A colloquium at the University Hospital Zurich was devoted to the broad clinical spectrum of viral hepatitis. It addressed the issue of screening and special risk groups, as well as the end state of chronic hepatopathy: liver cirrhosis. The modes of transmission of hepatitis E – an infection that occurs only sporadically in our latitudes and generally has few complications – were also discussed.
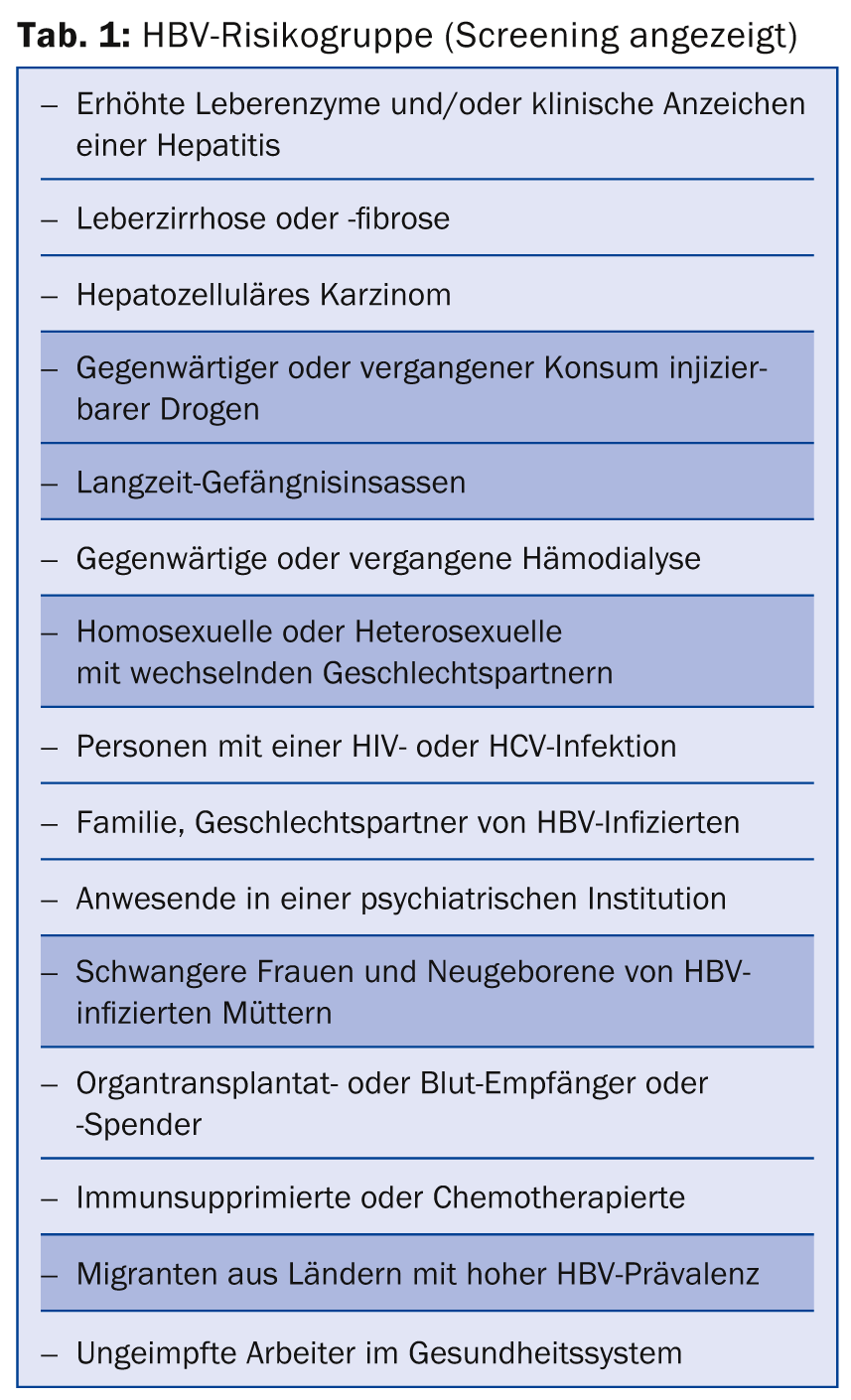
PD Tilman Gerlach, MD, Munich, spoke about the need for screening and surveillance in viral hepatitis. In Switzerland, a country with low HBs-Ag (hepatitis B surface antigen) prevalence (<2%), hepatitis B virus (HBV) is transmitted primarily sexually and less frequently vertically from mother to child. Contrary to media attention, the HBV infection rate, with an estimated 14 million infected persons in Europe, is significantly higher than that of HIV (less than 2 million). Many of them are not aware of the infection. “Nevertheless, it has to be said: we have a very effective vaccination that has led and continues to lead to a decrease in prevalence in Switzerland,” he said. In particular, countries such as Turkey and, to some extent, Romania, Italy, Spain, and Germany, for example, have significantly higher prevalence figures, so ethnicity should be considered in screening efforts in any case. Migration is a decisive factor. For family practice, it has been shown that with a detailed risk history – including promiscuity and migration background – plus laboratory (alanine aminotransferase, ALT), almost two-thirds of patients can be correctly classified as infected. A complete definition of the HBV risk group for which screening is appropriate is shown in Table 1. Regarding serology, anti-HBc indicates contact with HBV, and HBs-Ag indicates acute infectivity.
