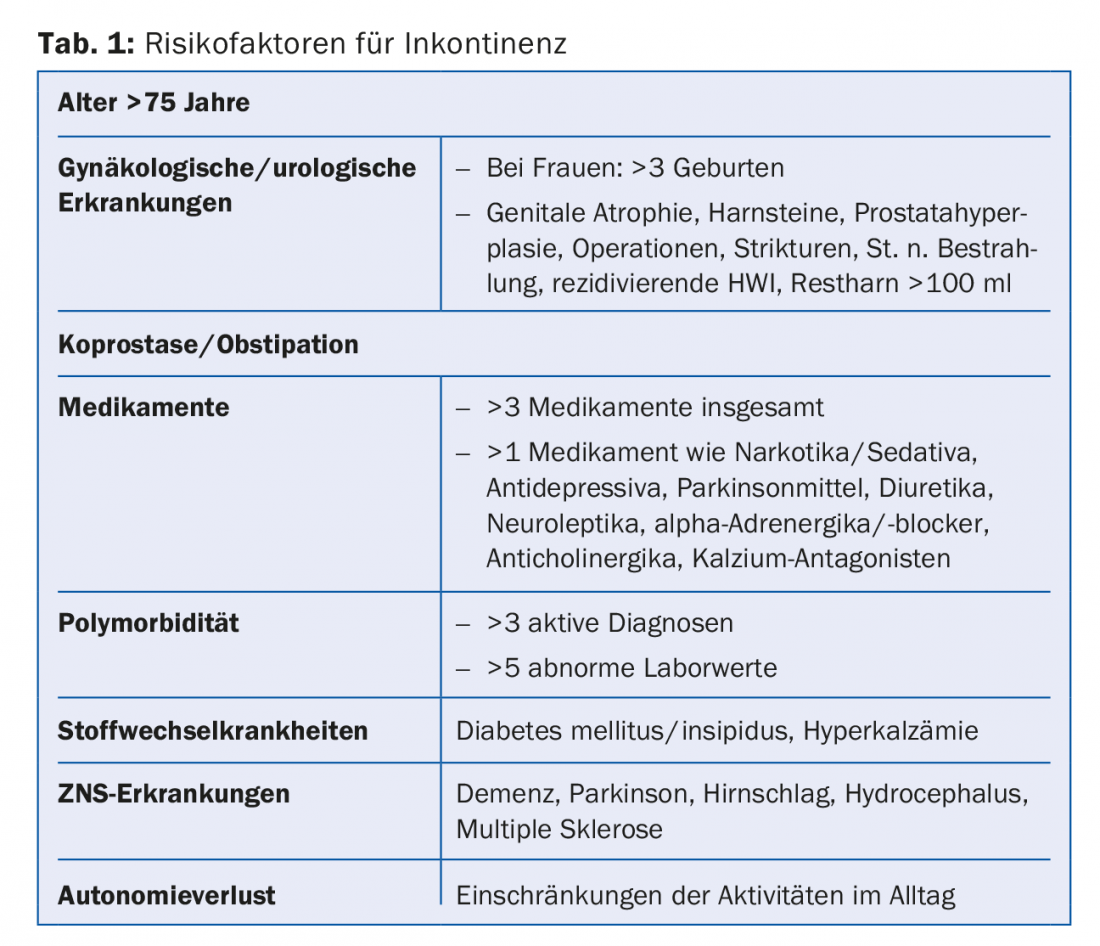
The prevalence of urinary incontinence correlates with age, cognition, and mobility: among 65-year-olds, 26% have incontinence; among 95-year-olds, 73% have incontinence; 76% of all patients with dementia are incontinent, and among bedridden elderly, 82 (Tab.1). The speaker used case studies to explain the various problems that can arise around micturition, especially in the elderly.
Mr. N., 73 years, bladder voiding disorder and urge symptoms
Mr. N. lives alone at home with the support of Spitex. He has severe COPD, coronary artery disease with heart failure, sarcopenia, and polyneuropathy. After prostate laser vaporization, he suffers from urge symptoms. He recently fell at night, while going to the bathroom, and suffered a contusion of the hip. He is now mobile again with pain medication (tramadol and paracetamol, Zaldiar®, 3×/d). He also takes the following medications: Exforge® 160/10 mg, Aspirin® 100 mg, Sortis® 40 mg, Detrusitol® 8 mg, and Saroten® 50 mg, and he inhales with Symbicort® and Spiriva®. Now he complains of great fatigue and increased urge to urinate, he has to get up four to five times a night with near falls. On examination, bladder emptying disorder (bladder contains 400 ml of urine without urge to urinate) and constipation are noticeable.
