Synovial cysts occur primarily in the joints of the extremities and much less frequently in the spinal canal region. The in-traspinal synovial cysts, like other intraspinal space-occupying lesions, can cause radicular symptoms, which may be unilateral or, in the case of large cysts, bilateral. The main age of manifestation is in the 6. and 7th decade of life.
Clinically, it is not possible to differentiate between disc herniation with radiculopathy or a synovial cyst as the cause of the symptomatology. In principle, any other space-occupying intraspinal change can lead to radicular symptoms [1], but other tumorous entities or a spinal or recess stenosis in degenerative change must be evaluated differently in the time course of the development of symptoms. The main age of manifestation is expected primarily in the 6th to 7th decade of life, preferentially in the L4/5 segment [2,3] and a slight predominance in females. If the cysts are located in the cervical or thoracic portion of the spine, myelopathy may result.
Conservative measures in therapy are not very promising, surgical cyst removal is considered the method of choice. Increasingly, CT-guided minimally invasive treatment of spinal synovial cysts is also being reported, with a published failure rate of 50 to 100%, especially by surgical specialties, is viewed critically [3,4]. In contrast, the surgical success rate is reported to be 91%.
Computed tomography is difficult to determine the exact extent of the intraspinal cyst: Cerebrospinal fluid and synovial fluid of the cyst are nearly isodense, and the cyst wall is usually not differentiable. The sensitivity of CT for cyst detection is 70%, and over 90% in MRI [2]. CT myelography as an invasive diagnostic procedure has also clearly moved into the background.
Magnetic resonance imaging is the best method to detect synovial cysts. The multiplanar visualization of the pathological change and the high soft tissue contrast with delineation of the delicate cyst wall and thus the possibility to determine the exact size and extent of the cyst as well as to delineate the altered nerve roots are unbeatable advantages of the procedure.
Case study
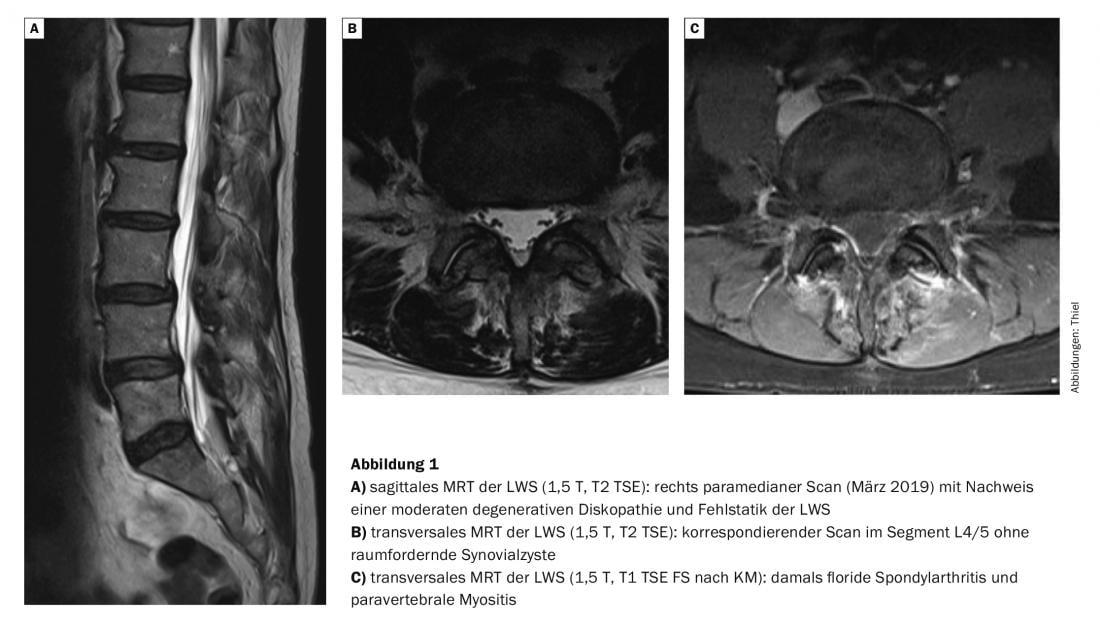
Perhaps you can still remember or browse through one of the last issues: In the case report on vertebral myositis, we also reported on a patient in her early 60s who had developed lumbar spondylarthritis and myositis (Fig. 1). After anti-inflammatory therapy, she was doing stably well for about six months. Then right-sided lumboischialgia reappeared, corresponding to an L4 symptomatology. 2 CT-guided PRTs were performed with good success. After a four-week vacation in South America with associated physical exertion, CT-guided pain therapy should again be used for recurrent symptoms. Prior to this, an MRI of the lumbar spine was obtained to rule out causes other than the known discopathy (Fig.2). A large intraspinal lumbar synovial cyst was diagnosed on the right side in segment L4/5, which not only caused a significant impression of the dural tube but also led to recessal and neuroforaminal stenosis and was the cause of the acute symptomatology.