Hepatitis C
“Overall in Europe, there are about 9 million people infected with the hepatitis C virus (HCV). The prevalence figures here are unfortunately less declining than for HBV, even in Switzerland, because there is no vaccination,” explained Dr. Gerlach. Italy, particularly the south, is considered an “HCV country,” where drug use is probably one of the most important factors (as with HCV prevalence overall: both injectable drugs and intranasal cocaine). An increase in liver cancer (hepatocellular carcinoma, HCC) mortality is currently being observed in the U.S., now exceeding that of all other cancers. This is because a good fifth of chronic HCV patients develop liver cirrhosis after 20 years, which in turn increases the risk of HCC. The Americans are therefore currently stepping up their screening efforts. In addition to drug use, risk factors for HCV that necessitate screening include long prison sentences, blood transfusions outside the EU or before 1992, and receipt of concentrated coagulation factors before 1987 for hemophilia. However, this also requires better awareness in the general population.
“Individuals infected with HBV and HCV should be identified as early as possible with intensive screening efforts,” the speaker concluded. “This is best done by history, elevated ALT levels, and demographic factors. Prospective hepatitis screening (anti-HBc, anti-HCV) is indicated in those considered at risk for medical, behavioral, occupational, or demographic reasons.” HBV vaccination completion should be performed and followed up on all patients as standard practice. The new antiviral therapies help those who are already infected; cooperation with the hepatologist is advisable here.
Hepatitis E – just a travel disease?
According to PD Dr. med. Thomas Kuntzen, Zurich, the genotype of hepatitis E (HEV) that mainly occurs in our latitudes (genotype 3) usually has a clinically mild to asymptomatic course and is self-limiting. Nevertheless, the virus should not be forgotten, as it can become chronic in immunosuppressed individuals, for example (with potential cirrhosis of the liver). “There are a total of four genotypes of HEV in humans: Genotypes 1 and 2, which are at risk for acute liver failure, are sometimes endemic in Central America, certain regions of Africa, and Southeast Asia, and are transmitted primarily fecal-orally via contaminated water. Pregnant women in particular are at risk for severe hepatitis with fatal outcomes. Genotype 3, which occurs sporadically in Europe and the USA, tends to take the zoonotic route of transmission (e.g., infectious raw meat). Genotype 4 occurs in China, for example, and also tends to be transmitted zoonotically,” explained Dr. Kuntzen.
For prevention of fecal-oral transmission, avoid drinking water and ice cubes of unknown quality, raw seafood, and unpeeled and uncooked vegetables or fruits in affected regions. The country’s own hygiene and, of course, wastewater management are also crucial. For zoonotic infection , avoid raw meat, especially in the hyperendemic regions of genotype 3 (Toulouse area). A vaccine is currently only available in China (Hecolin®). It protects effectively, but it is unknown when and if it will be accessible in Europe in the future.
Therapeutic data are very scarce and come mainly from single case reports and small series. Currently, ribavirin is thought to help with severe acute or chronic infections.