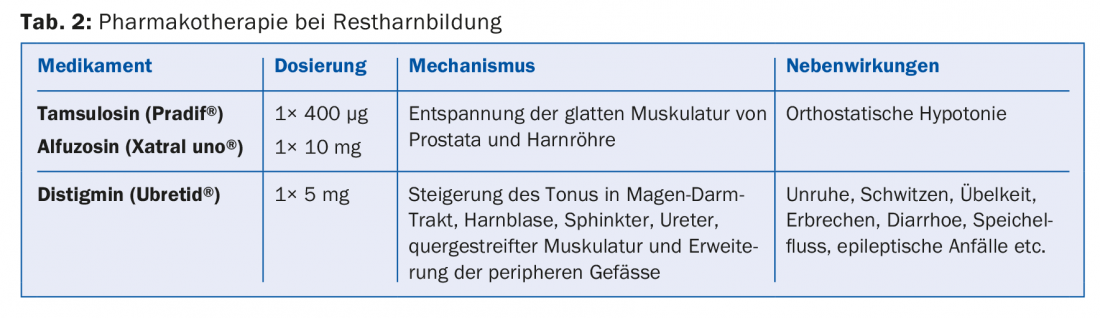
The innervation of the bladder is extremely complex: the parasympathetic pelvic nerve (neurotransmitter: acetylcholine), the sympathetic hypogastric nerve (norepinephrine) and the somatic pudendal nerve (acetylcholine) are involved in the control of micturition. The physiological capacity of the bladder is about 500 ml, urge to urinate occurs from 200 ml. Anticholinergics relax the detrusor, alpha-blockers relax the internal sphincter. Pharmacotherapy for residual urine is also based on this (Tab. 2) . Residual urine is defined as more than 60 ml of urine remaining in the bladder after micturition. “In the elderly, it is important to keep in mind that constipation can exacerbate bladder emptying dysfunction and lead to confusion,” the speaker emphasized. For this reason, stimulant laxatives and additional emollients are appropriate for constipation. In Mr. N, the dosage of Exforge® was lowered, Detrusitol® and Saroten® were dropped, and Pradif® (400 µg/1×/d) and Laxoberon® (10 drops in the evening) were prescribed instead. This was accompanied by non-drug measures to improve his situation: support stockings, meal service, orthotics and more frequent visits to Spitex.
Mrs. W., 79 years, recurrent loss of urine
Mrs. W. has been living alone at home since the death of her husband. She has type 2 diabetes mellitus and mild dementia. For some time she has been losing small amounts of urine; before that she feels urge to urinate each time, but not imperatively. She has also felt like “sitting on a pillow” for about six months.
In addition to the specific urogynecological history and the general history, the diagnosis of urinary incontinence always includes a local examination, a brief neuro status and a urine examination. “Sonography of the kidney and urinary tract, including residual urine determination, and a micturition log are also very helpful,” Dr. Mitrache said. In Mrs. W, physical examination revealed complete synechiae of the labiae, and sonography showed 600 ml of residual urine and retrograde congestion. “The patient had been to her primary care physician for a checkup at least once a month in the months before,” the speaker said, “without the local finding being detected. This case also shows how much body awareness can change with age and especially with the onset of dementia.” After surgical repair of the synechiae, Mrs. W. was continent again.
Mrs. S., 83 years, imperative urination
Mrs. S. lives independently at home. She has had recurrent imperative urination for about two years, resulting in hourly micturitions. When she’s out of the house, she’s always on the lookout for public restrooms, and she needs three to four deposits per day. During the night, she has to get up three times to go to the bathroom. Two years ago, Mrs. S. received a right hip replacement; at that time, she had an indwelling catheter and subsequently suffered from urinary tract infections (UTI) twice. Since then, the urge problem has developed. Mrs. S. has already taken SpasmoUrgenin® and Detrusitol® without success. Other diagnoses include hypertensive heart disease, obesity, gonarthrosis bilaterally, right hip TP for coxarthrosis, mastectomy bilaterally after breast carcinoma 20 years ago, and chronic lymphedema. Local examination reveals atrophy of the genital mucosa. The cough test is negative, and there is no residual urine. Urinalysis reveals a UTI with E. coli >100,000/ml.