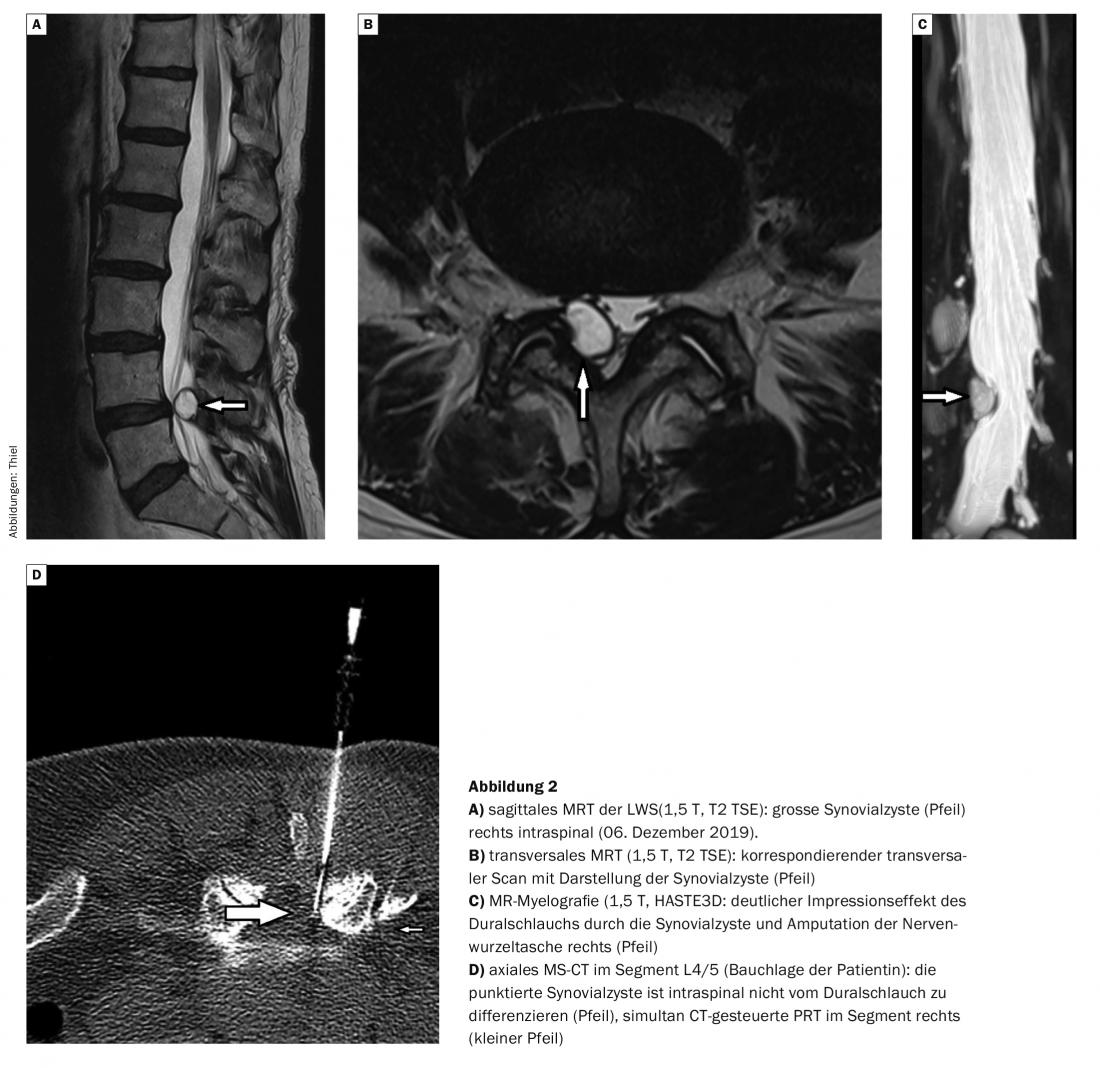
The patient initially decided against surgical treatment. An outpatient CT-guided puncture of the cyst was performed. With the very viscous synovial fluid, only little material could be aspirated. Nevertheless, the patient felt a complete reduction in pain immediately after puncture, but this only lasted a few days. Given the size of the cyst, 1.2 × 0.8 cm on transverse scan, expansion with NaCl and destruction of the cyst, as is possible minimally invasively for smaller cysts, was initially not performed.
MR-tomographic cyst control one week after puncture showed only minimal size reduction. A repeat outpatient CT-guided puncture under local anesthesia was performed. In this case, with the needle in an intracystic position, a slight dilatation and irrigation with 1 ml Volon A was performed first, followed by aspiration of the fluid. Significantly better aspiration of the synovial fluid diluted by the liquid cortisone was seen. The irrigation was repeated in the same manner and again aspirated. Immediately after manipulation, the patient was symptom-free. A size check of the cyst about 5 weeks after the second puncture showed a significant reduction of the synovial cyst with a decrease in the impression of the dural tube and the recessal stenosis on the right side with a persistent complete regression of symptoms (Fig. 3).

Case casuistry shows that surgical treatment of a symptomatic synovial cyst is not always mandatory. If no neurological complication with paresis results, therapy with cyst puncture can certainly be attempted, whereby intracystic cortisone application has obviously brought a clear advantage.