Cirrhosis of the liver
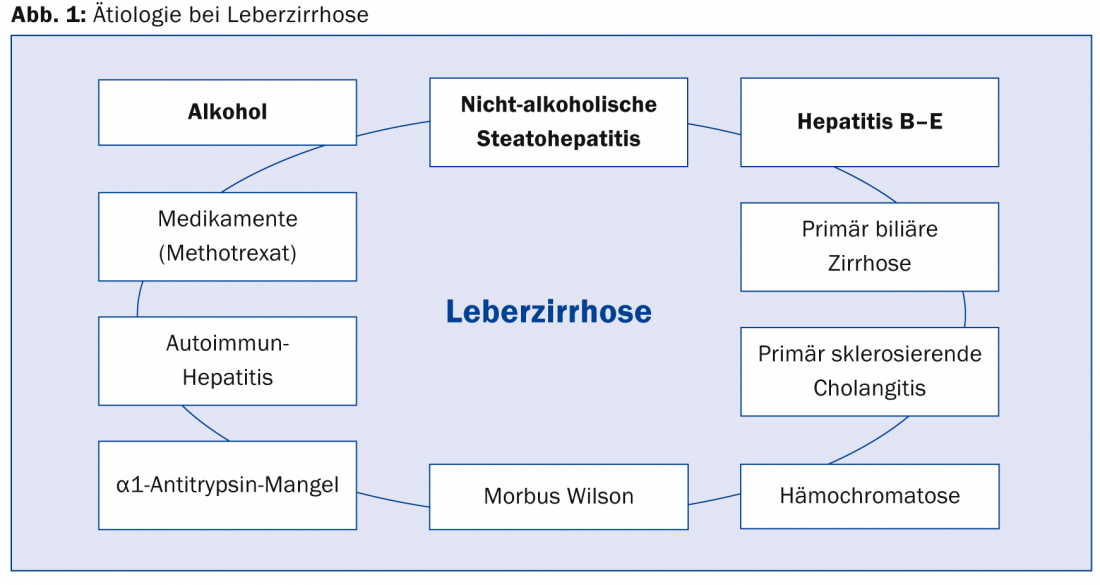
Finally, Joachim Mertens, MD, Zurich, gave an update on liver cirrhosis. This is the end state of chronic hepatopathy with remodeling of lobular architecture (connective tissue septa, functional portosystemic shunts, loss of functional hepatocellular mass). In terms of etiology, the “top 3” alcohol, hepatitis B to E and non-alcoholic steatohepatitis (fatty liver) play a major role (Fig. 1) . The clinical course of liver cirrhosis can sometimes lead to hepatic encephalopathy, portal hypertension (ascites, esophageal varices), or HCC.
Hepatic encephalopathy: Diagnosis should not be made by arterial measurement of blood ammonia. This is a poor parameter because there is no good correlation and high variability. Psychomotor tests are much more reliable (number connection test and Stroop test). Therapeutically, the reduction of NH3 absorption is clearly the focus (2-3 soft stools per day). Lactulose can help here. In addition, one should look for the trigger: Bleeding, infection, acute event, medication with benzodiazepines or opiates? A general protein reduction is not indicated.
Ascites: 30-50% of patients with cirrhosis develop ascites, it is a sign of decompensation. Therapy is via salt reduction and medication (spironolactone, torasemide). If ascites cannot be adequately treated diuretically, paracentesis, for example, may be considered.
Esophageal varices: 5-20% of cirrhotic patients develop varices. Screening endoscopy is indicated in all patients. If no varices are found, it should be repeated every two to three years. If small varices are found and liver function is good, endoscopy must be repeated after one year. Primary prophylaxis of life-threatening bleeding in large varices is given with propranolol or carvedilol. The goal is a 25% reduction in heart rate or a resting heart rate of about 55/min. The pulse should thus be well controlled.
HCC: The incidence of HCC in liver cirrhosis is high, 1-5% per year. Here, the screening examination should take place every six months by means of ultrasound.
Source: “What does the physician in practice need to know about viral hepatitis?”, Gastro-surgical Colloquium, December 11, 2014, Zurich.
HAUSARZT PRAXIS 2015; 10(2): 34-36