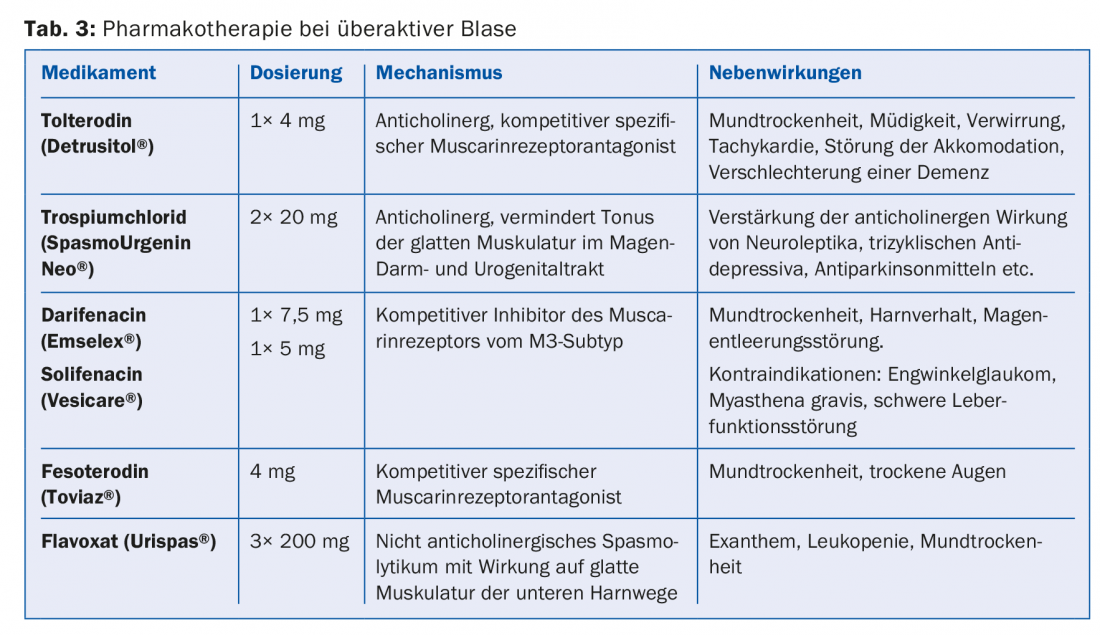
Urinary incontinence and hyperactive bladder often have several causes. The sensible combination of therapies improves the success of treatment. It is also important that primary treatment is followed by long-term prophylaxis. First, Mrs. S’s UTI was treated with Noroxin (2× 400 mg/5 d). Other therapeutic approaches included adequate drinking (2-2.5 l/d), local estrogenization of the genital mucosa with colpotrophins, lymphatic drainage, and compression stockings. Ms. S. also kept a micturition log for three days. In it, she recorded over 24 hours when she went to the toilet, how much water she was able to dissolve in each case, whether there was any involuntary loss of urine and when she drank how much. The protocol showed that Mrs. S. had to go to the toilet almost every hour and lost urine each time before that. In this situation, pharmacotherapy of hyperactive bladder is recommended (Tab. 3), therefore, after controlling the intraocular pressure, therapy with Toviaz® was started. In addition, Ms. S began bladder training. “The goal of bladder training is to increase the intervals between toilet visits,” the speaker explained. “It is suitable for people with preserved cognitive function and can significantly reduce incontinence episodes.” With micturition training, when the urge to urinate comes, the patient waits until the urge subsides and only then goes to the bathroom. During the urge, the patient remains seated and tenses the pelvic floor. The emptying intervals are gradually extended by approx. 20 minutes per week. After two months, Ms. S. again kept a micturition log, which turned out to be significantly better: she had to go to the toilet less frequently and only lost small amounts of urine once or twice a day.
When extended diagnostics?
Dr. Mitrache recommended extended diagnostics if conservative therapy does not lead to satisfactory treatment success within three months. In such cases, urodynamic clarification is useful. Further investigations may be necessary earlier if the diagnosis is uncertain (discrepancy between symptoms and clinical examination), there is an indication for surgical intervention (e.g., prostatic hyperplasia), hematuria without infection, or comorbidities such as abnormalities of the prostate, recurrent complicated UTI, prolapse, or overflow bladder.
Source: 19th Continuing Education Conference of the College of Family Medicine (KHM), June 22-23, 2017, Lucerne.
HAUSARZT PRAXIS 2017; 12(8): 53-55