Take-Home Messages
- Intraspinal synovial cysts may cause radicular symptoms, depending on size and extension.
- The main age of manifestation is in the 6th and 7th decades of life, with a slight predominance in females.
- The preferred site of synovial cysts is the L4/5 segment, and magnetic resonance imaging is undoubtedly the imaging method of choice for detecting cysts.
- According to current knowledge, surgical resection of cysts has a higher success rate of therapy than puncture procedures.
Literature:
- Jeong GK, Bendo JA: Lumbar intervertebral disc cyst as a cause of radiculopathy. Spine J 2003; 3(3): 242-246.
- Boviatsis EJ, et al: Spinal synovial cysts: pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J 2008; 17(6): 831-837.
- Rahim T, Vinas-Rios JM: Lumbar synovial cysts: literature review and original long-term results after microsurgical. Orthopaedic 2019; 48(10): 849-857.
- Epstein NE, Baisden J: The diagnosis and management of synovial cysts: efficacy of surgery versus cyst aspiration. Surg Neurol Int 2012; 3(Suppl 3): S157-166. Jeong GK, Bendo JA: Lumbar intervertebral disc cyst as a cause of radiculopathy. Spine J 2003; 3(3): 242-246.
- Reddy P, Satyanarayana S, Nanda A: Synovial cyst of lumbar spine presenting as disc disease: a case report and review of literature. J La State Med Soc 2000; 152(11): 563-536.
FAMILY PRACTICE 2020; 15(6): 34-36











